| | | | |
| Early, Late, PrEP, PEP | (Preprint) (meta analysis) | meta-analysis v114 | Vitamin D for COVID-19: real-time meta analysis of 144 studies |
| Details • 85% of 53 vitamin D treatment studies report positive effects. 27 studies show statistically significant improvements in isolation (21 for the most serious outcome). • Random effects meta-analysis with pooled effects using the most ser.. |
| Details Source PDF Early, Late, PrEP, PEP Early, Late, PrEP, PEP |
| Covid Analysis (Preprint) (meta analysis) |
| Vitamin D for COVID-19: real-time meta analysis of 144 studies |
• 85% of 53 vitamin D treatment studies report positive effects. 27 studies show statistically significant improvements in isolation (21 for the most serious outcome).• Random effects meta-analysis with pooled effects using the most serious outcome reported shows 81% [65‑90%] and 45% [37‑53%] improvement for early treatment and for all studies. Results are similar after restriction to 47 peer-reviewed studies: 84% [68‑92%] and 44% [35‑52%], and for the 31 mortality results: 79% [61‑88%] and 50% [34‑62%].• Statistically significant improvements are seen in treatment studies for mortality, ventilation, ICU admission, hospitalization, and cases.• Late stage treatment with calcifediol/calcitriol shows greater improvement compared to cholecalciferol: 78% [67‑85%] vs. 45% [24‑60%].• Sufficiency studies show a strong association between vitamin D sufficiency and outcomes. Meta analysis of the 91 studies with pooled effects using the most serious outcome reported shows 57% [50‑63%] improvement.• While many treatments have some level of efficacy, they do not replace vaccines and other measures to avoid infection. Only 11% of vitamin D treatment studies show zero events in the treatment arm.• Elimination of COVID-19 is a race against viral evolution. No treatment, vaccine, or intervention is 100% available and effective for all current and future variants. All practical, effective, and safe means should be used. Not doing so increases the risk of COVID-19 becoming endemic; and increases mortality, morbidity, and collateral damage.• All data to reproduce this paper and the sources are in the appendix. | Improvement | Studies | Authors | Patients | | Treatment RCTs | 53% [23‑72%] | 9 | 84 | 774 | | Treatment studies | 45% [37‑53%] | 53 | 529 | 66,371 | | Cholecalciferol treatment | 42% [32‑51%] | 44 | 418 | 58,390 | | Calcifediol/calcitriol treatment | 61% [30‑78%] | 9 | 111 | 7,981 | | Treatment mortality | 50% [34‑62%] | 31 | 283 | 12,599 | | Sufficiency studies | 57% [50‑63%] | 91 | 754 | 41,555 | 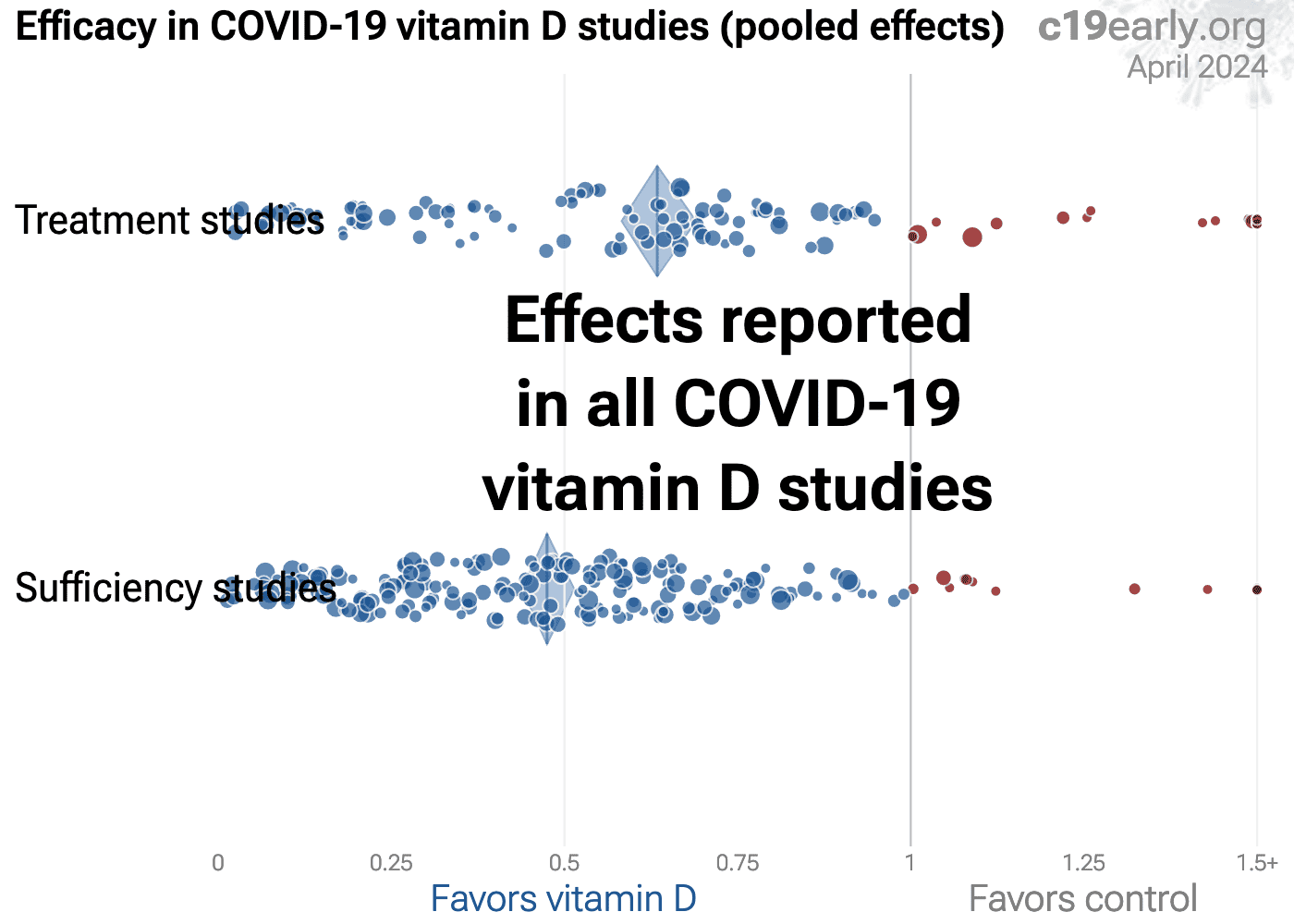 |
| Submit Corrections or Comments |
| Levels | Fatemi et al., Acute and Critical Care, doi:10.4266/acc.2021.00605 (Peer Reviewed) | death, ↓42.0%, p=0.07 | Association of vitamin D deficiency with COVID-19 severity and mortality in Iranian people: a prospective observational study |
| Details Prospective study of 248 hospitalized COVID+ patients in Iran with vitamin D levels measured in the previous year and again at admission, showing vitamin D status associated with severity and mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Fatemi et al., Acute and Critical Care, doi:10.4266/acc.2021.00605 (Peer Reviewed) |
| Association of vitamin D deficiency with COVID-19 severity and mortality in Iranian people: a prospective observational study |
Prospective study of 248 hospitalized COVID+ patients in Iran with vitamin D levels measured in the previous year and again at admission, showing vitamin D status associated with severity and mortality. 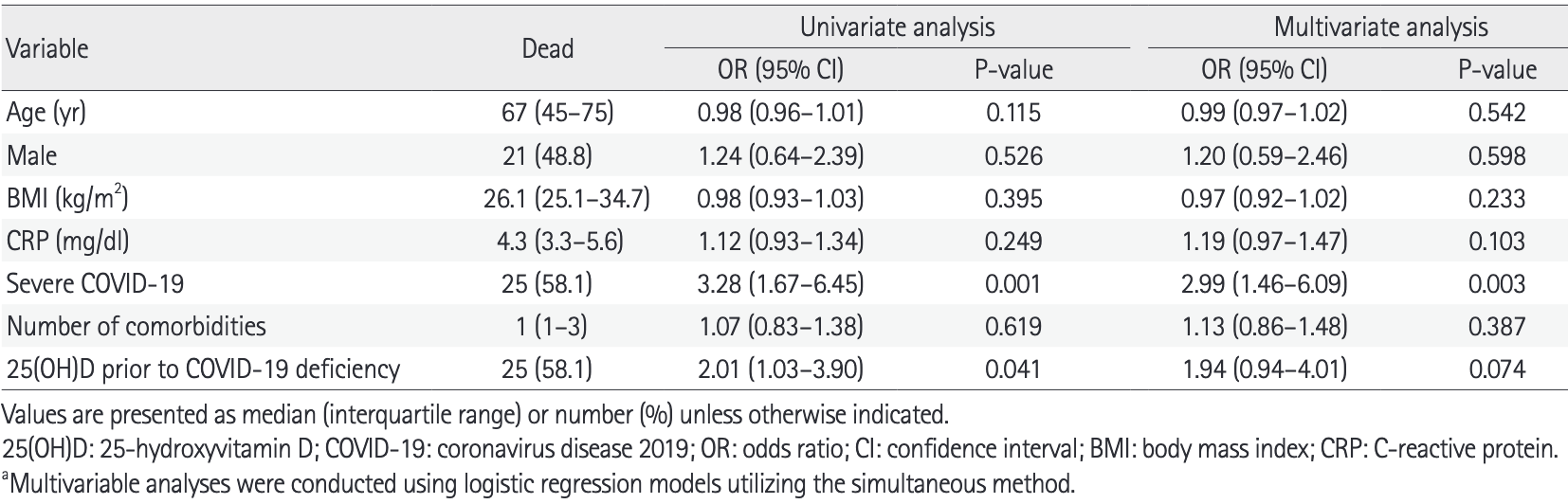 risk of death, 42.0% lower, RR 0.58, p = 0.07, high D levels 18 of 139 (12.9%), low D levels 25 of 109 (22.9%), OR converted to RR, vitamin D measured prior to COVID-19, multivariate. risk of death, 51.1% lower, RR 0.49, p = 0.02, high D levels 13 of 115 (11.3%), low D levels 30 of 133 (22.6%), OR converted to RR, vitamin D measured on admission, multivariate. risk of severe case, 37.9% lower, RR 0.62, p = 0.007, high D levels 38 of 139 (27.3%), low D levels 48 of 109 (44.0%), vitamin D measured prior to COVID-19. risk of severe case, 34.8% lower, RR 0.65, p = 0.02, high D levels 31 of 115 (27.0%), low D levels 55 of 133 (41.4%), vitamin D measured on admission. Fatemi et al., 11/30/2021, prospective, Iran, Middle East, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Kaur et al., Indian Journal of Clinical Practice, 32:6 (Peer Reviewed) | death, ↓89.8%, p<0.0001 | Correlation of Vitamin D Levels with COVID-19 Severity and Outcome |
| Details Prospective study of 81 hospitalized COVID+ patients in India, showing low vitamin D levels associated with COVID-19 severity and mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Kaur et al., Indian Journal of Clinical Practice, 32:6 (Peer Reviewed) |
| Correlation of Vitamin D Levels with COVID-19 Severity and Outcome |
Prospective study of 81 hospitalized COVID+ patients in India, showing low vitamin D levels associated with COVID-19 severity and mortality. 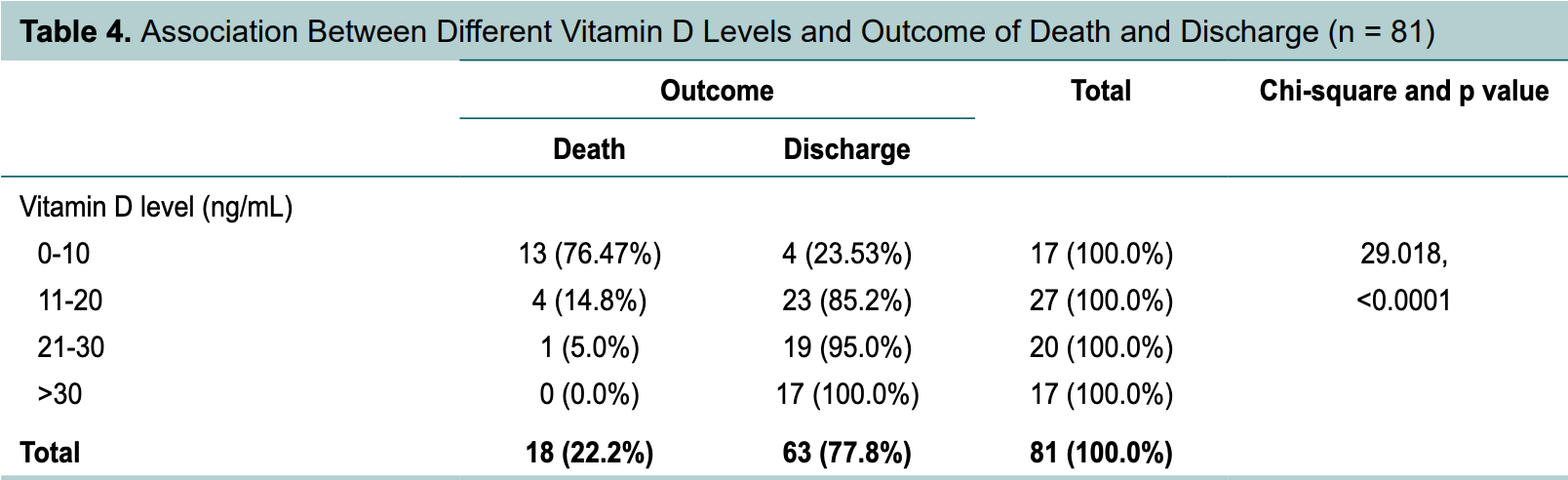 risk of death, 89.8% lower, RR 0.10, p < 0.001, high D levels (≥10ng/mL) 5 of 64 (7.8%), low D levels (<10ng/mL) 13 of 17 (76.5%). risk of mechanical ventilation, 90.3% lower, RR 0.10, p < 0.001, high D levels (≥10ng/mL) 4 of 64 (6.2%), low D levels (<10ng/mL) 11 of 17 (64.7%). Excluded in after exclusion results of meta analysis: unadjusted results with no group details. Kaur et al., 11/30/2021, prospective, India, South Asia, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Jenei et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.11.025 (Peer Reviewed) | COVID-19 mortality is associated with low Vitamin D levels in patients with risk factors and/or advanced age |
| Details Retrospective 257 hospitalized patients in Hungary, showing mortality associated with lower vitamin D levels for all patients, for patients >60, and for age-matched patients with risk factors or age >60. The non-age-matched analyses are c.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Jenei et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.11.025 (Peer Reviewed) |
| COVID-19 mortality is associated with low Vitamin D levels in patients with risk factors and/or advanced age |
Retrospective 257 hospitalized patients in Hungary, showing mortality associated with lower vitamin D levels for all patients, for patients >60, and for age-matched patients with risk factors or age >60. The non-age-matched analyses are confounded by age, with elderly patients more likely to have lower vitamin D levels. 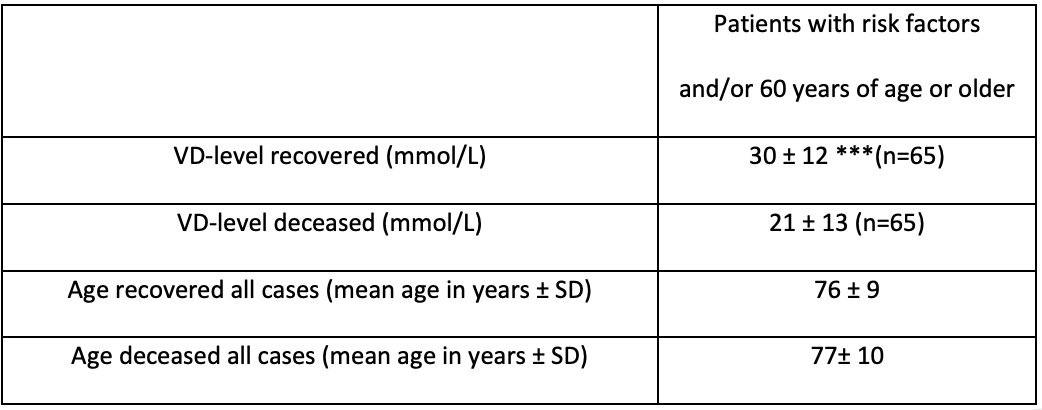 Jenei et al., 11/24/2021, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Levels | Sacristán et al., Transplantation Proceedings, doi:10.1016/j.transproceed.2021.08.060 (Peer Reviewed) | Risk of severe COVID-19 infection in kidney transplant recipients |
| Details Retrospective 63 COVID+ kidney transplant recipients, showing significantly lower vitamin D levels before infection in patients requiring ICU admission. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Sacristán et al., Transplantation Proceedings, doi:10.1016/j.transproceed.2021.08.060 (Peer Reviewed) |
| Risk of severe COVID-19 infection in kidney transplant recipients |
Retrospective 63 COVID+ kidney transplant recipients, showing significantly lower vitamin D levels before infection in patients requiring ICU admission. 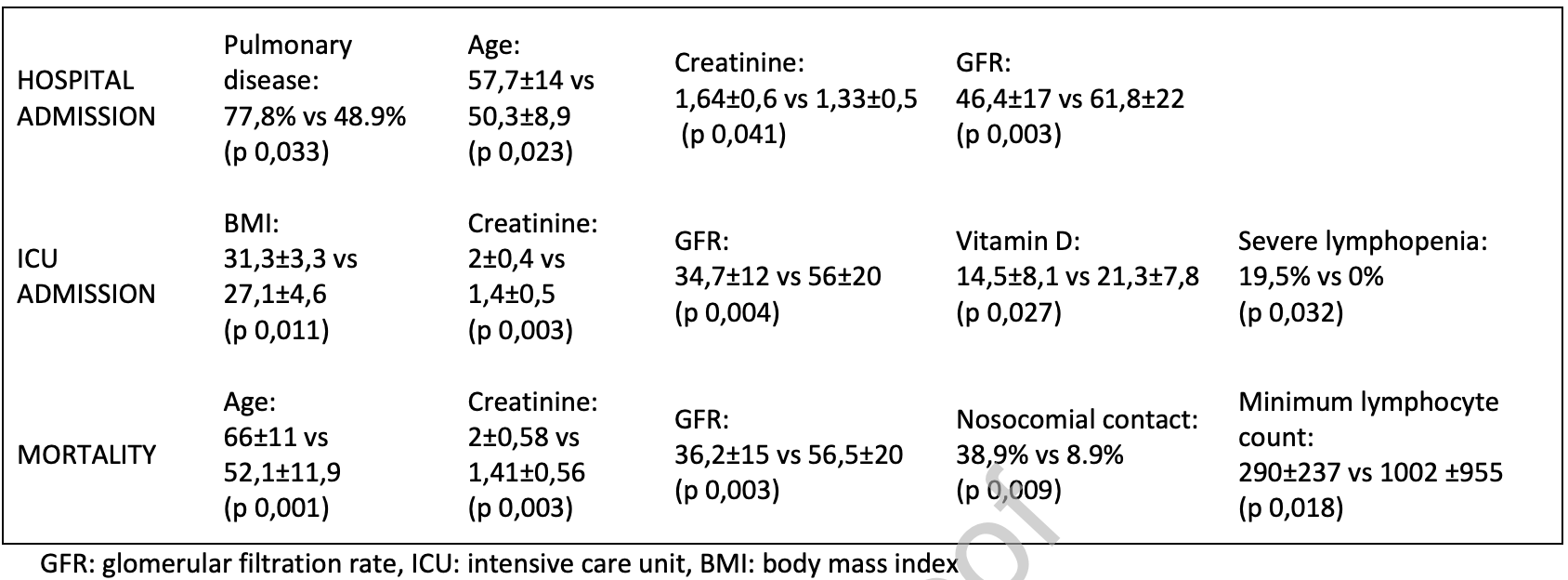 Sacristán et al., 11/12/2021, peer-reviewed, 9 authors. |
| Submit Corrections or Comments |
| Levels | Gönen et al., Nutrients, doi:10.3390/nu13114047 (Peer Reviewed) | death, ↓65.8%, p=0.62 | Rapid and Effective Vitamin D Supplementation May Present Better Clinical Outcomes in COVID-19 (SARS-CoV-2) Patients by Altering Serum INOS1, IL1B, IFNg, Cathelicidin-LL37, and ICAM1 |
| Details Retrospective 867 hospitalized COVID-19 patients in Turkey, showing worse outcomes with vitamin D deficiency (without statistical significance); followed by a prospective study of 210 patients with vitamin D supplementation for those that.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Gönen et al., Nutrients, doi:10.3390/nu13114047 (Peer Reviewed) |
| Rapid and Effective Vitamin D Supplementation May Present Better Clinical Outcomes in COVID-19 (SARS-CoV-2) Patients by Altering Serum INOS1, IL1B, IFNg, Cathelicidin-LL37, and ICAM1 |
Retrospective 867 hospitalized COVID-19 patients in Turkey, showing worse outcomes with vitamin D deficiency (without statistical significance); followed by a prospective study of 210 patients with vitamin D supplementation for those that were deficient, showing significantly lower mortality compared to the retrospective study without treatment. 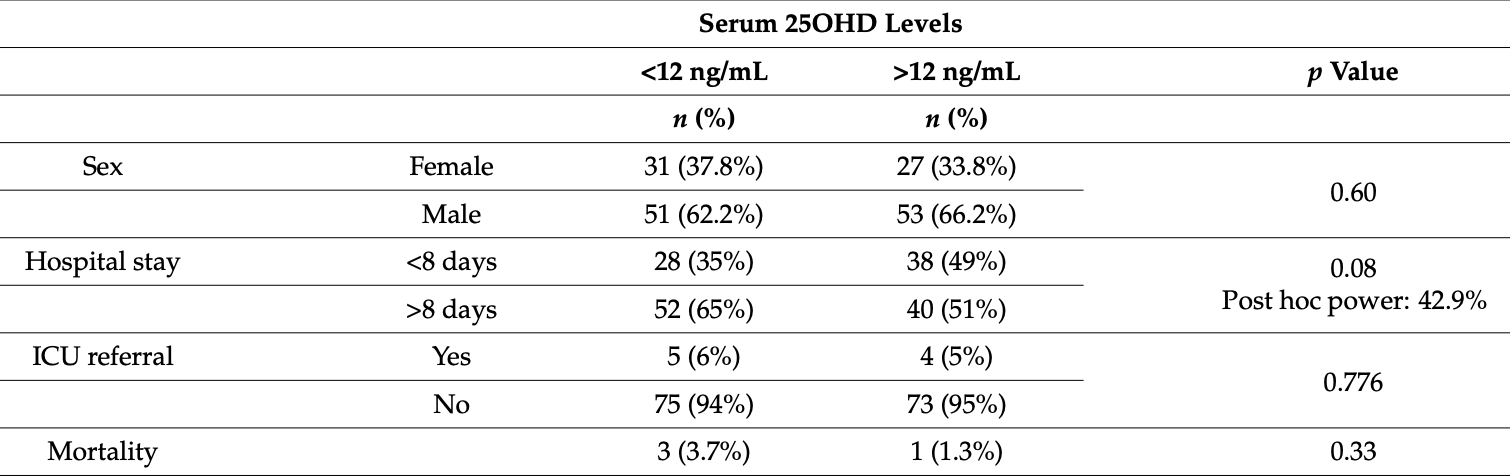 risk of death, 65.8% lower, RR 0.34, p = 0.62, high D levels (≥12ng/mL) 1 of 80 (1.2%), low D levels (<12ng/mL) 3 of 82 (3.7%), retrospective study. risk of ICU admission, 16.9% lower, RR 0.83, p = 1.00, high D levels (≥12ng/mL) 4 of 77 (5.2%), low D levels (<12ng/mL) 5 of 80 (6.2%), retrospective study. hospital stay >8 days, 21.1% lower, RR 0.79, p = 0.11, high D levels (≥12ng/mL) 40 of 78 (51.3%), low D levels (<12ng/mL) 52 of 80 (65.0%), retrospective study. Gönen et al., 11/12/2021, retrospective, Turkey, Europe, peer-reviewed, 20 authors, dosage varies. |
| Submit Corrections or Comments |
| Levels | Asghar et al., Am. J. Trop. Med. Hyg., doi:10.4269/ajtmh.21-0577 (Peer Reviewed) | death, ↓53.1%, p=0.05 | Evaluation of Vitamin-D Status and Its Association with Clinical Outcomes Among COVID-19 Patients in Pakistan |
| Details Retrospective 91 hospitalized patients in Pakistan, showing vitamin D deficiency associated with mortality in multivariate Cox regression. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Asghar et al., Am. J. Trop. Med. Hyg., doi:10.4269/ajtmh.21-0577 (Peer Reviewed) |
| Evaluation of Vitamin-D Status and Its Association with Clinical Outcomes Among COVID-19 Patients in Pakistan |
Retrospective 91 hospitalized patients in Pakistan, showing vitamin D deficiency associated with mortality in multivariate Cox regression. 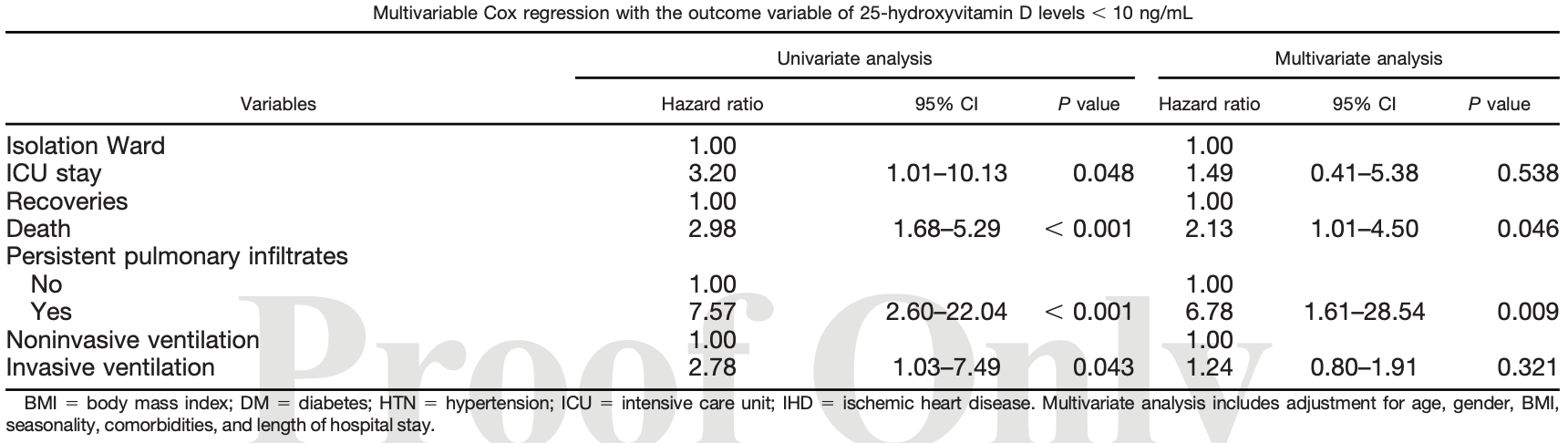 risk of death, 53.1% lower, RR 0.47, p = 0.05, high D levels (≥10ng/mL) 73, low D levels (<10ng/mL) 18, multivariate Cox regression. risk of mechanical ventilation, 19.4% lower, RR 0.81, p = 0.32, high D levels (≥10ng/mL) 5 of 73 (6.8%), low D levels (<10ng/mL) 6 of 18 (33.3%), adjusted, multivariate Cox regression. risk of ICU admission, 32.9% lower, RR 0.67, p = 0.54, high D levels (≥10ng/mL) 73, low D levels (<10ng/mL) 18, multivariate Cox regression. Asghar et al., 11/10/2021, retrospective, Pakistan, South Asia, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Gallelli et al., Nutrients, doi:10.3390/nu13113932 (Peer Reviewed) | Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study |
| Details Analysis of 117 patients in Italy, showing COVID-19 patients had significantly lower vitamin D levels than control patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Gallelli et al., Nutrients, doi:10.3390/nu13113932 (Peer Reviewed) |
| Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study |
Analysis of 117 patients in Italy, showing COVID-19 patients had significantly lower vitamin D levels than control patients. 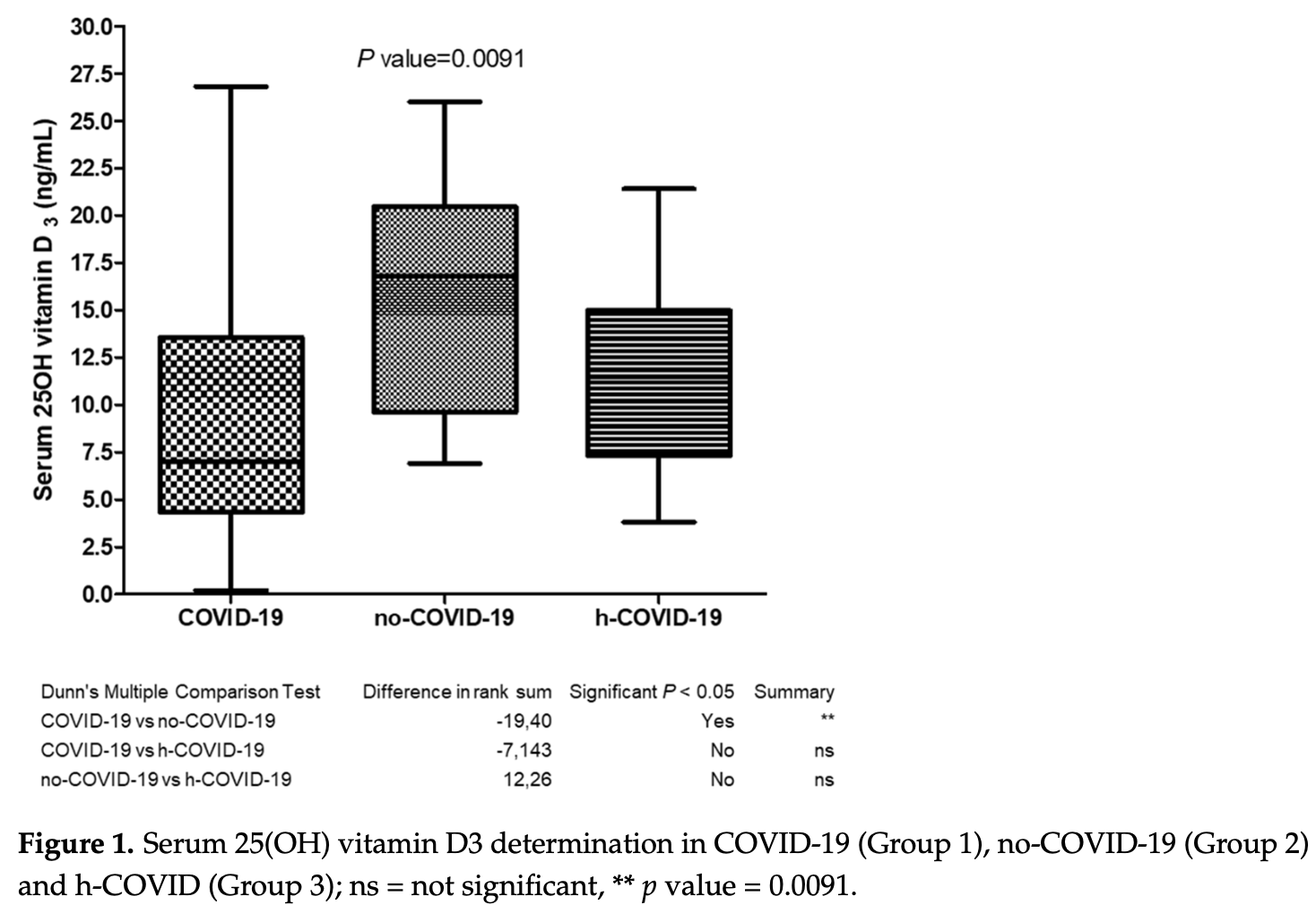 Gallelli et al., 11/3/2021, prospective, Italy, Europe, peer-reviewed, 17 authors. |
| Submit Corrections or Comments |
| Levels | Atanasovska et al., Redox Report, doi:10.1080/13510002.2021.1999126 (Peer Reviewed) | death, ↓40.7%, p=0.68 | Vitamin D levels and oxidative stress markers in patients hospitalized with COVID-19 |
| Details Retrospective 33 COVID-19 hospitalized patients in North Macedonia, showing significantly lower vitamin D levels for severe vs. moderate cases. Oxidative stress was also higher for vitamin D insufficient patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Atanasovska et al., Redox Report, doi:10.1080/13510002.2021.1999126 (Peer Reviewed) |
| Vitamin D levels and oxidative stress markers in patients hospitalized with COVID-19 |
Retrospective 33 COVID-19 hospitalized patients in North Macedonia, showing significantly lower vitamin D levels for severe vs. moderate cases. Oxidative stress was also higher for vitamin D insufficient patients. 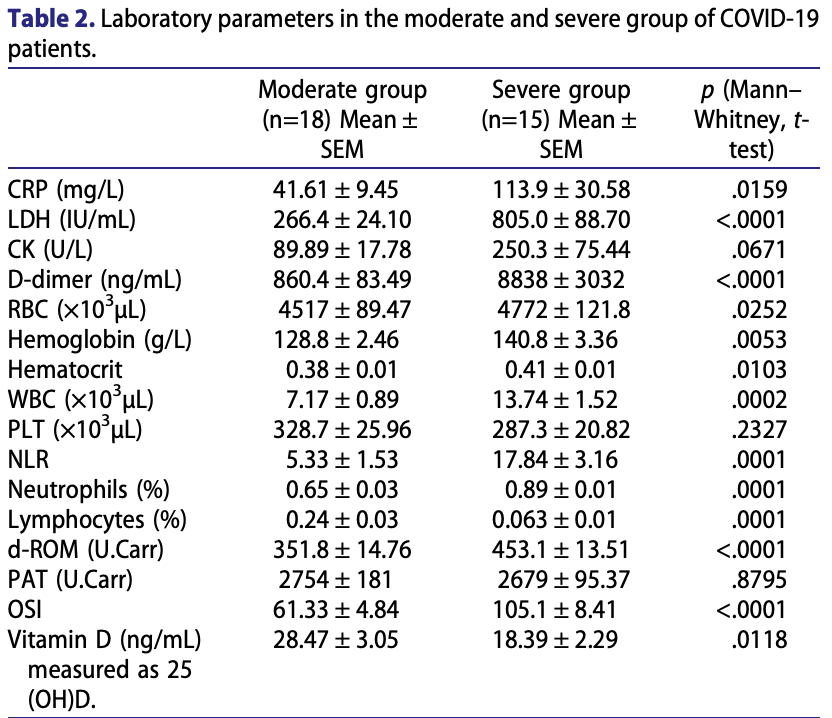 risk of death, 40.7% lower, RR 0.59, p = 0.68, high D levels (≥30ng/mL) 2 of 9 (22.2%), low D levels (<30ng/mL) 9 of 24 (37.5%). risk of severe case, 59.0% lower, RR 0.41, p = 0.13, high D levels (≥30ng/mL) 2 of 9 (22.2%), low D levels (<30ng/mL) 13 of 24 (54.2%). Atanasovska et al., 11/2/2021, retrospective, North Macedonia, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Late | Leal et al., SSRN, doi:10.2139/ssrn.3949424 (Preprint) | death, ↓85.7%, p=0.03 | Effect of a Nutritional Support System to Increase Survival and Reduce Mortality in Patients with COVID-19 in Stage III and Comorbidities: A Blinded Randomized Controlled Clinical Trial |
| Details 80 patient RCT with 40 patients treated with a comprehensive regimen of nutritional support, showing significantly lower mortality with treatment. Treatment contained cholecalciferol, vitamin C, zinc, spirulina maxima, folic acid, glutam.. |
| Details Source PDF Late treatment study Late treatment study |
| Leal et al., SSRN, doi:10.2139/ssrn.3949424 (Preprint) |
| Effect of a Nutritional Support System to Increase Survival and Reduce Mortality in Patients with COVID-19 in Stage III and Comorbidities: A Blinded Randomized Controlled Clinical Trial |
80 patient RCT with 40 patients treated with a comprehensive regimen of nutritional support, showing significantly lower mortality with treatment.Treatment contained cholecalciferol, vitamin C, zinc, spirulina maxima, folic acid, glutamine, vegetable protein, selenium, resveratrol, omega-3 fatty acids, l-arginine, magnesium, probiotics, and B-complex IV. Adherence was strictly monitored. NCT04507867. 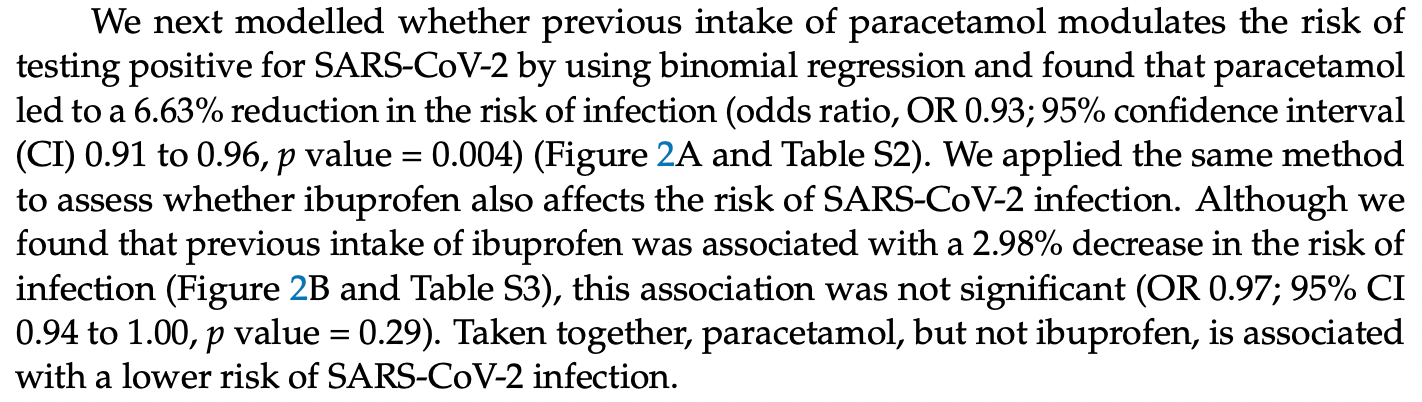 risk of death, 85.7% lower, RR 0.14, p = 0.03, treatment 1 of 40 (2.5%), control 7 of 40 (17.5%). risk of mechanical ventilation, 57.1% lower, RR 0.43, p = 0.31, treatment 3 of 40 (7.5%), control 7 of 40 (17.5%). Excluded in after exclusion results of meta analysis: combined treatments may contribute more to the effect seen. Leal et al., 10/25/2021, Randomized Controlled Trial, Mexico, North America, preprint, 7 authors, dosage 2,000IU days 1-21, this trial uses multiple treatments in the treatment arm (combined with comprehensive nutritional support) - results of individual treatments may vary. |
| Submit Corrections or Comments |
| Levels | Hurst et al., BMJ Open, doi:10.1136/bmjopen-2021-055435 (Peer Reviewed) | death, ↓68.4%, p=0.005 | Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: a cross-sectional study |
| Details Analysis of 259 hospitalized COVID-19 patients in the UK, showing a majority of patients had vitamin D deficiency/insufficiency, which was associated with poor outcomes. Both free and total 25(OH)D were analyzed with consistent results. I.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Hurst et al., BMJ Open, doi:10.1136/bmjopen-2021-055435 (Peer Reviewed) |
| Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: a cross-sectional study |
Analysis of 259 hospitalized COVID-19 patients in the UK, showing a majority of patients had vitamin D deficiency/insufficiency, which was associated with poor outcomes. Both free and total 25(OH)D were analyzed with consistent results. ISRCTN66726260. 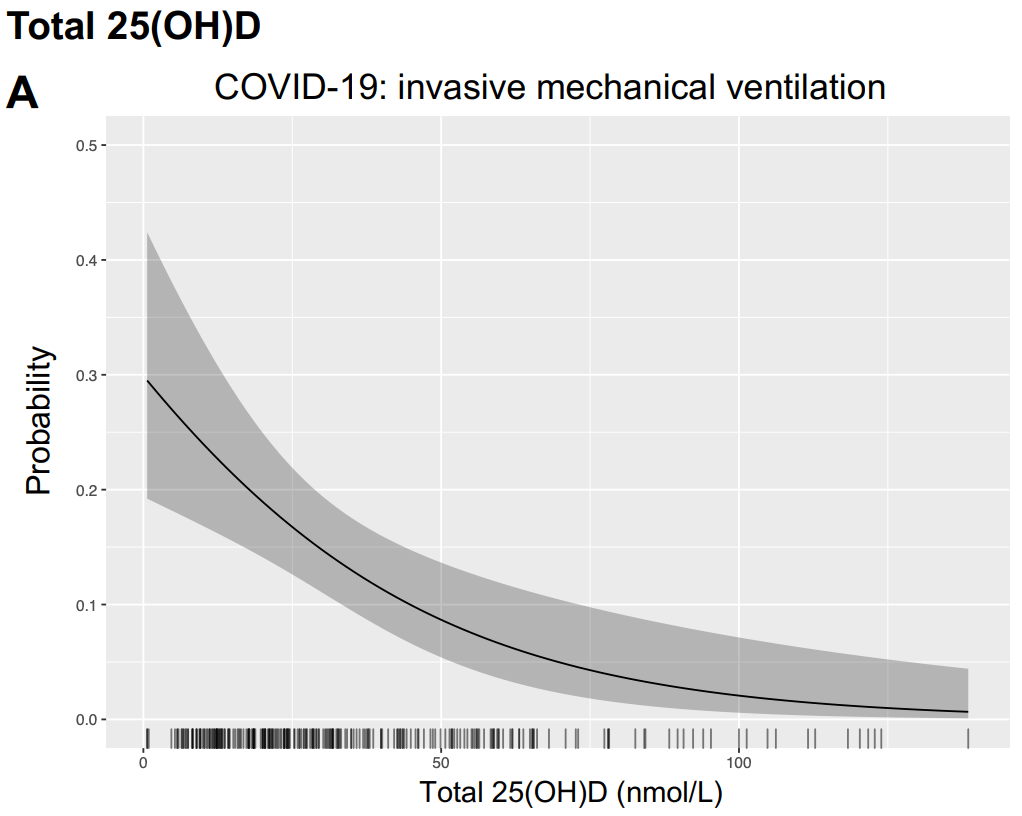 risk of death, 68.4% lower, RR 0.32, p = 0.005, high D levels 68, low D levels 191, OR converted to RR, >50nmol/l, multivariable, Supplementary Table 2, control prevalance approximated with overall prevalence. risk of mechanical ventilation, 66.0% lower, RR 0.34, p = 0.004, high D levels 6 of 68 (8.8%), low D levels 61 of 191 (31.9%), OR converted to RR, >50nmol/l, multivariable, Supplementary Table 2. Hurst et al., 10/22/2021, prospective, United Kingdom, Europe, peer-reviewed, 23 authors. |
| Submit Corrections or Comments |
| Levels | Al-Anouti et al., Nutrients, doi:10.3390/nu13113680 (Peer Reviewed) | severe case, ↓68.1%, p=0.0007 | Associations between Genetic Variants in the Vitamin D Metabolism Pathway and Severity of COVID-19 among UAE Residents |
| Details Retrospective 646 COVID-19 patients in the UAE, showing significant associations between genetic determinants of vitamin D metabolism and COVID-19 severity, and an association with vitamin D deficiency and COVID-19 severity. Patients in t.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Al-Anouti et al., Nutrients, doi:10.3390/nu13113680 (Peer Reviewed) |
| Associations between Genetic Variants in the Vitamin D Metabolism Pathway and Severity of COVID-19 among UAE Residents |
Retrospective 646 COVID-19 patients in the UAE, showing significant associations between genetic determinants of vitamin D metabolism and COVID-19 severity, and an association with vitamin D deficiency and COVID-19 severity. Patients in this study overlap with [1]. DOH/DQD/2020/538. 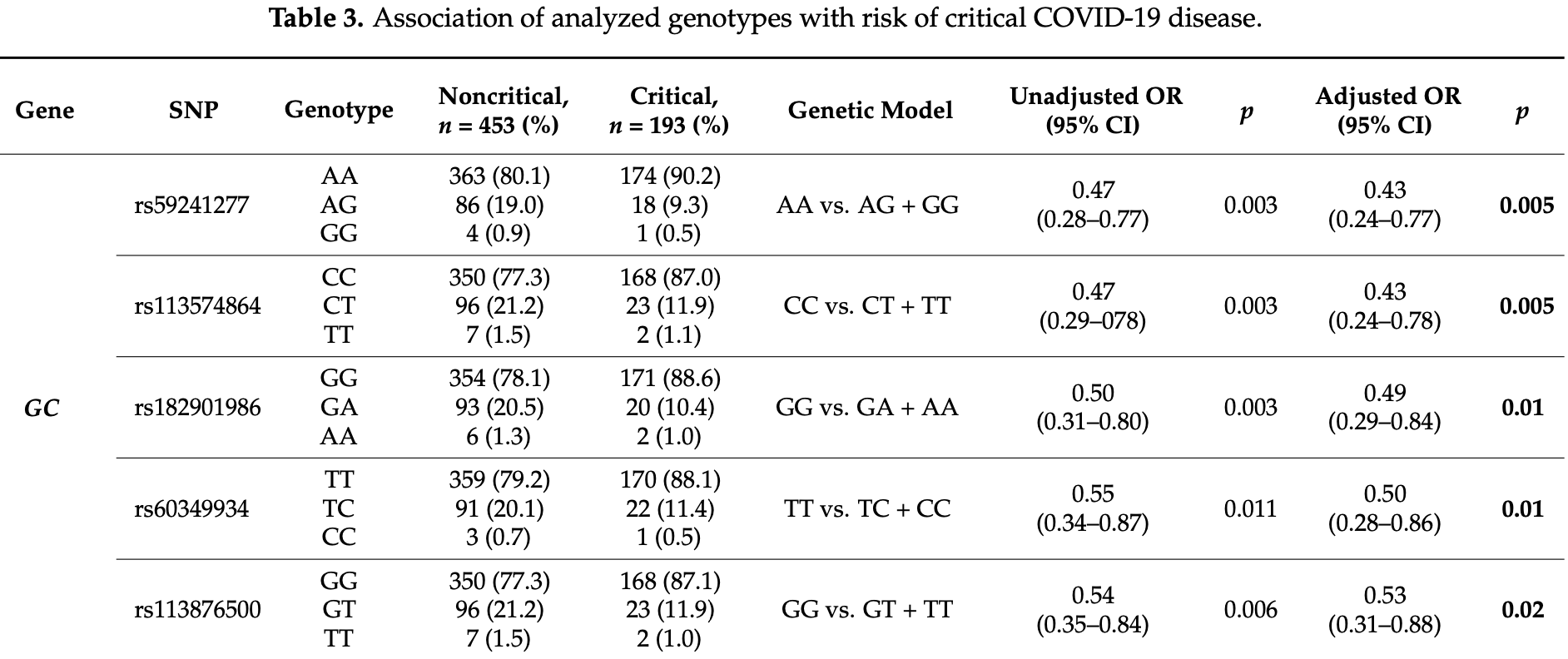 risk of severe case, 68.1% lower, RR 0.32, p < 0.001, high D levels 56 of 146 (38.4%), low D levels 52 of 142 (36.6%), adjusted, OR converted to RR, <12ng/ml vs. >20ng/ml. Al-Anouti et al., 10/20/2021, retrospective, United Arab Emirates, Middle East, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Ramirez-Sandoval et al., Archives of Medical Research, doi:10.1016/j.arcmed.2021.09.006 (Peer Reviewed) | death, ↓31.5%, p<0.0001 | Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19 |
| Details Retrospective 2,908 hospitalized patients in Mexico with vitamin D levels measured on admission, showing significantly lower mortality for patients without vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ramirez-Sandoval et al., Archives of Medical Research, doi:10.1016/j.arcmed.2021.09.006 (Peer Reviewed) |
| Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19 |
Retrospective 2,908 hospitalized patients in Mexico with vitamin D levels measured on admission, showing significantly lower mortality for patients without vitamin D deficiency. 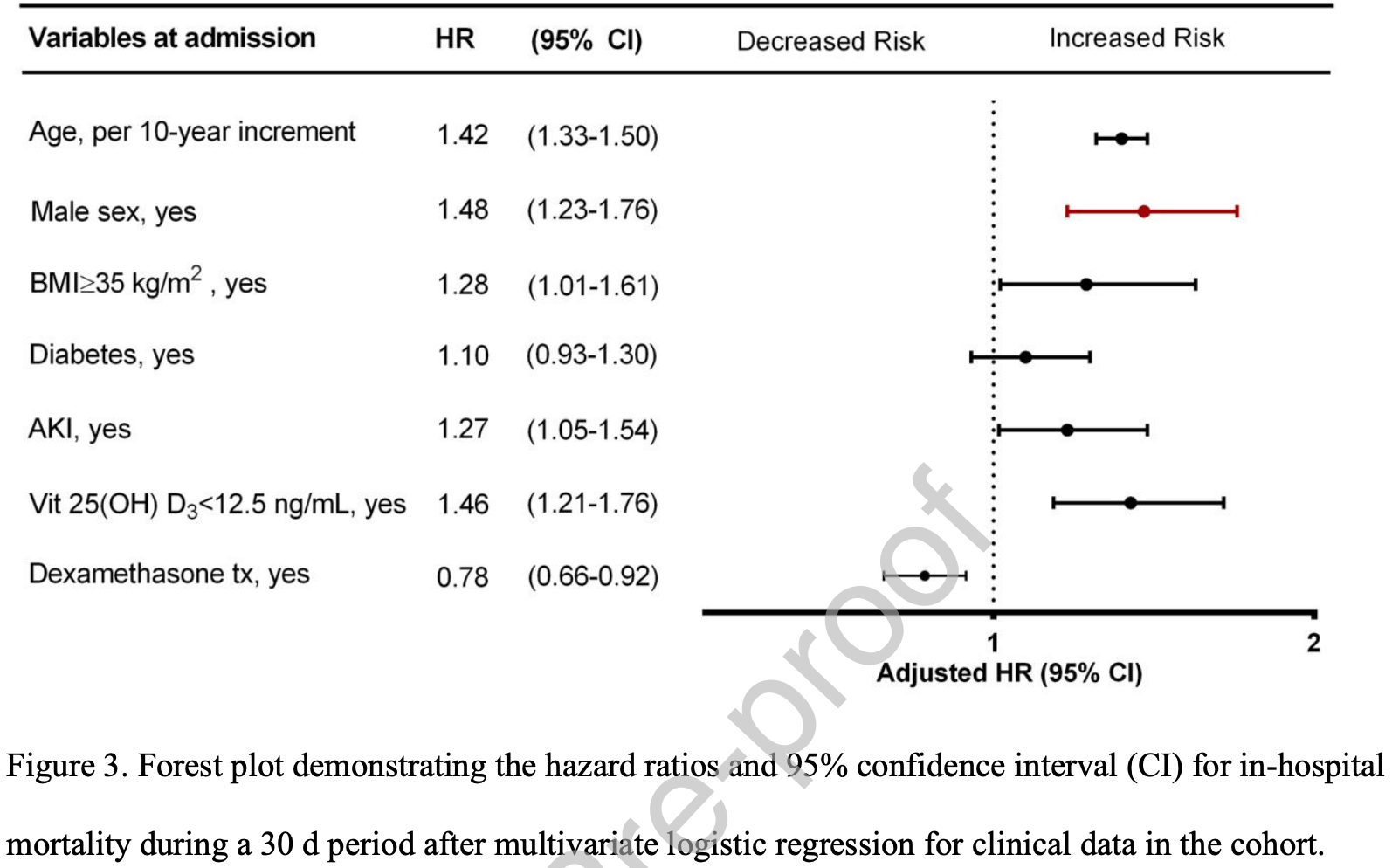 risk of death, 31.5% lower, RR 0.68, p < 0.001, high D levels 2,337, low D levels 571, adjusted, >12.5ng/mL, 30 day in-hospital mortality. hospitalization time, 22.2% lower, relative time 0.78, p < 0.001, high D levels 2,337, low D levels 571. Ramirez-Sandoval et al., 10/15/2021, retrospective, Mexico, North America, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Late | Maghbooli et al., Endocrine Practice, doi:10.1016/j.eprac.2021.09.016 (Peer Reviewed) | death, ↓40.0%, p=0.72 | Treatment with 25-hydroxyvitamin D3 (calcifediol) is associated with a reduction in the blood neutrophil-to-lymphocyte ratio marker of disease severity in patients hospitalized with COVID-19: a pilot, multicenter, randomized, placebo-controlled double blind clinical trial |
| Details RCT 106 hospitalized patients with vitamin D levels <30ng/ml in Iran, 53 treated with calcifediol, showing that treatment was able to correct vitamin D deficiency/insufficiency, resulting in improved immune system function. Hospitalizatio.. |
| Details Source PDF Late treatment study Late treatment study |
| Maghbooli et al., Endocrine Practice, doi:10.1016/j.eprac.2021.09.016 (Peer Reviewed) |
| Treatment with 25-hydroxyvitamin D3 (calcifediol) is associated with a reduction in the blood neutrophil-to-lymphocyte ratio marker of disease severity in patients hospitalized with COVID-19: a pilot, multicenter, randomized, placebo-controlled double blind clinical trial |
RCT 106 hospitalized patients with vitamin D levels <30ng/ml in Iran, 53 treated with calcifediol, showing that treatment was able to correct vitamin D deficiency/insufficiency, resulting in improved immune system function. Hospitalization, ICU duration, ventilation, and mortality was lower with treatment, without reaching statistical significance with the small sample size. The dosage used in this trial was much lower than other trials. 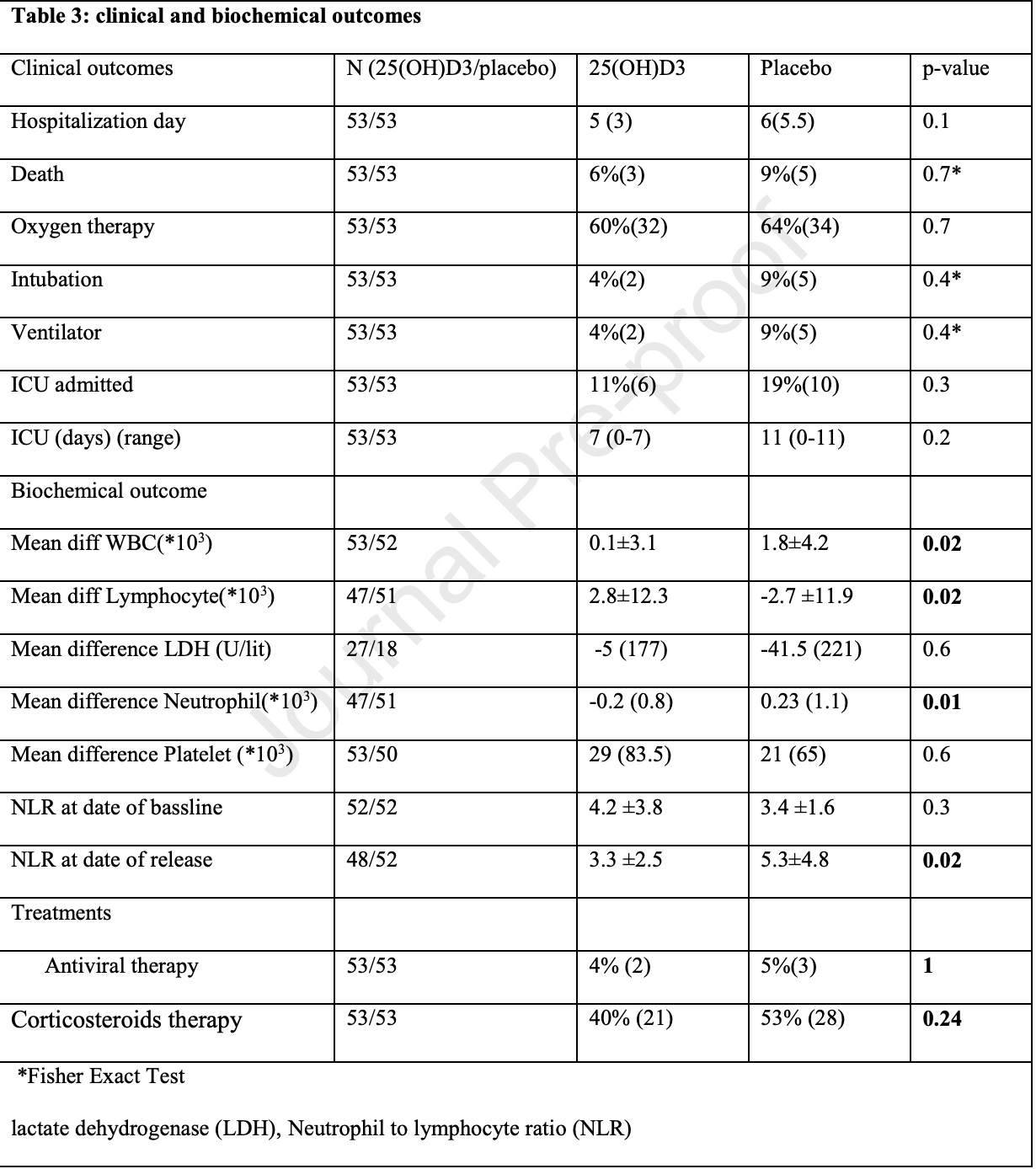 risk of death, 40.0% lower, RR 0.60, p = 0.72, treatment 3 of 53 (5.7%), control 5 of 53 (9.4%). risk of mechanical ventilation, 60.0% lower, RR 0.40, p = 0.44, treatment 2 of 53 (3.8%), control 5 of 53 (9.4%). risk of ICU admission, 40.0% lower, RR 0.60, p = 0.42, treatment 6 of 53 (11.3%), control 10 of 53 (18.9%). ICU time, 36.4% lower, relative time 0.64, p = 0.20, treatment 53, control 53. hospitalization time, 16.7% lower, relative time 0.83, p = 0.10, treatment 53, control 53. Maghbooli et al., 10/13/2021, Double Blind Randomized Controlled Trial, Iran, Middle East, peer-reviewed, 12 authors, dosage calcifediol 25μg daily, mean daily dose. |
| Submit Corrections or Comments |
| Levels | Afaghi et al., The Tohoku Journal of Experimental Medicine, doi:10.1620/tjem.255.127 (Peer Reviewed) | death, ↓55.0%, p=0.002 | Prevalence and Clinical Outcomes of Vitamin D Deficiency in COVID-19 Hospitalized Patients: A Retrospective Single-Center Analysis |
| Details Retrospective 646 COVID-19+ hospitalized patients in Iran, showing higher mortality with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Afaghi et al., The Tohoku Journal of Experimental Medicine, doi:10.1620/tjem.255.127 (Peer Reviewed) |
| Prevalence and Clinical Outcomes of Vitamin D Deficiency in COVID-19 Hospitalized Patients: A Retrospective Single-Center Analysis |
Retrospective 646 COVID-19+ hospitalized patients in Iran, showing higher mortality with vitamin D deficiency. 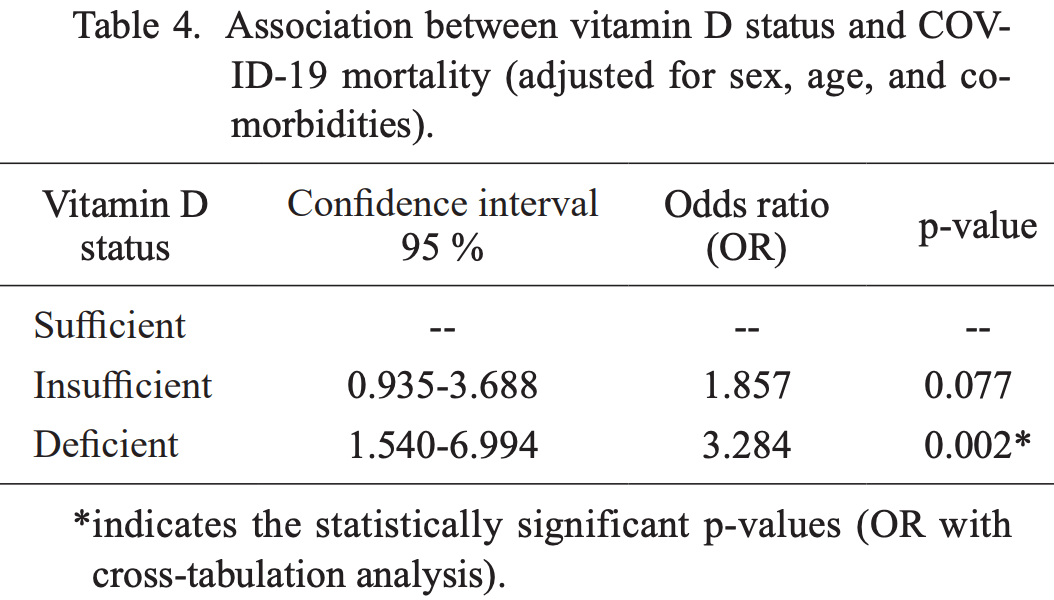 risk of death, 55.0% lower, RR 0.45, p = 0.002, high D levels 97 of 537 (18.1%), low D levels 51 of 109 (46.8%), adjusted, OR converted to RR, >20ng/mL, multivariate. risk of mechanical ventilation, 55.9% lower, RR 0.44, p < 0.001, high D levels 89 of 537 (16.6%), low D levels 41 of 109 (37.6%), >20ng/mL, unadjusted. risk of ICU admission, 34.1% lower, RR 0.66, p < 0.001, high D levels 211 of 537 (39.3%), low D levels 65 of 109 (59.6%), >20ng/mL, unadjusted. Afaghi et al., 10/12/2021, retrospective, Iran, Middle East, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| PrEP, Early | Worcel et al., Annals of Palliative Medicine, doi:10.21037/apm-21-1707 (Peer Reviewed) | Low mortality from COVID-19 at a nursing facility in France following a combined preventive and active treatment protocol |
| Details Report on the relatively low mortality and relatively mild COVID-19 symptoms at a French nursing facility that has adopted several treatments including vitamin D, zinc, anticoagulants, corticosteroids, and a multivitamin. |
| Details Source PDF PrEP, Early PrEP, Early |
| Worcel et al., Annals of Palliative Medicine, doi:10.21037/apm-21-1707 (Peer Reviewed) |
| Low mortality from COVID-19 at a nursing facility in France following a combined preventive and active treatment protocol |
Report on the relatively low mortality and relatively mild COVID-19 symptoms at a French nursing facility that has adopted several treatments including vitamin D, zinc, anticoagulants, corticosteroids, and a multivitamin. 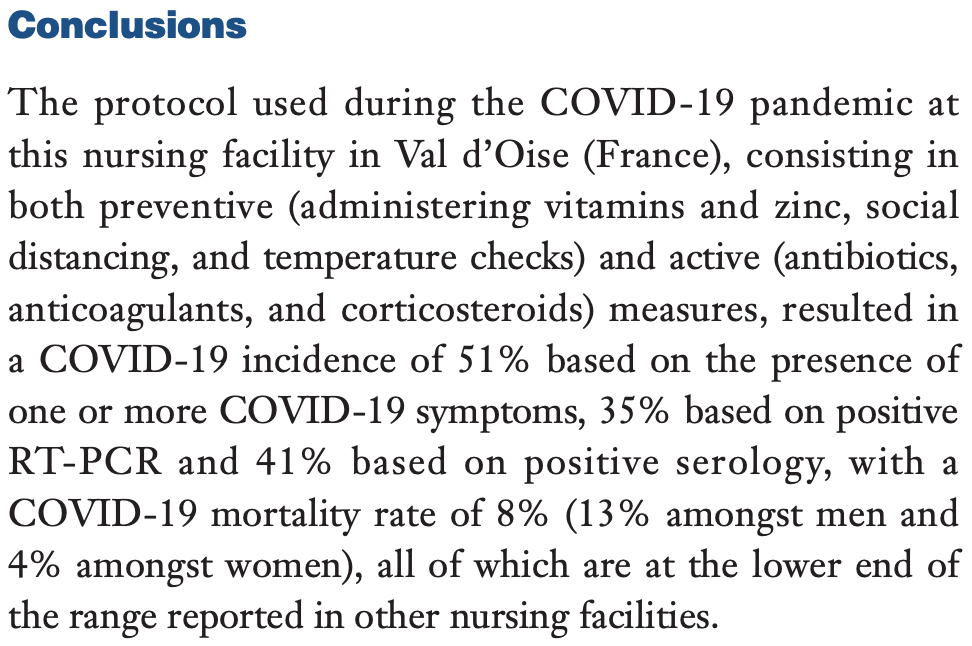 Worcel et al., 10/12/2021, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Late | Caballero-García et al., Medicina, doi:10.3390/medicina57101079 (Peer Reviewed) | Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection |
| Details Small RCT with 30 patients examining the effect of vitamin D supplementation on muscle status in elderly recovering COVID-19 patients, showing serum creatine kinase levels returned to optimal values, however there was no significant diffe.. |
| Details Source PDF Late treatment study Late treatment study |
| Caballero-García et al., Medicina, doi:10.3390/medicina57101079 (Peer Reviewed) |
| Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection |
Small RCT with 30 patients examining the effect of vitamin D supplementation on muscle status in elderly recovering COVID-19 patients, showing serum creatine kinase levels returned to optimal values, however there was no significant difference in physical test results.
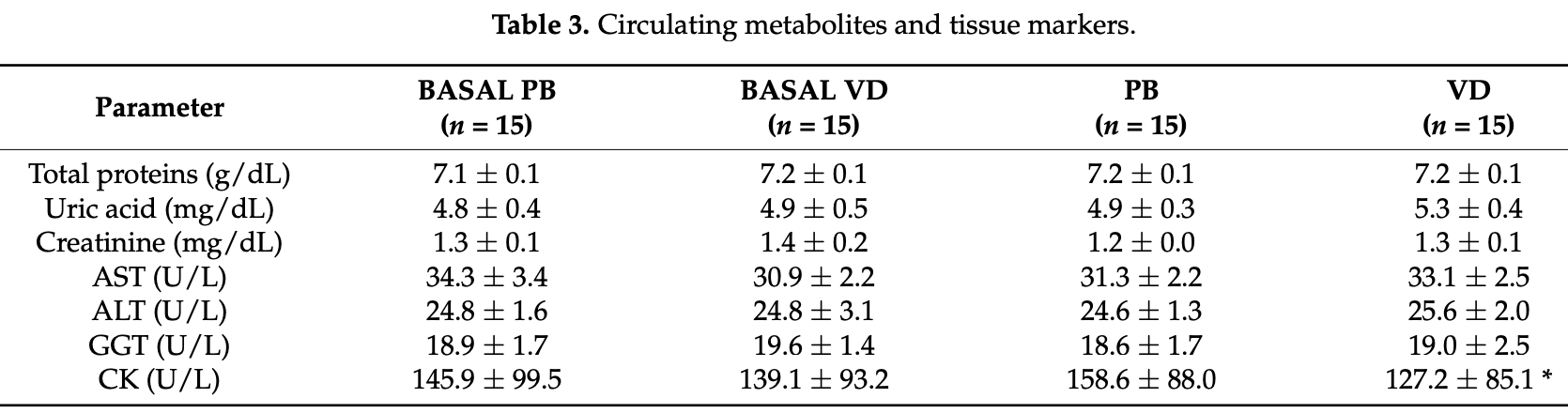 Caballero-García et al., 10/9/2021, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Levels | Mukherjee et al., FEBS Open Bio, doi:10.1002/2211-5463.13309 (Peer Reviewed) | Seasonal UV exposure and vitamin D: Association with the dynamics of COVID-19 transmission in Europe |
| Details Analysis of UV and temperature levels in 26 European countries, showing that low temperature, UV index, and cloud-free vitamin D UV dose levels are negatively correlated with COVID-19 prevalence. Authors suggest that low UV exposure can a.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Mukherjee et al., FEBS Open Bio, doi:10.1002/2211-5463.13309 (Peer Reviewed) |
| Seasonal UV exposure and vitamin D: Association with the dynamics of COVID-19 transmission in Europe |
Analysis of UV and temperature levels in 26 European countries, showing that low temperature, UV index, and cloud-free vitamin D UV dose levels are negatively correlated with COVID-19 prevalence. Authors suggest that low UV exposure can affect the required production of vitamin D in the body, which substantially influences the dynamics of COVID-19 transmission and severity. 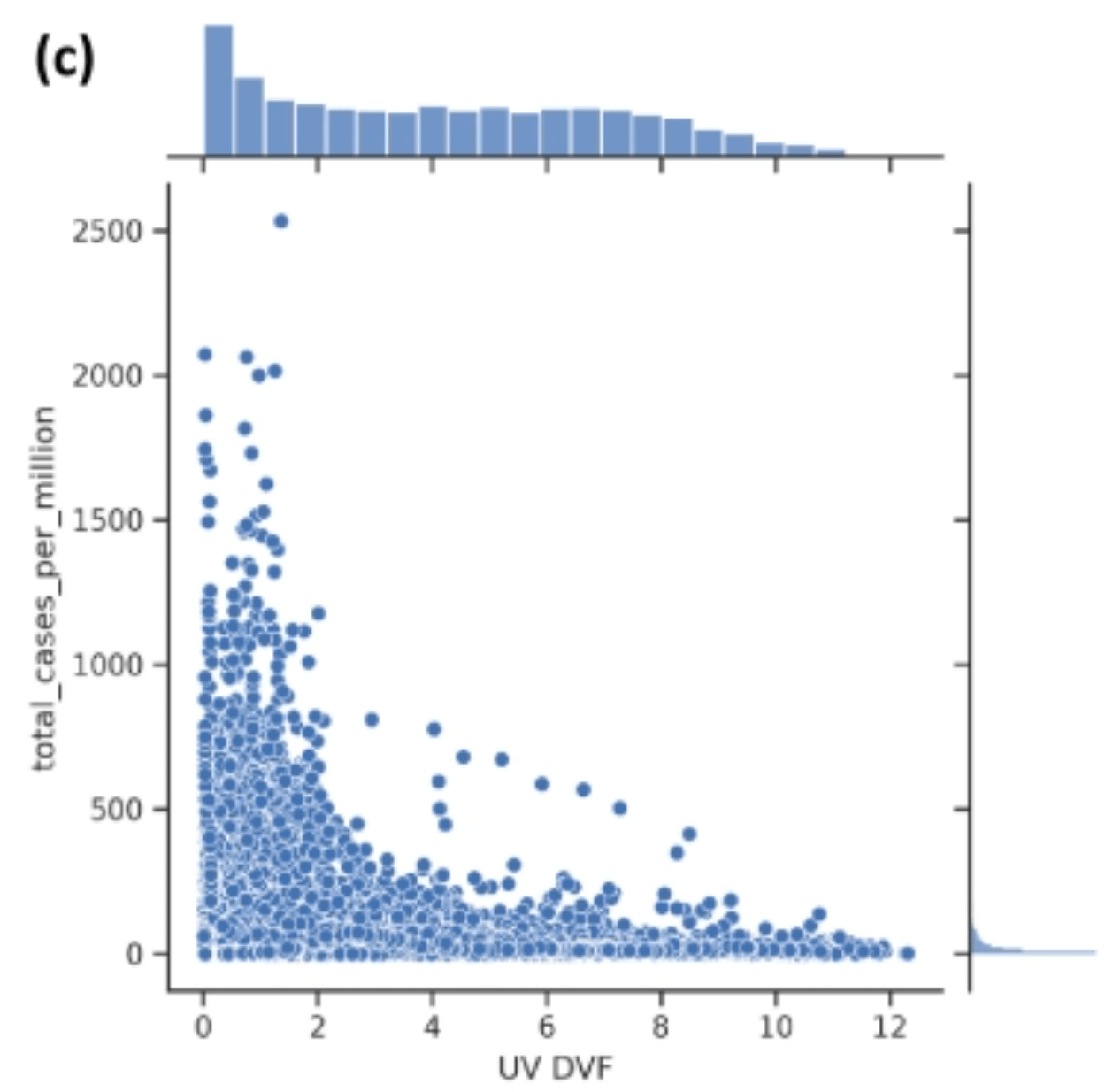 Mukherjee et al., 10/5/2021, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Abdollahzadeh et al., Infection, Genetics and Evolution, doi:10.1016/j.meegid.2021.105098 (Peer Reviewed) | Association of Vitamin D receptor gene polymorphisms and clinical/severe outcomes of COVID-19 patients |
| Details Analysis of 500 hospitalized patients in Iran, showing associations between specific vitamin D receceptor gene polymorphisms and COVID-19 outcomes. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Abdollahzadeh et al., Infection, Genetics and Evolution, doi:10.1016/j.meegid.2021.105098 (Peer Reviewed) |
| Association of Vitamin D receptor gene polymorphisms and clinical/severe outcomes of COVID-19 patients |
Analysis of 500 hospitalized patients in Iran, showing associations between specific vitamin D receceptor gene polymorphisms and COVID-19 outcomes. 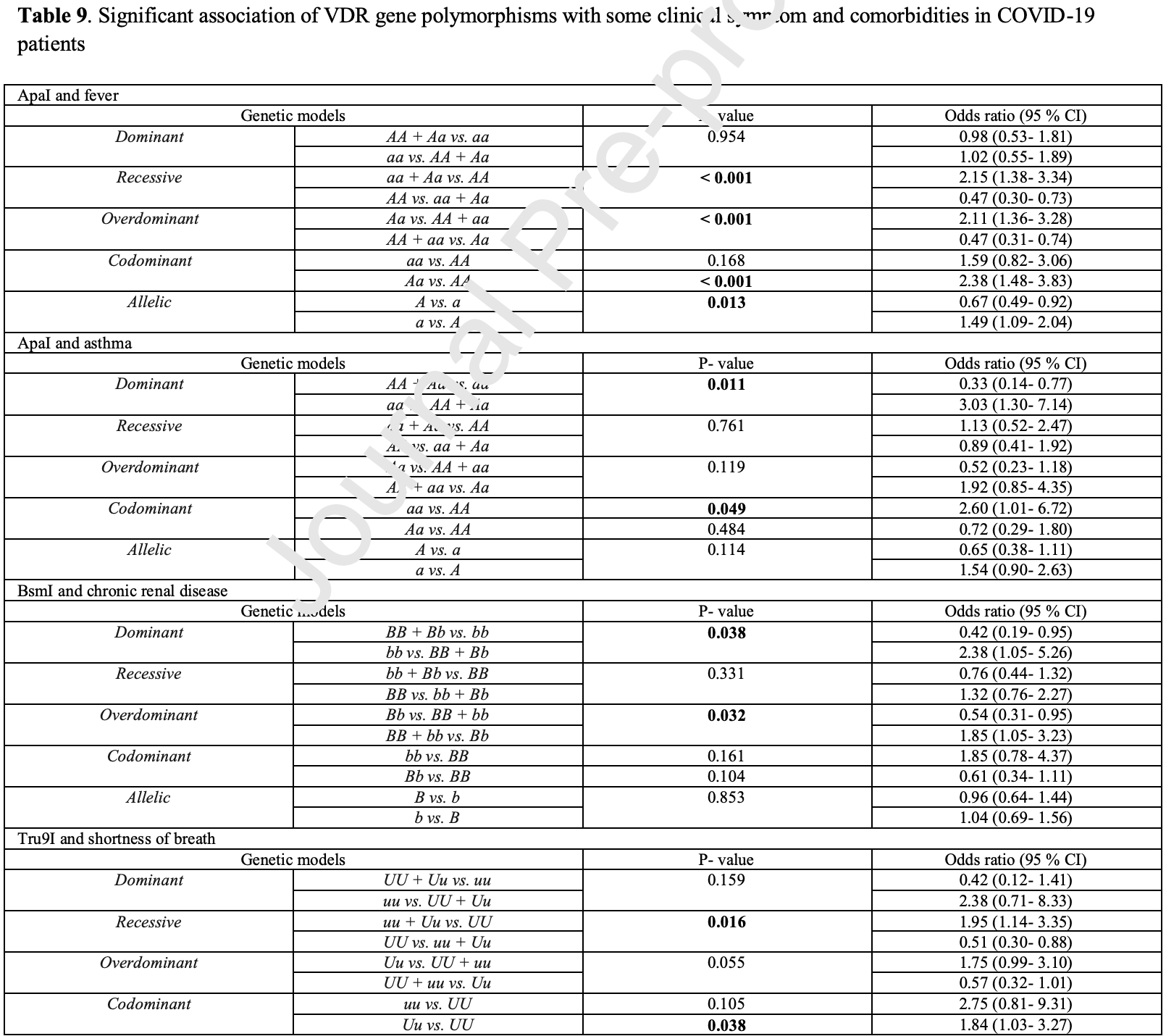 Abdollahzadeh et al., 10/2/2021, peer-reviewed, 9 authors. |
| Submit Corrections or Comments |
| Late | Yildiz et al., Bratislava Medical Journal, doi:10.4149/BLL_2021_119 (Peer Reviewed) | death, ↓80.9%, p=0.04 | The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia |
| Details Retrospective 207 hospitalized patients in Turkey, 37 with vitamin D levels <30ng/ml treated with a 300,000IU vitamin D, showing lower mortality with treatment. |
| Details Source PDF Late treatment study Late treatment study |
| Yildiz et al., Bratislava Medical Journal, doi:10.4149/BLL_2021_119 (Peer Reviewed) |
| The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia |
Retrospective 207 hospitalized patients in Turkey, 37 with vitamin D levels <30ng/ml treated with a 300,000IU vitamin D, showing lower mortality with treatment. 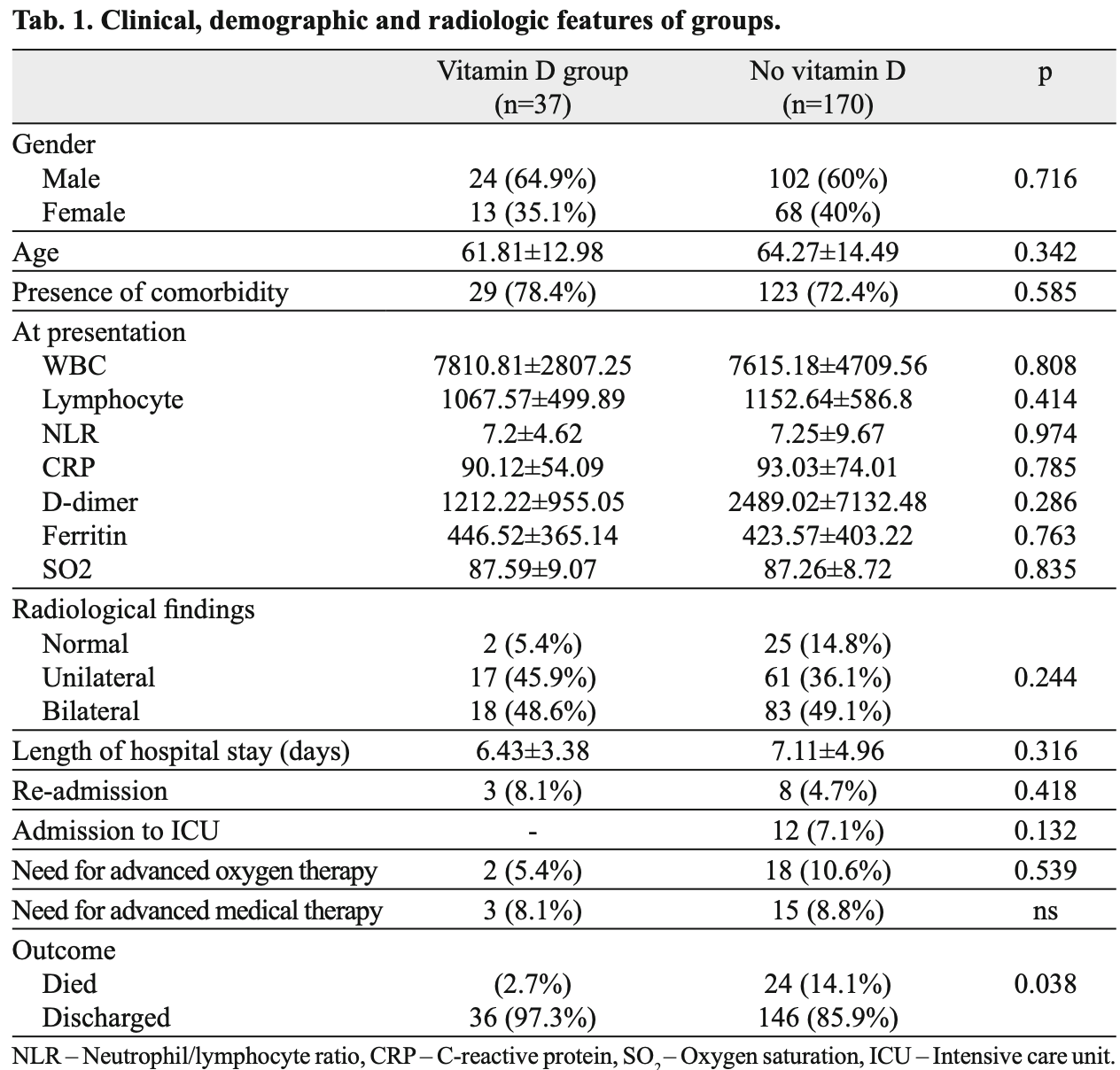 risk of death, 80.9% lower, RR 0.19, p = 0.04, treatment 1 of 37 (2.7%), control 24 of 170 (14.1%). risk of ICU admission, 94.5% lower, RR 0.06, p = 0.13, treatment 0 of 37 (0.0%), control 14 of 170 (8.2%), relative risk is not 0 because of continuity correction due to zero events. hospitalization time, 9.6% lower, relative time 0.90, p = 0.32, treatment 37, control 170. Yildiz et al., 9/27/2021, retrospective, Turkey, Europe, peer-reviewed, 5 authors, dosage 300,000IU single dose. |
| Submit Corrections or Comments |
| Meta | Borsche et al., Nutrients, doi:10.3390/nu13103596 (preprint 9/25/2021) (Peer Reviewed) (meta analysis) | meta-analysis | COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis |
| Details Meta analysis of 8 studies with vitamin D levels measured pre-infection or on the day of hospital admission, showing a correlation between the levels and mortality. Authors recommend combining vaccination with vitamin D supplementation to.. |
| Details Source PDF Meta Meta |
| Borsche et al., Nutrients, doi:10.3390/nu13103596 (preprint 9/25/2021) (Peer Reviewed) (meta analysis) |
| COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis |
Meta analysis of 8 studies with vitamin D levels measured pre-infection or on the day of hospital admission, showing a correlation between the levels and mortality. Authors recommend combining vaccination with vitamin D supplementation to maintain levels above 50 ng/ml. Authors extrapolate to predict a point of zero mortality, however there is no reason to predict a linear relationship where zero mortality would be reached.  Borsche et al., 9/25/2021, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Arroyo-Díaz et al., Frontiers in Public Health, doi:10.3389/fpubh.2021.758347 (Peer Reviewed) | death, ↑12.4%, p=0.59 | Previous Vitamin D Supplementation and Morbidity and Mortality Outcomes in People Hospitalised for COVID19: A Cross-Sectional Study |
| Details Retrospective 1,267 hospitalized patients in Spain, 189 on vitamin D supplementation before admission, showing lower ICU admission with supplementation, and no statistically significant difference for mortality or ventilation. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Arroyo-Díaz et al., Frontiers in Public Health, doi:10.3389/fpubh.2021.758347 (Peer Reviewed) |
| Previous Vitamin D Supplementation and Morbidity and Mortality Outcomes in People Hospitalised for COVID19: A Cross-Sectional Study |
Retrospective 1,267 hospitalized patients in Spain, 189 on vitamin D supplementation before admission, showing lower ICU admission with supplementation, and no statistically significant difference for mortality or ventilation. 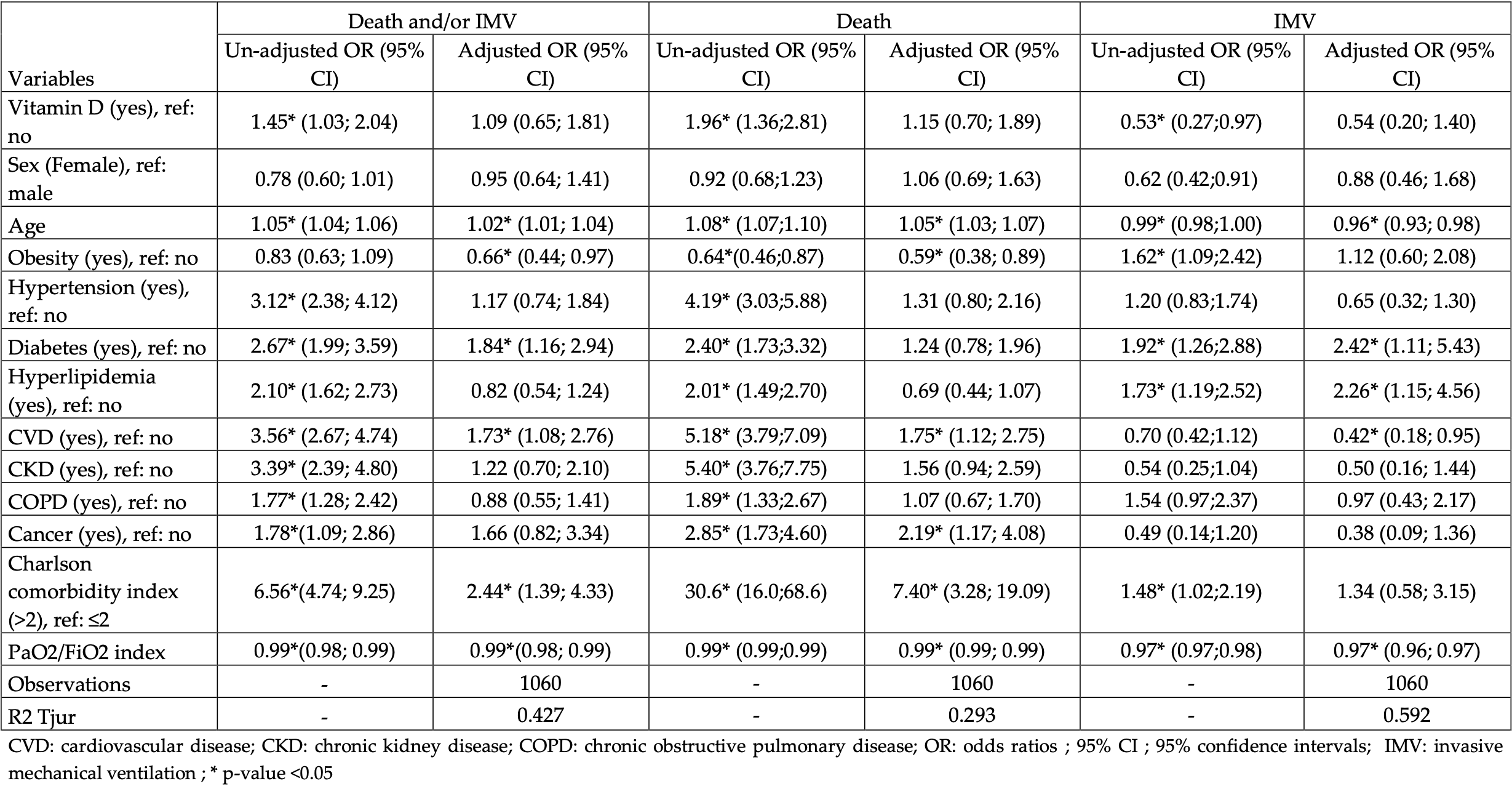 risk of death, 12.4% higher, RR 1.12, p = 0.59, treatment 50 of 189 (26.5%), control 167 of 1,078 (15.5%), adjusted, OR converted to RR. risk of mechanical ventilation, 43.3% lower, RR 0.57, p = 0.22, treatment 11 of 189 (5.8%), control 113 of 1,078 (10.5%), adjusted, OR converted to RR. risk of ICU admission, 44.2% lower, RR 0.56, p = 0.03, treatment 13 of 189 (6.9%), control 133 of 1,078 (12.3%), unadjusted. hospitalization time, 11.8% lower, relative time 0.88, p = 0.20, treatment 189, control 1,078, unadjusted. Arroyo-Díaz et al., 9/24/2021, retrospective, Spain, Europe, peer-reviewed, 11 authors, dosage not specified. |
| Submit Corrections or Comments |
| Review | Castle et al., Journal of Inflammation Research, doi:10.2147/JIR.S323356 (Review) (Peer Reviewed) | review | Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation |
| Details Review of the effects of COVID-19 on inflammatory markers, and the effects on those markers of standard treatments vs. vitamin D, melatonin, and meditation, showing comparable or superior effects with the non-standard treatments. The stan.. |
| Details Source PDF Review Review |
| Castle et al., Journal of Inflammation Research, doi:10.2147/JIR.S323356 (Review) (Peer Reviewed) |
| Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation |
Review of the effects of COVID-19 on inflammatory markers, and the effects on those markers of standard treatments vs. vitamin D, melatonin, and meditation, showing comparable or superior effects with the non-standard treatments. The standard treatments in this study were remdesivir and tocilizumab. We note that standard treatments vary widely around the world, for example vitamin D is a standard treatment in many locations. 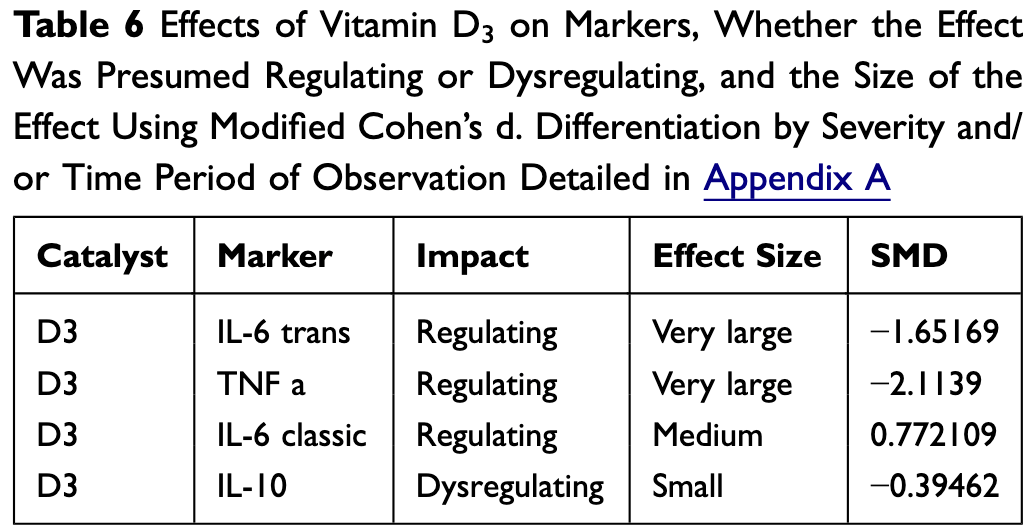 Castle et al., 9/22/2021, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Marino-Ramirez et al., medRxiv, doi:10.1101/2021.09.20.21263865 (Preprint) | Vitamin D and socioeconomic deprivation mediate COVID-19 ethnic health disparities |
| Details UK Biobank retrospective showing that vitamin supplements, including vitamin D, mediate the Asian disparity in COVID-19 susceptibility, and vitamin D levels mediate Asian and Black COVID-19 severity disparities. Authors conclude that the .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Marino-Ramirez et al., medRxiv, doi:10.1101/2021.09.20.21263865 (Preprint) |
| Vitamin D and socioeconomic deprivation mediate COVID-19 ethnic health disparities |
UK Biobank retrospective showing that vitamin supplements, including vitamin D, mediate the Asian disparity in COVID-19 susceptibility, and vitamin D levels mediate Asian and Black COVID-19 severity disparities. Authors conclude that the results support the use of vitamin D as both a prophylactic and a supplemental therapeutic for COVID-19 in those individuals. 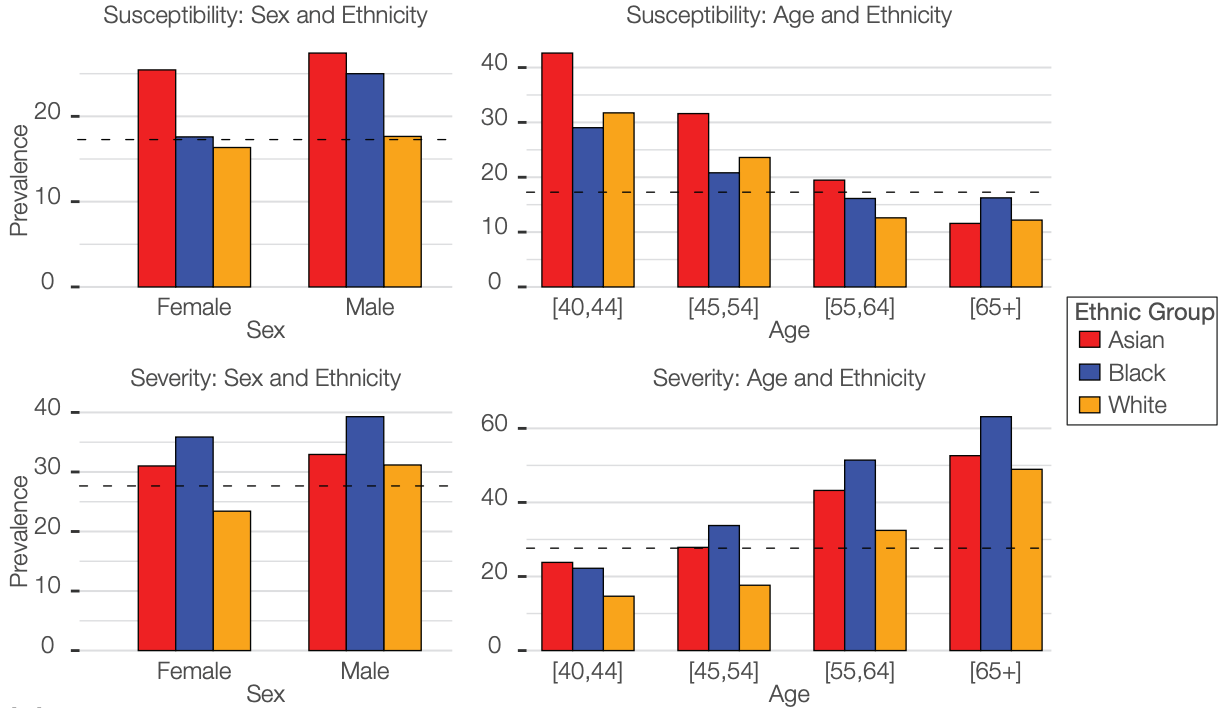 Marino-Ramirez et al., 9/22/2021, preprint, 7 authors. |
| Submit Corrections or Comments |
| Levels | Derakhshanian et al., Food Science & Nutrition, doi:10.1002/fsn3.2591 (Peer Reviewed) | death, ↓44.8%, p=0.05 | The predictive power of serum vitamin D for poor outcomes in COVID-19 patients |
| Details Retrospective 290 hospitalized patients in Iran, showing higher mortality with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Derakhshanian et al., Food Science & Nutrition, doi:10.1002/fsn3.2591 (Peer Reviewed) |
| The predictive power of serum vitamin D for poor outcomes in COVID-19 patients |
Retrospective 290 hospitalized patients in Iran, showing higher mortality with vitamin D deficiency.  risk of death, 44.8% lower, RR 0.55, p = 0.05, high D levels 148, low D levels 142, OR converted to RR, control prevalance approximated with overall prevalence. risk of mechanical ventilation, 41.7% lower, RR 0.58, p = 0.09, high D levels 148, low D levels 142, OR converted to RR, control prevalance approximated with overall prevalence. risk of ICU admission, 37.3% lower, RR 0.63, p = 0.04, high D levels 148, low D levels 142, OR converted to RR, control prevalance approximated with overall prevalence. Derakhshanian et al., 9/19/2021, retrospective, Iran, Middle East, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Padhi et al., International Immunopharmacology, doi:10.1016/j.intimp.2020.107001 (Peer Reviewed) | Lower levels of vitamin D are associated with SARS-CoV-2 infection and mortality in the Indian population: An observational study |
| Details Analysis of vitamin D levels and COVID-19 in Indian states and union territories, showing an inverse correlation of vitamin D levels with SARS-CoV-2 cases and mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Padhi et al., International Immunopharmacology, doi:10.1016/j.intimp.2020.107001 (Peer Reviewed) |
| Lower levels of vitamin D are associated with SARS-CoV-2 infection and mortality in the Indian population: An observational study |
Analysis of vitamin D levels and COVID-19 in Indian states and union territories, showing an inverse correlation of vitamin D levels with SARS-CoV-2 cases and mortality. 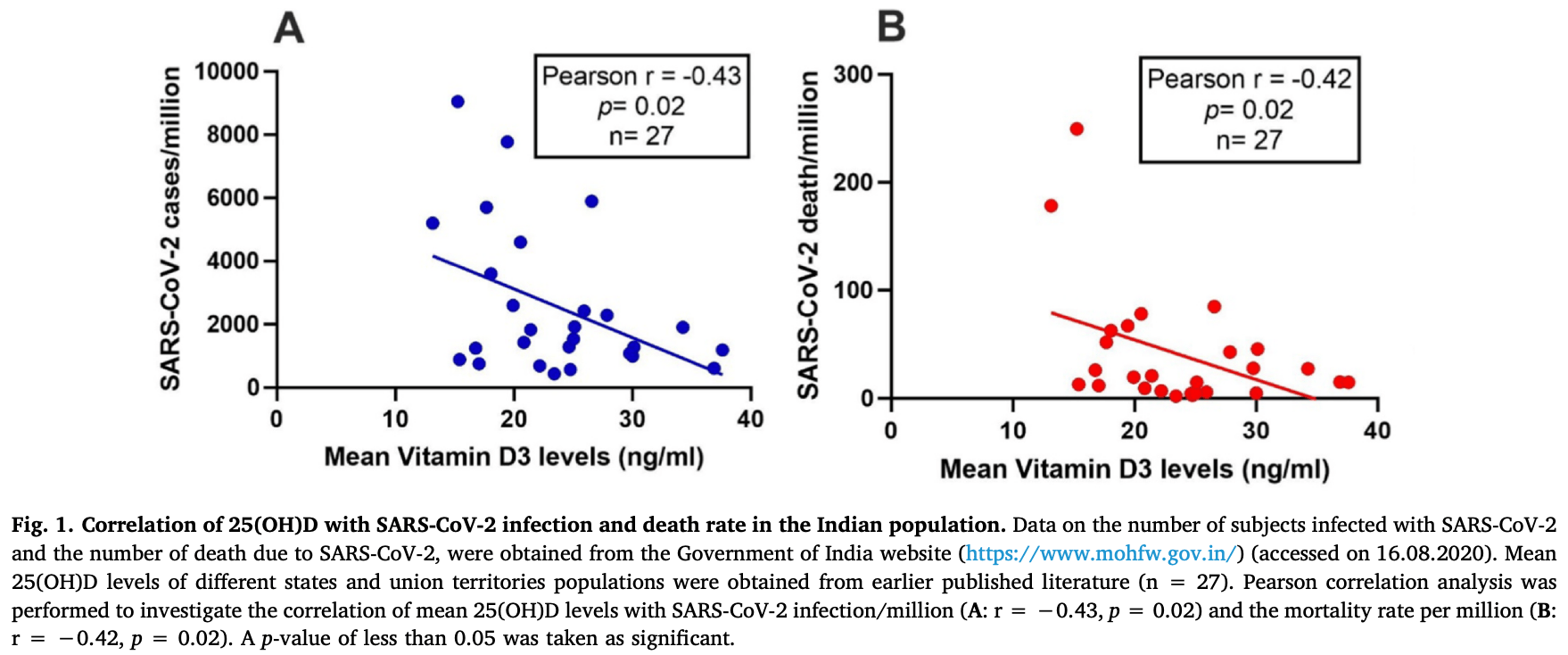 Padhi et al., 9/14/2021, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| In Vitro | Pickard et al., PLOS Pathogens, doi:10.1371/journal.ppat.1009840 (Peer Reviewed) (In Vitro) | in vitro | Discovery of re-purposed drugs that slow SARS-CoV-2 replication in human cells |
| Details In Vitro studying identifying 35 compounds that inhibit SARS-CoV-2 in Vero cells and hepatocytes when treated prior to infection, and several compounds that slow replication when treated after infection: vitamin D, amodiaquine, atovaquone.. |
| Details Source PDF In Vitro In Vitro |
| Pickard et al., PLOS Pathogens, doi:10.1371/journal.ppat.1009840 (Peer Reviewed) (In Vitro) |
| Discovery of re-purposed drugs that slow SARS-CoV-2 replication in human cells |
In Vitro studying identifying 35 compounds that inhibit SARS-CoV-2 in Vero cells and hepatocytes when treated prior to infection, and several compounds that slow replication when treated after infection: vitamin D, amodiaquine, atovaquone, bedaquiline, ebastine, LY2835219, manidipine, and panobinosta. Authors use a nano-luciferase tagged version of the virus to quantify viral load. 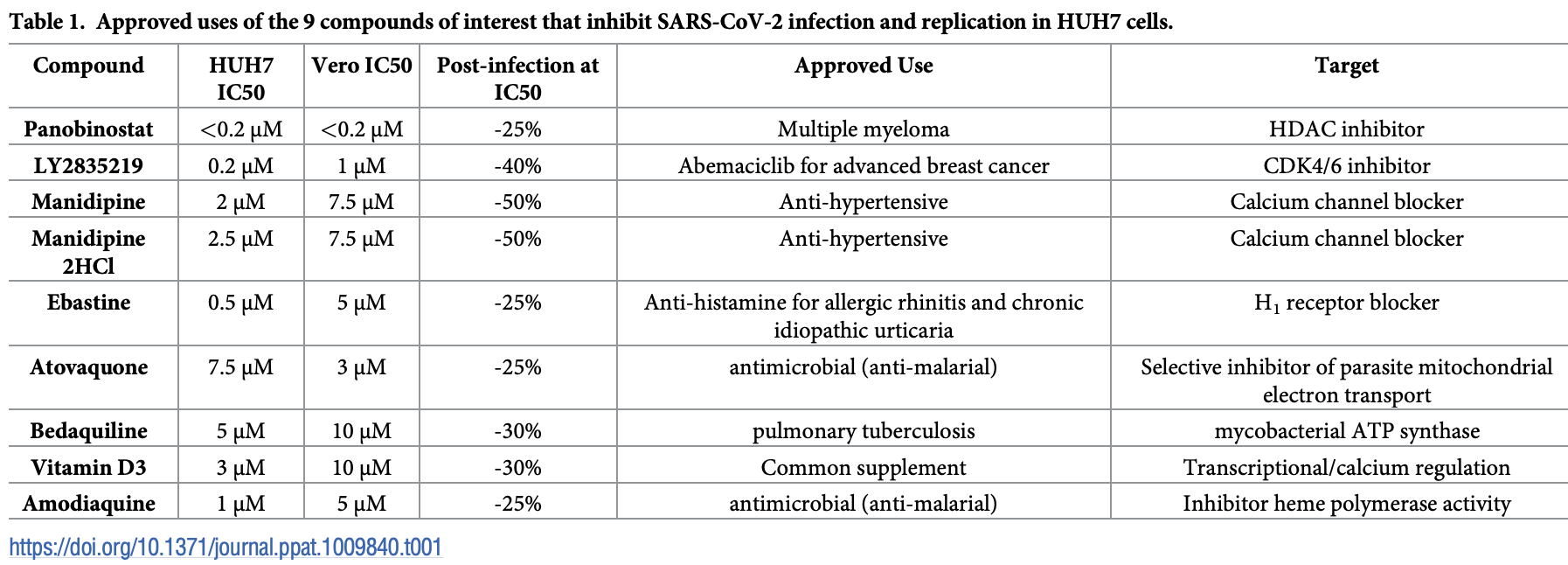 Pickard et al., 9/9/2021, peer-reviewed, 7 authors. In Vitro studies are an important part of preclinical research, however results may be very different in vivo. |
| Submit Corrections or Comments |
| Late | Elamir et al., Bone, doi:10.1016/j.bone.2021.116175 (Peer Reviewed) | death, ↓85.7%, p=0.23 | A Randomized Pilot Study Using Calcitriol in Hospitalized Patients |
| Details RCT 50 hospitalized patients in the USA, 25 treated with calcitriol, showing significantly improved oxygenation with treatment. Mortality, intubation, ICU admission, and hospitalization time also favored treatment, while not reaching stat.. |
| Details Source PDF Late treatment study Late treatment study |
| Elamir et al., Bone, doi:10.1016/j.bone.2021.116175 (Peer Reviewed) |
| A Randomized Pilot Study Using Calcitriol in Hospitalized Patients |
RCT 50 hospitalized patients in the USA, 25 treated with calcitriol, showing significantly improved oxygenation with treatment. Mortality, intubation, ICU admission, and hospitalization time also favored treatment, while not reaching statistical significance with the very small sample size. 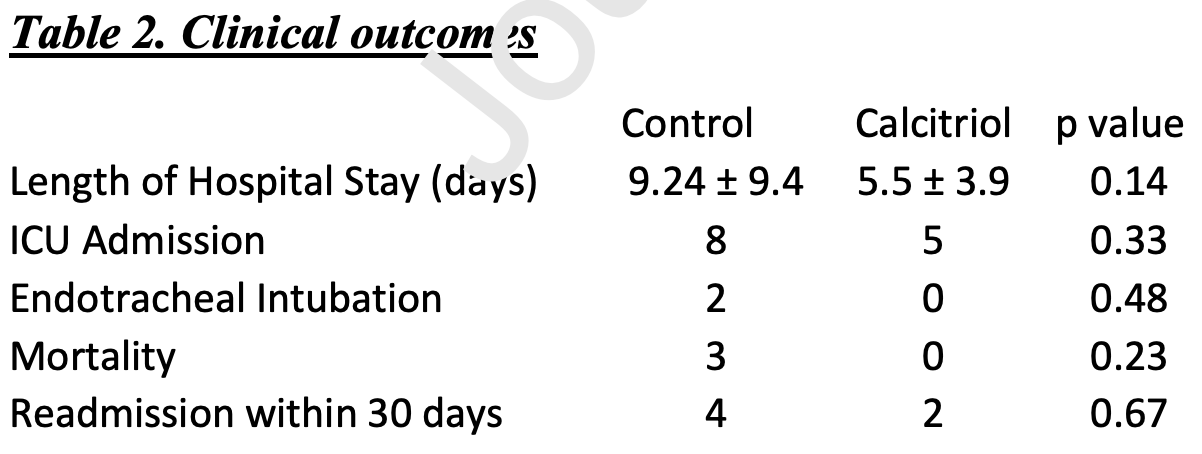 risk of death, 85.7% lower, RR 0.14, p = 0.23, treatment 0 of 25 (0.0%), control 3 of 25 (12.0%), relative risk is not 0 because of continuity correction due to zero events. risk of mechanical ventilation, 80.0% lower, RR 0.20, p = 0.48, treatment 0 of 25 (0.0%), control 2 of 25 (8.0%), relative risk is not 0 because of continuity correction due to zero events. risk of ICU admission, 37.5% lower, RR 0.62, p = 0.33, treatment 5 of 25 (20.0%), control 8 of 25 (32.0%). hospitalization time, 40.5% lower, relative time 0.60, p = 0.14, treatment 25, control 25. relative Δ SaO2/FiO2, RR 0.14, p = 0.03, treatment 25, control 25. Elamir et al., 9/8/2021, Randomized Controlled Trial, USA, North America, peer-reviewed, 9 authors, dosage calcitriol 0.5μg days 1-14. |
| Submit Corrections or Comments |
| PrEPPEP | Lázaro et al., Endocrine Abstracts, doi:10.1530/endoabs.70.EP552 (Preprint) | cases, ↓26.8%, p=1.00 | Vitamin D deficit in type 2 diabetes patients during COVID-19 lockdown with and without supplementation |
| Details Analysis of 239 consecutive diabetic patients, 97 taking vitamin D supplements, showing significantly higher vitamin D levels in supplemented patients. There was no statistically significant difference in cases based on supplementation, w.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Lázaro et al., Endocrine Abstracts, doi:10.1530/endoabs.70.EP552 (Preprint) |
| Vitamin D deficit in type 2 diabetes patients during COVID-19 lockdown with and without supplementation |
Analysis of 239 consecutive diabetic patients, 97 taking vitamin D supplements, showing significantly higher vitamin D levels in supplemented patients. There was no statistically significant difference in cases based on supplementation, with only 3 cases total. risk of case, 26.8% lower, RR 0.73, p = 1.00, treatment 1 of 97 (1.0%), control 2 of 142 (1.4%). Excluded in after exclusion results of meta analysis: very few events, unadjusted results with no group details, minimal details provided. Lázaro et al., 9/5/2021, retrospective, Spain, Europe, preprint, 9 authors, dosage not specified. |
| Submit Corrections or Comments |
| PrEPPEP | Bagheri et al., Journal of Family & Reproductive Health, doi:10.18502/jfrh.v14i3.4668 (Peer Reviewed) | progression, ↓70.9%, p=0.02 | Supplement Usage Pattern in a Group of COVID- 19 Patients in Tehran |
| Details Retrospective 510 patients in Iran, showing lower risk of severity with vitamin D (statistically significant) and zinc (not statistically significant) supplementation. IR.TUMS.VCR.REC.1398.1063. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Bagheri et al., Journal of Family & Reproductive Health, doi:10.18502/jfrh.v14i3.4668 (Peer Reviewed) |
| Supplement Usage Pattern in a Group of COVID- 19 Patients in Tehran |
Retrospective 510 patients in Iran, showing lower risk of severity with vitamin D (statistically significant) and zinc (not statistically significant) supplementation. IR.TUMS.VCR.REC.1398.1063. 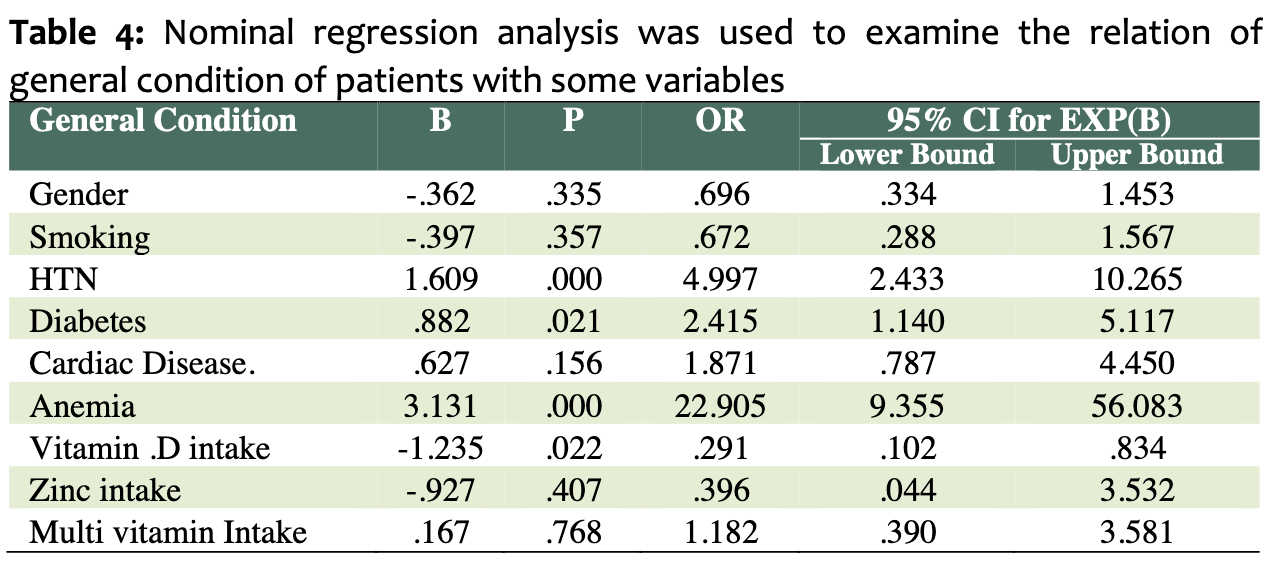 risk of disease progression, 70.9% lower, RR 0.29, p = 0.02, treatment 131, control 379, adjusted, multinomial logistic regression, RR approximated with OR. risk of being in the hospitalized vs. outpatient group, 37.9% lower, RR 0.62, p = 0.11, treatment 28 of 131 (21.4%), control 143 of 379 (37.7%), adjusted, OR converted to RR, binary logistic regression. Bagheri et al., 9/1/2021, retrospective, Iran, Middle East, peer-reviewed, 6 authors, dosage not specified. |
| Submit Corrections or Comments |
| Late | Soliman et al., Proceedings of Singapore Healthcare, doi:10.1177/20101058211041405 (Peer Reviewed) | death, ↓63.4%, p=0.21 | Impact of Vitamin D Therapy on the Progress COVID-19: Six Weeks Follow-Up Study of Vitamin D Deficient Elderly Diabetes Patients |
| Details Small RCT with 56 eldery diabetes patients hospitalized in Egypt, 40 treated with cholecalciferol, not showing significant differences. |
| Details Source PDF Late treatment study Late treatment study |
| Soliman et al., Proceedings of Singapore Healthcare, doi:10.1177/20101058211041405 (Peer Reviewed) |
| Impact of Vitamin D Therapy on the Progress COVID-19: Six Weeks Follow-Up Study of Vitamin D Deficient Elderly Diabetes Patients |
Small RCT with 56 eldery diabetes patients hospitalized in Egypt, 40 treated with cholecalciferol, not showing significant differences. 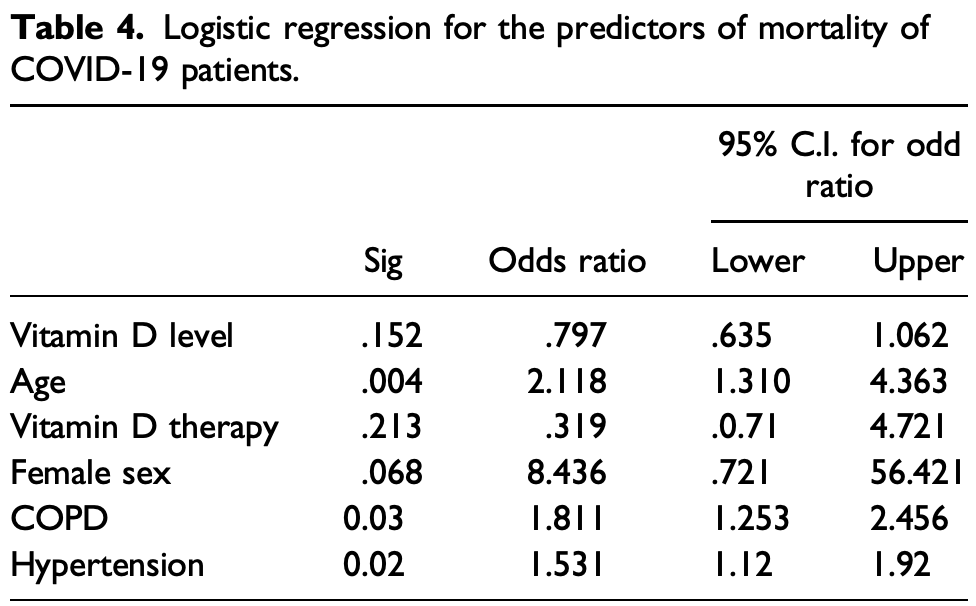 risk of death, 63.4% lower, RR 0.37, p = 0.21, treatment 7 of 40 (17.5%), control 3 of 16 (18.8%), adjusted, OR converted to RR, logistic regression. risk of mechanical ventilation, 20.0% lower, RR 0.80, p = 0.56, treatment 14 of 40 (35.0%), control 7 of 16 (43.8%), unadjusted. risk of no recovery, 20.0% lower, RR 0.80, p = 0.56, treatment 14 of 40 (35.0%), control 7 of 16 (43.8%), unadjusted. Soliman et al., 9/1/2021, Randomized Controlled Trial, Egypt, Africa, peer-reviewed, 3 authors, dosage 200,000IU single dose. |
| Submit Corrections or Comments |
| Meta | Ben-Eltriki et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2021.1951891 (Peer Reviewed) (meta analysis) | meta-analysis | Association between Vitamin D Status and Risk of Developing Severe COVID-19 Infection: A Meta-Analysis of Observational Studies |
| Details Meta analysis of 24 observational studies with 3,637 participants, showing low vitamin D status associated with a higher risk of death and a higher risk of developing severe COVID-19 pneumonia. |
| Details Source PDF Meta Meta |
| Ben-Eltriki et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2021.1951891 (Peer Reviewed) (meta analysis) |
| Association between Vitamin D Status and Risk of Developing Severe COVID-19 Infection: A Meta-Analysis of Observational Studies |
Meta analysis of 24 observational studies with 3,637 participants, showing low vitamin D status associated with a higher risk of death and a higher risk of developing severe COVID-19 pneumonia. 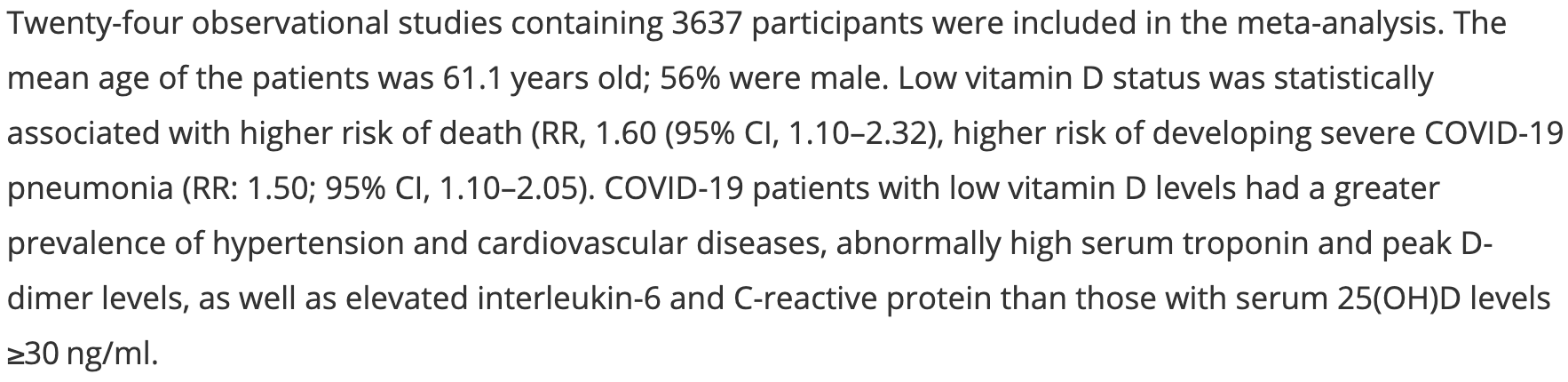 Ben-Eltriki et al., 8/31/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Karonova et al., Nutrients, doi:10.3390/nu13093021 (Peer Reviewed) | death, ↓77.8%, p=0.006 | Low 25(OH)D Level Is Associated with Severe Course and Poor Prognosis in COVID-19 |
| Details Retrospective 161 hospitalized patients in Russia, showing COVID-19 severity and mortality associated with vitamin D deficiency. Patients in this study may overlap with those in an earlier smaller study from some of the same authors. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Karonova et al., Nutrients, doi:10.3390/nu13093021 (Peer Reviewed) |
| Low 25(OH)D Level Is Associated with Severe Course and Poor Prognosis in COVID-19 |
Retrospective 161 hospitalized patients in Russia, showing COVID-19 severity and mortality associated with vitamin D deficiency. Patients in this study may overlap with those in an earlier smaller study from some of the same authors. 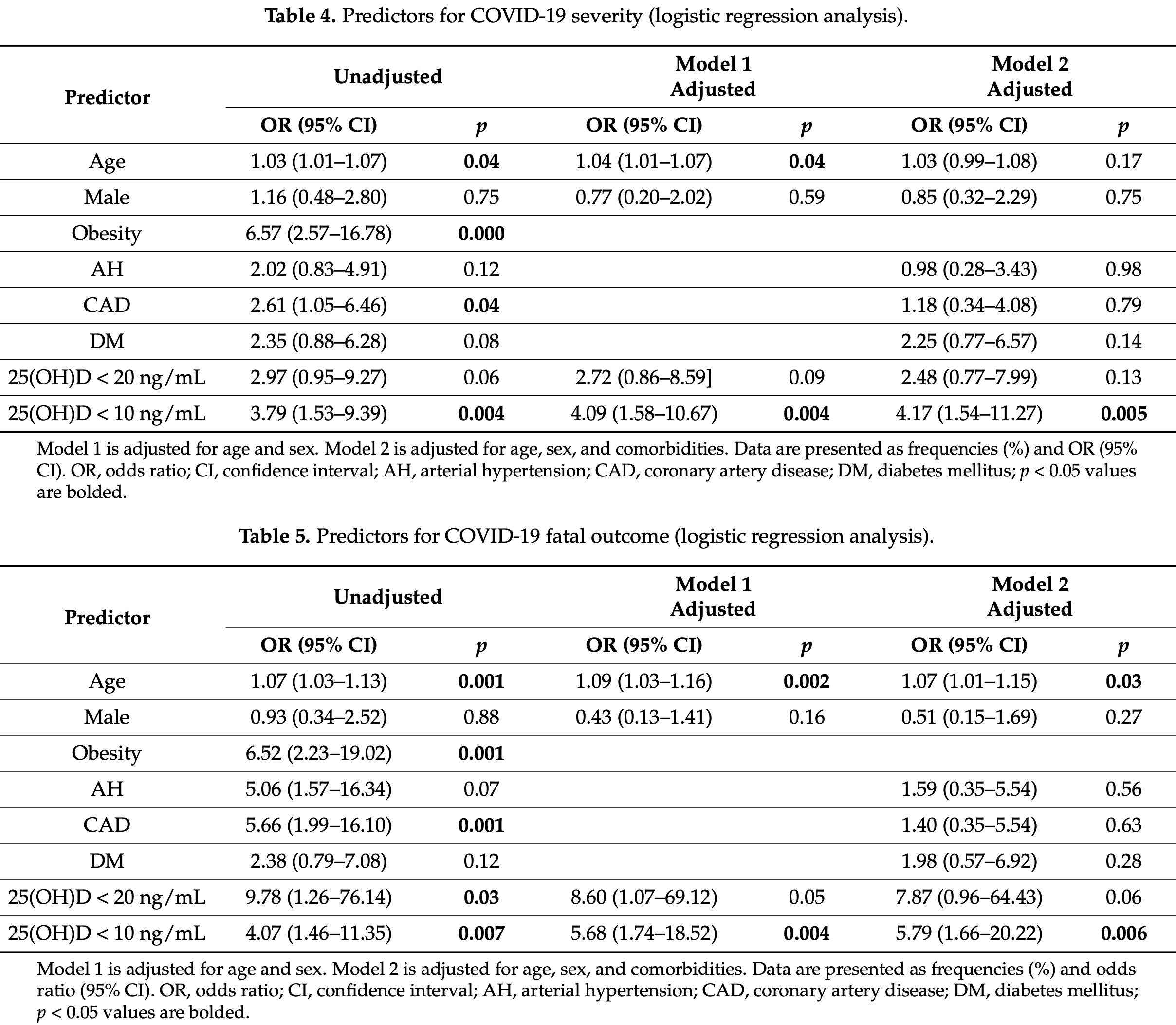 risk of death, 77.8% lower, RR 0.22, p = 0.006, high D levels 8 of 96 (8.3%), low D levels 10 of 37 (27.0%), adjusted, OR converted to RR, >10ng/mL, logistic regression model 2. risk of death, 84.8% lower, RR 0.15, p = 0.06, high D levels 1 of 43 (2.3%), low D levels 17 of 90 (18.9%), adjusted, OR converted to RR, >20ng/mL, logistic regression model 2. risk of severe case, 67.3% lower, RR 0.33, p = 0.005, high D levels 12 of 96 (12.5%), low D levels 13 of 37 (35.1%), adjusted, OR converted to RR, >10ng/mL, logistic regression model 2. risk of severe case, 53.2% lower, RR 0.47, p = 0.13, high D levels 4 of 43 (9.3%), low D levels 21 of 90 (23.3%), adjusted, OR converted to RR, >20ng/mL, logistic regression model 2. Karonova et al., 8/29/2021, retrospective, Russia, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Late | Assiri et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.08.030 (Peer Reviewed) | death, ↑66.5%, p=0.60 | COVID-19 related treatment and outcomes among COVID-19 ICU patients: A retrospective cohort study |
| Details Retrospective 118 ICU patients in Saudi Arabia showing no significant differences in unadjusted results with zinc, vitamin D, and favipiravir treatment. |
| Details Source PDF Late treatment study Late treatment study |
| Assiri et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.08.030 (Peer Reviewed) |
| COVID-19 related treatment and outcomes among COVID-19 ICU patients: A retrospective cohort study |
Retrospective 118 ICU patients in Saudi Arabia showing no significant differences in unadjusted results with zinc, vitamin D, and favipiravir treatment. 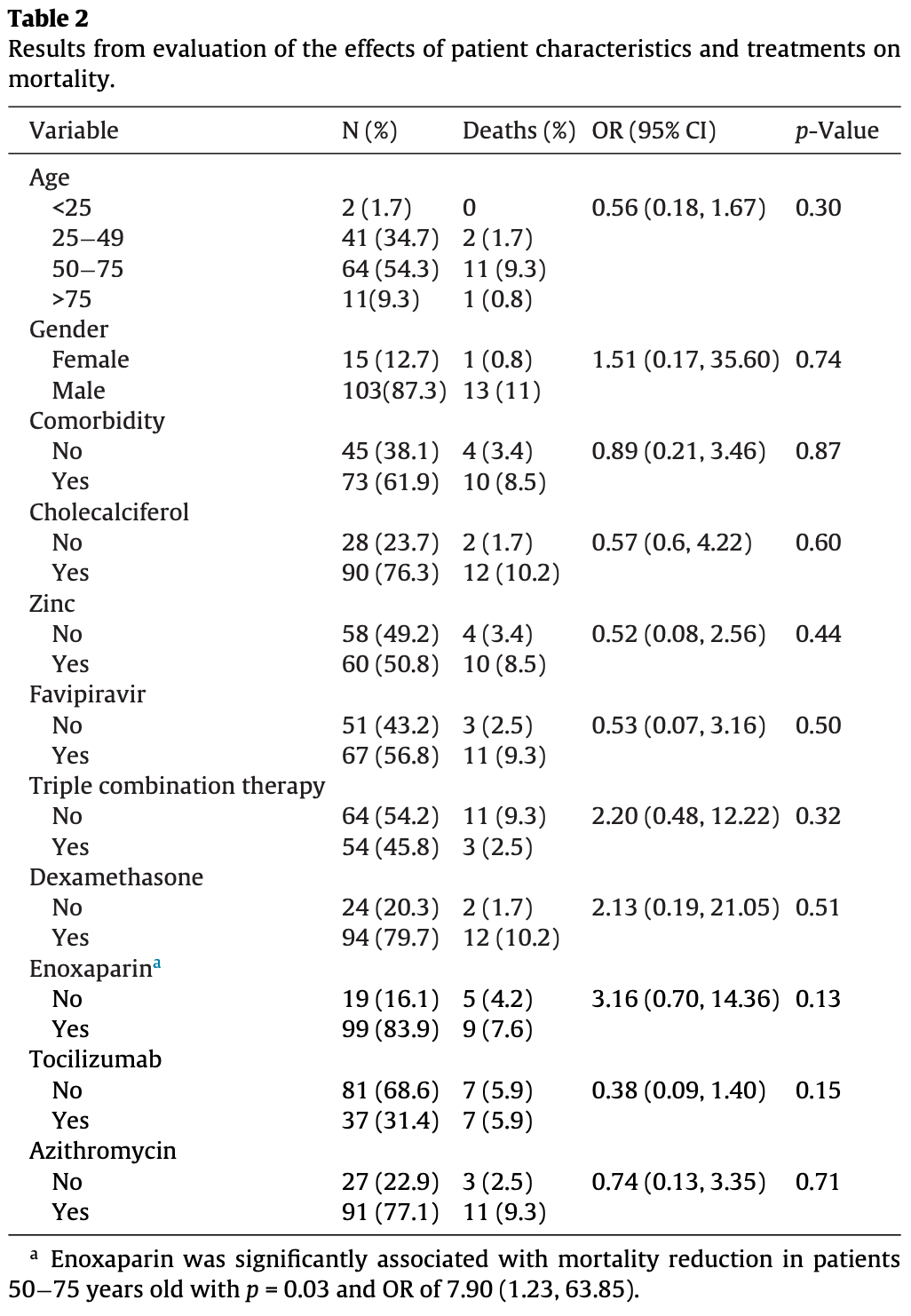 risk of death, 66.5% higher, RR 1.66, p = 0.60, treatment 12 of 90 (13.3%), control 2 of 28 (7.1%), OR converted to RR. Excluded in after exclusion results of meta analysis: unadjusted results with no group details. Assiri et al., 8/28/2021, retrospective, Saudi Arabia, Middle East, peer-reviewed, 8 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Pecina et al., Journal of Primary Care & Community Health, doi:10.1177/21501327211041206 (Peer Reviewed) | death, ↓35.9%, p=0.74 | Vitamin D Status and Severe COVID-19 Disease Outcomes in Hospitalized Patients |
| Details Retrospective 92 hospitalized patients not showing significant differences in outcomes based on vitamin D status or supplementation. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Pecina et al., Journal of Primary Care & Community Health, doi:10.1177/21501327211041206 (Peer Reviewed) |
| Vitamin D Status and Severe COVID-19 Disease Outcomes in Hospitalized Patients |
Retrospective 92 hospitalized patients not showing significant differences in outcomes based on vitamin D status or supplementation. 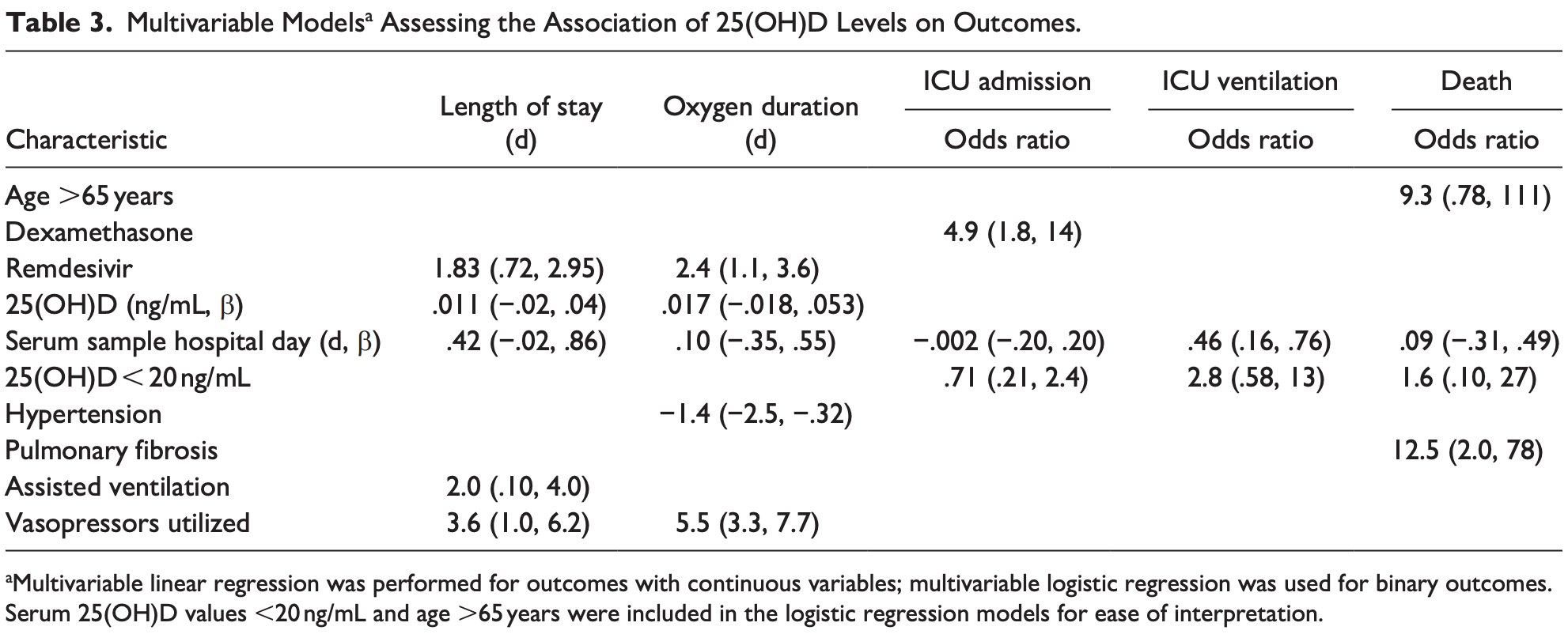 risk of death, 35.9% lower, RR 0.64, p = 0.74, high D levels 6 of 77 (7.8%), low D levels 1 of 15 (6.7%), OR converted to RR, >20ng/mL, multivariable logistic regression. risk of mechanical ventilation, 56.9% lower, RR 0.43, p = 0.22, high D levels 8 of 15 (53.3%), low D levels 4 of 15 (26.7%), OR converted to RR, >20ng/mL, multivariable logistic regression. risk of ICU admission, 13.1% higher, RR 1.13, p = 0.57, high D levels 54 of 77 (70.1%), low D levels 9 of 15 (60.0%), OR converted to RR, >20ng/mL, multivariable logistic regression. Pecina et al., 8/27/2021, retrospective, USA, North America, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Golabi et al., Nutrients, doi:10.3390/nu13103368 (preprint 8/26/2021) (Peer Reviewed) | cases, ↑25.4%, p=0.56 | The Association between Vitamin D and Zinc Status and the Progression of Clinical Symptoms among Outpatients Infected with SARS-CoV-2 and Potentially Non-Infected Participants: A Cross-Sectional Study |
| Details Analysis of vitamin D and zinc levels in 53 PCR+ outpatients and 53 matched controls, showing lower zinc levels in COVID-19 patients, and increased risk of cases and symptoms with vitamin D deficiency. There was no significant difference .. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Golabi et al., Nutrients, doi:10.3390/nu13103368 (preprint 8/26/2021) (Peer Reviewed) |
| The Association between Vitamin D and Zinc Status and the Progression of Clinical Symptoms among Outpatients Infected with SARS-CoV-2 and Potentially Non-Infected Participants: A Cross-Sectional Study |
Analysis of vitamin D and zinc levels in 53 PCR+ outpatients and 53 matched controls, showing lower zinc levels in COVID-19 patients, and increased risk of cases and symptoms with vitamin D deficiency. There was no significant difference in the use of supplements between cases and controls. IR.ABADANUMS.REC.1399.073. risk of case, 25.4% higher, RR 1.25, p = 0.56, treatment 28 of 53 (52.8%) cases, 25 of 53 (47.2%) controls, case control OR. Golabi et al., 8/26/2021, retrospective, Iran, Middle East, peer-reviewed, 10 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Golabi et al., Nutrients, doi:10.3390/nu13103368 (preprint 8/26/2021) (Peer Reviewed) | symp., ↓90.0%, p<0.0001 | The Association between Vitamin D and Zinc Status and the Progression of Clinical Symptoms among Outpatients Infected with SARS-CoV-2 and Potentially Non-Infected Participants: A Cross-Sectional Study |
| Details Analysis of vitamin D and zinc levels in 53 PCR+ outpatients and 53 matched controls, showing lower zinc levels in COVID-19 patients, and increased risk of cases and symptoms with vitamin D deficiency. There was no significant difference .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Golabi et al., Nutrients, doi:10.3390/nu13103368 (preprint 8/26/2021) (Peer Reviewed) |
| The Association between Vitamin D and Zinc Status and the Progression of Clinical Symptoms among Outpatients Infected with SARS-CoV-2 and Potentially Non-Infected Participants: A Cross-Sectional Study |
Analysis of vitamin D and zinc levels in 53 PCR+ outpatients and 53 matched controls, showing lower zinc levels in COVID-19 patients, and increased risk of cases and symptoms with vitamin D deficiency. There was no significant difference in the use of supplements between cases and controls. IR.ABADANUMS.REC.1399.073. 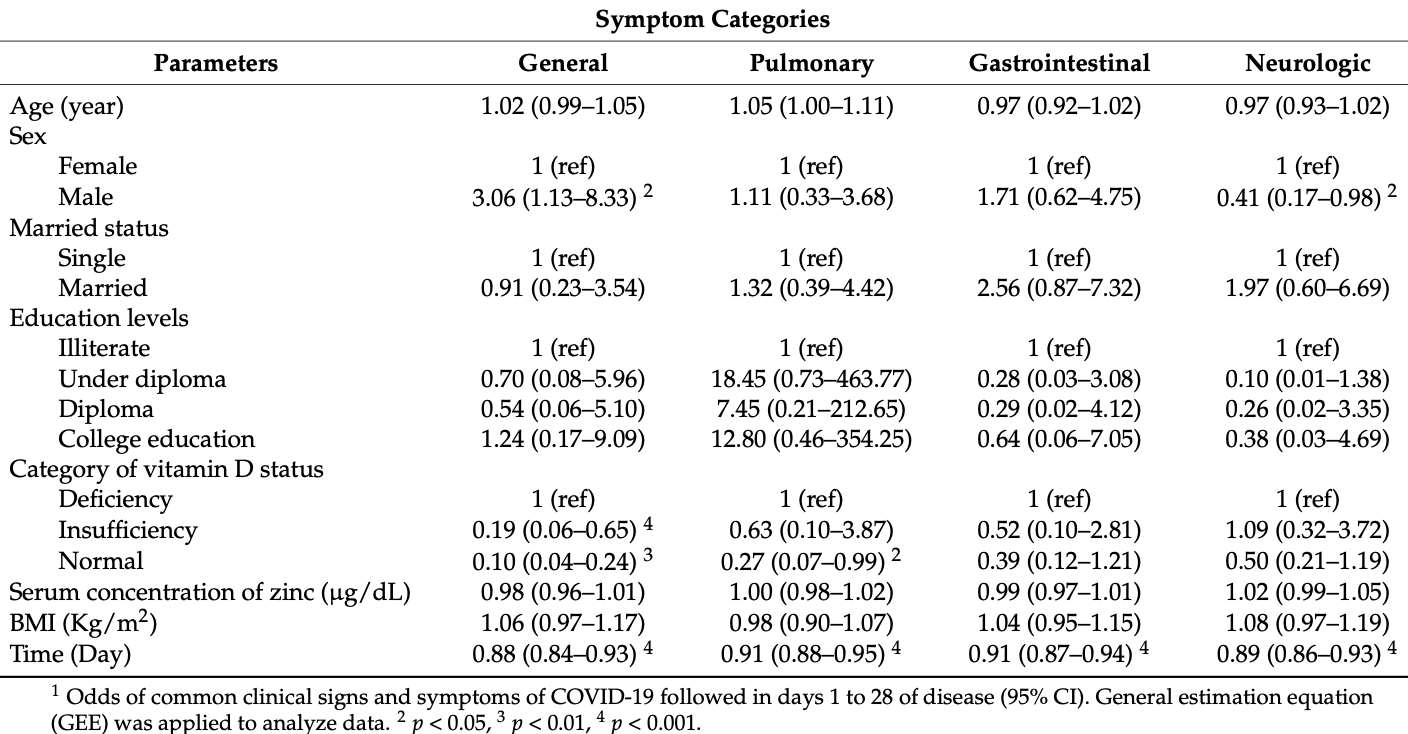 odds of symptoms, 90.0% lower, RR 0.10, p < 0.001, high D levels 34, low D levels 10, >30ng/mL vs. <20ng/mL, GEE regression, RR approximated with OR. odds of symptoms, 81.0% lower, RR 0.19, p = 0.006, high D levels 34, low D levels 9, 20-30ng/mL vs. <20ng/mL, GEE regression, RR approximated with OR. risk of case, 71.7% lower, RR 0.28, p = 0.07, high D levels 34 of 44 (77.3%) cases, 36 of 39 (92.3%) controls, case control OR, >30ng/mL vs. <20ng/mL. Golabi et al., 8/26/2021, retrospective, Iran, Middle East, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Meta | Varikasuvu (Preprint) (meta analysis) | meta-analysis | COVID-19 and Vitamin D (Co-VIVID Study): a systematic review and meta-analysis of randomized controlled trials |
| Details Meta analysis of 6 vitamin D treatment RCTs, showing statistically significant improvements for pooled outcomes and PCR positivity, and positive but not statistically significant improvements for mortality, mechanical ventilation, ICU adm.. |
| Details Source PDF Meta Meta |
| Varikasuvu (Preprint) (meta analysis) |
| COVID-19 and Vitamin D (Co-VIVID Study): a systematic review and meta-analysis of randomized controlled trials |
Meta analysis of 6 vitamin D treatment RCTs, showing statistically significant improvements for pooled outcomes and PCR positivity, and positive but not statistically significant improvements for mortality, mechanical ventilation, ICU admission, and severity. 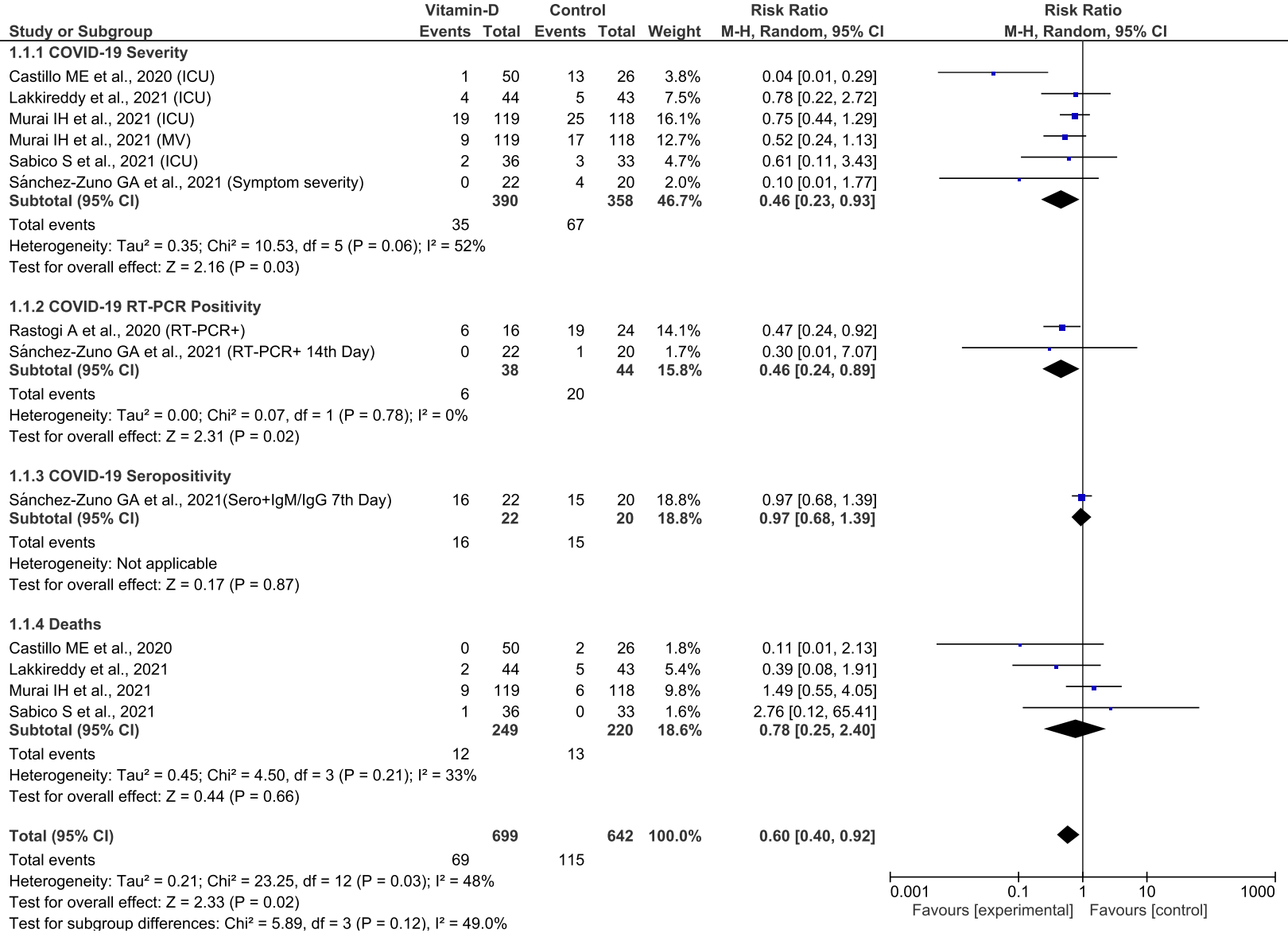 Varikasuvu et al., 8/25/2021, preprint, 3 authors. |
| Submit Corrections or Comments |
| In Silico | Song et al., Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1964601 (Peer Reviewed) | Vitamin D3 and its hydroxyderivatives as promising drugs against COVID-19: a computational study |
| Details In Silico study suggesting that vitamin D3 and its biologically active hydroxyderivatives can serve as an TMPRSS2 inhibitor, and inhibit ACE2 binding with the SARS-CoV-2 RBD. |
| Details Source PDF In Silico In Silico |
| Song et al., Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1964601 (Peer Reviewed) |
| Vitamin D3 and its hydroxyderivatives as promising drugs against COVID-19: a computational study |
In Silico study suggesting that vitamin D3 and its biologically active hydroxyderivatives can serve as an TMPRSS2 inhibitor, and inhibit ACE2 binding with the SARS-CoV-2 RBD. 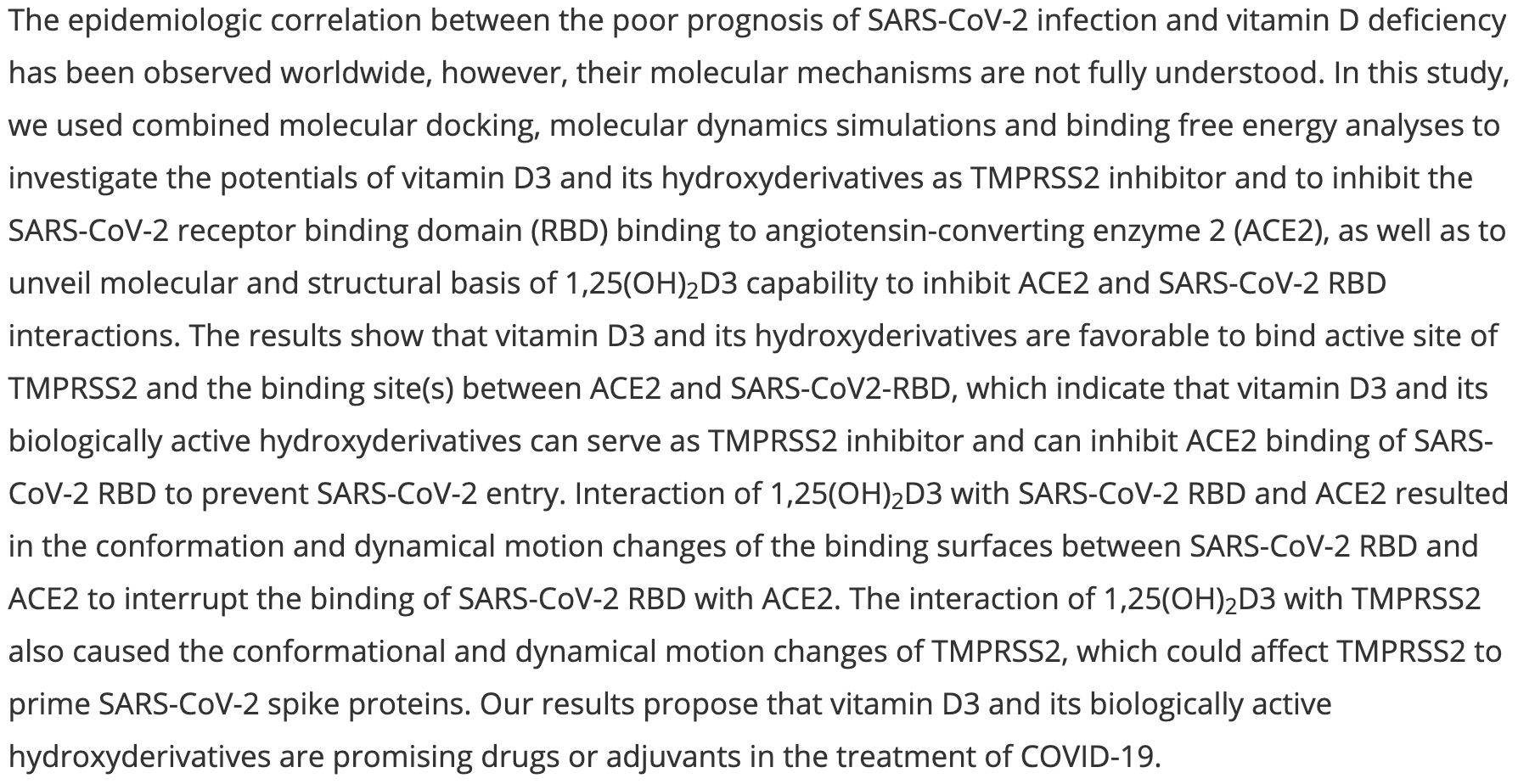 Song et al., 8/20/2021, peer-reviewed, 7 authors. In Silico studies are an important part of preclinical research, however results may be very different in vivo. |
| Submit Corrections or Comments |
| Levels | Shakeri et al., Journal of Medical Virology, doi:10.1002/jmv.27277 (Peer Reviewed) | Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19 |
| Details Retrospective 293 hospitalized patients in Iran showing lower levels of zinc, vitamin B12, and vitamin D in patients that died, with statistical significance reached only for zinc. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Shakeri et al., Journal of Medical Virology, doi:10.1002/jmv.27277 (Peer Reviewed) |
| Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19 |
Retrospective 293 hospitalized patients in Iran showing lower levels of zinc, vitamin B12, and vitamin D in patients that died, with statistical significance reached only for zinc. 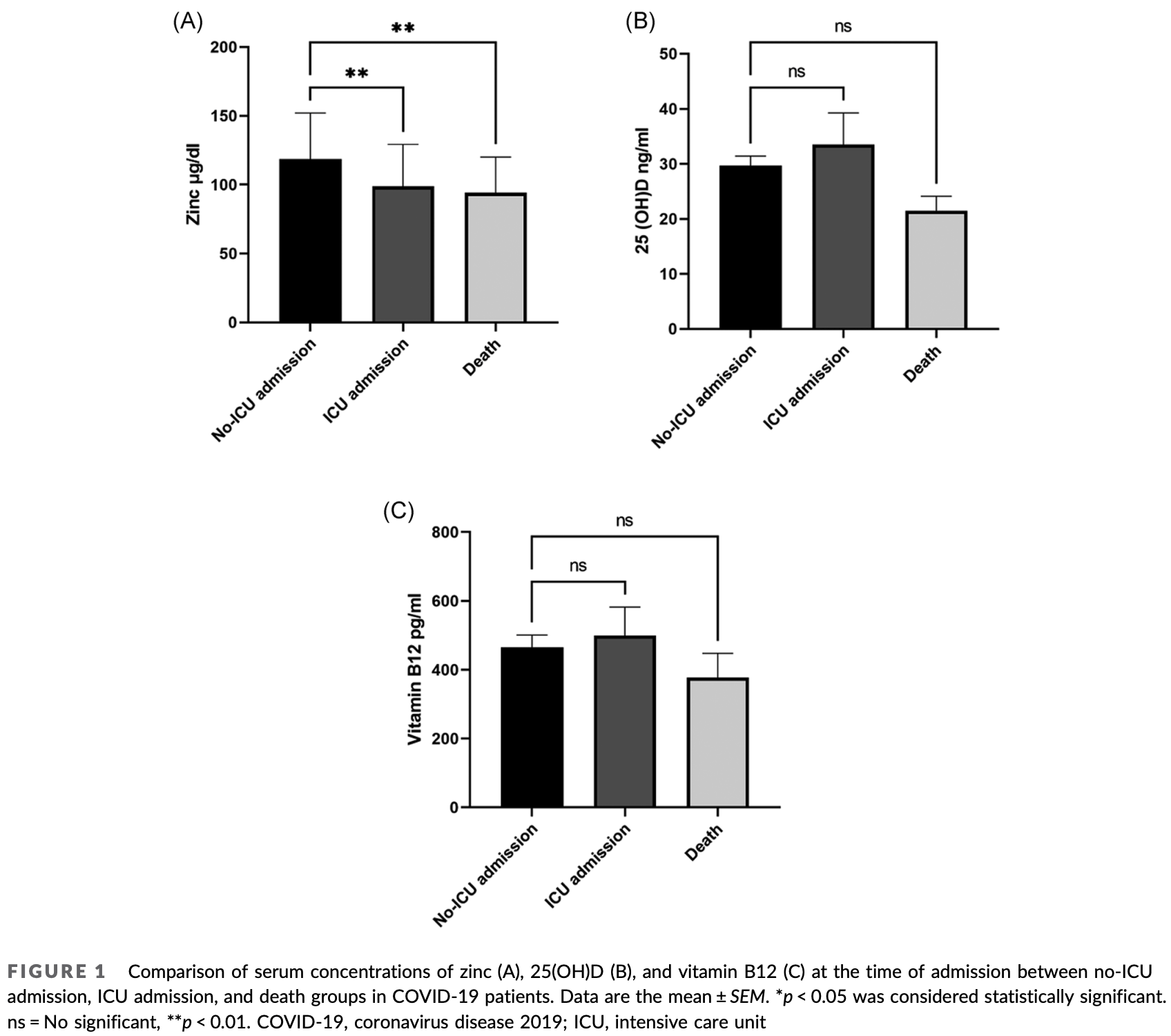 Shakeri et al., 8/18/2021, Iran, Middle East, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Levels | di Filippo et al, The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab599 (Peer Reviewed) | death, ↓10.7%, p=1.00 | Vitamin D levels associate with blood glucose and BMI in COVID-19 patients predicting disease severity |
| Details Retrospective 88 patients in Italy, showing vitamin D deficiency associated with severe cases, blood glucose, and BMI. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| di Filippo et al, The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab599 (Peer Reviewed) |
| Vitamin D levels associate with blood glucose and BMI in COVID-19 patients predicting disease severity |
Retrospective 88 patients in Italy, showing vitamin D deficiency associated with severe cases, blood glucose, and BMI. 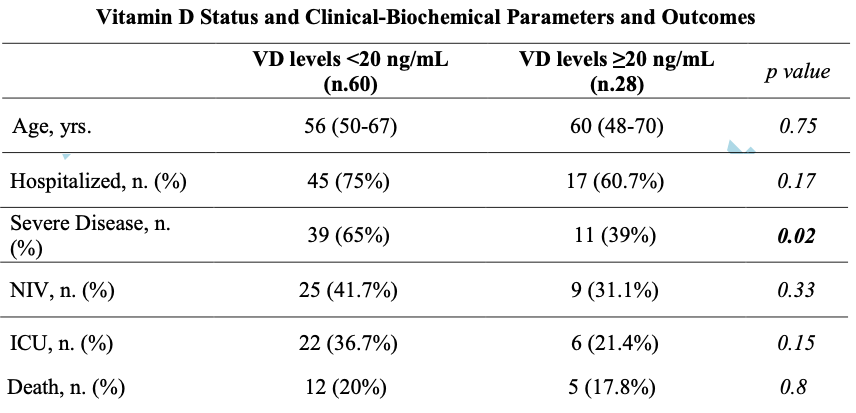 risk of death, 10.7% lower, RR 0.89, p = 1.00, high D levels 5 of 28 (17.9%), low D levels 12 of 60 (20.0%), >20ng/mL. risk of ICU admission, 41.6% lower, RR 0.58, p = 0.22, high D levels 6 of 28 (21.4%), low D levels 22 of 60 (36.7%), >20ng/mL. risk of severe case, 39.6% lower, RR 0.60, p = 0.04, high D levels 11 of 28 (39.3%), low D levels 39 of 60 (65.0%), >20ng/mL. di Filippo et al., 8/12/2021, retrospective, Italy, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Sinaci et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105964 (Peer Reviewed) | m/s case, ↓79.5%, p<0.0001 | Impact of vitamin D on the course of COVID-19 during pregnancy: A case control study |
| Details Retrospective 159 COVID-19+ pregnant women in Turkey and 332 healthy pregnant controls, showing significantly lower vitamin D levels in COVID-19+ patients. 23% of COVID-19 patients where on vitamin D supplementation, while none of the 7 s.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Sinaci et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105964 (Peer Reviewed) |
| Impact of vitamin D on the course of COVID-19 during pregnancy: A case control study |
Retrospective 159 COVID-19+ pregnant women in Turkey and 332 healthy pregnant controls, showing significantly lower vitamin D levels in COVID-19+ patients. 23% of COVID-19 patients where on vitamin D supplementation, while none of the 7 severe cases were on supplementation. 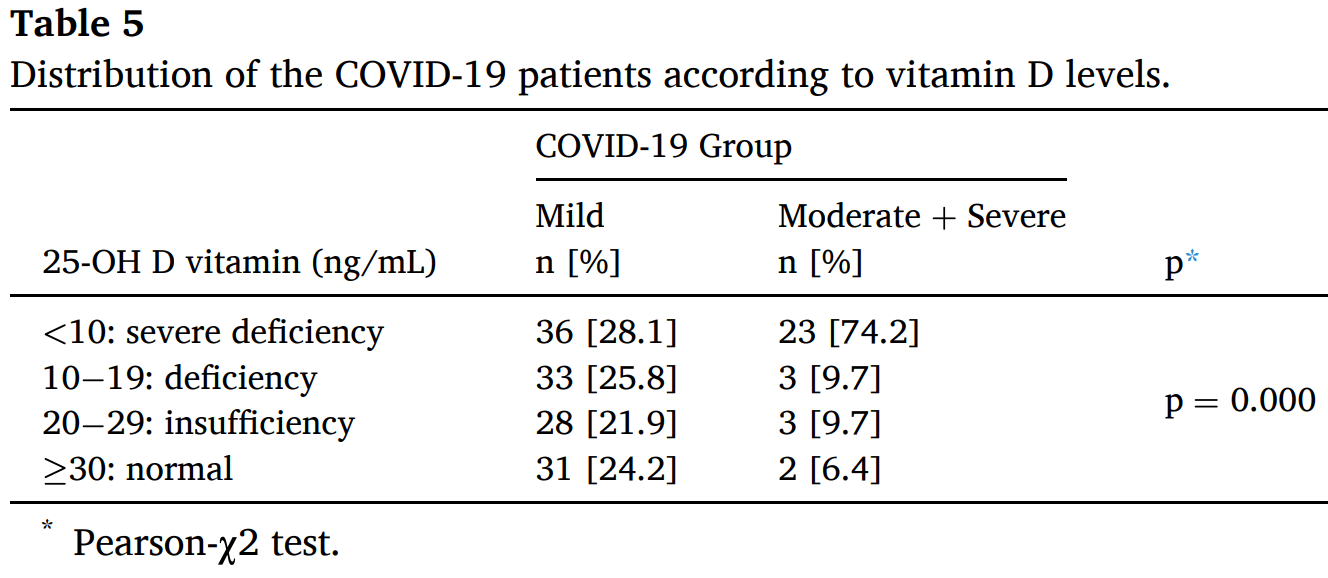 risk of moderate/severe case, 79.5% lower, RR 0.21, p < 0.001, high D levels 8 of 100 (8.0%), low D levels 23 of 59 (39.0%), >10ng/mL. risk of case, 59.9% lower, RR 0.40, p < 0.001, high D levels 100 of 397 (25.2%), low D levels 59 of 94 (62.8%), >10ng/mL. Sinaci et al., 8/11/2021, retrospective, Turkey, Europe, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Levels | Alpcan et al., Epidemiology & Infection, doi:10.1017/S0950268821001825 (Peer Reviewed) | cases, ↓73.0%, p=0.0005 | Vitamin D levels in children with COVID-19: a report from Turkey |
| Details Retrospective 75 COVID-19 hospitalized pediatric patients in Turkey and 80 healthy controls, showing significantly lower vitamin D levels in COVID-19 patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Alpcan et al., Epidemiology & Infection, doi:10.1017/S0950268821001825 (Peer Reviewed) |
| Vitamin D levels in children with COVID-19: a report from Turkey |
Retrospective 75 COVID-19 hospitalized pediatric patients in Turkey and 80 healthy controls, showing significantly lower vitamin D levels in COVID-19 patients. 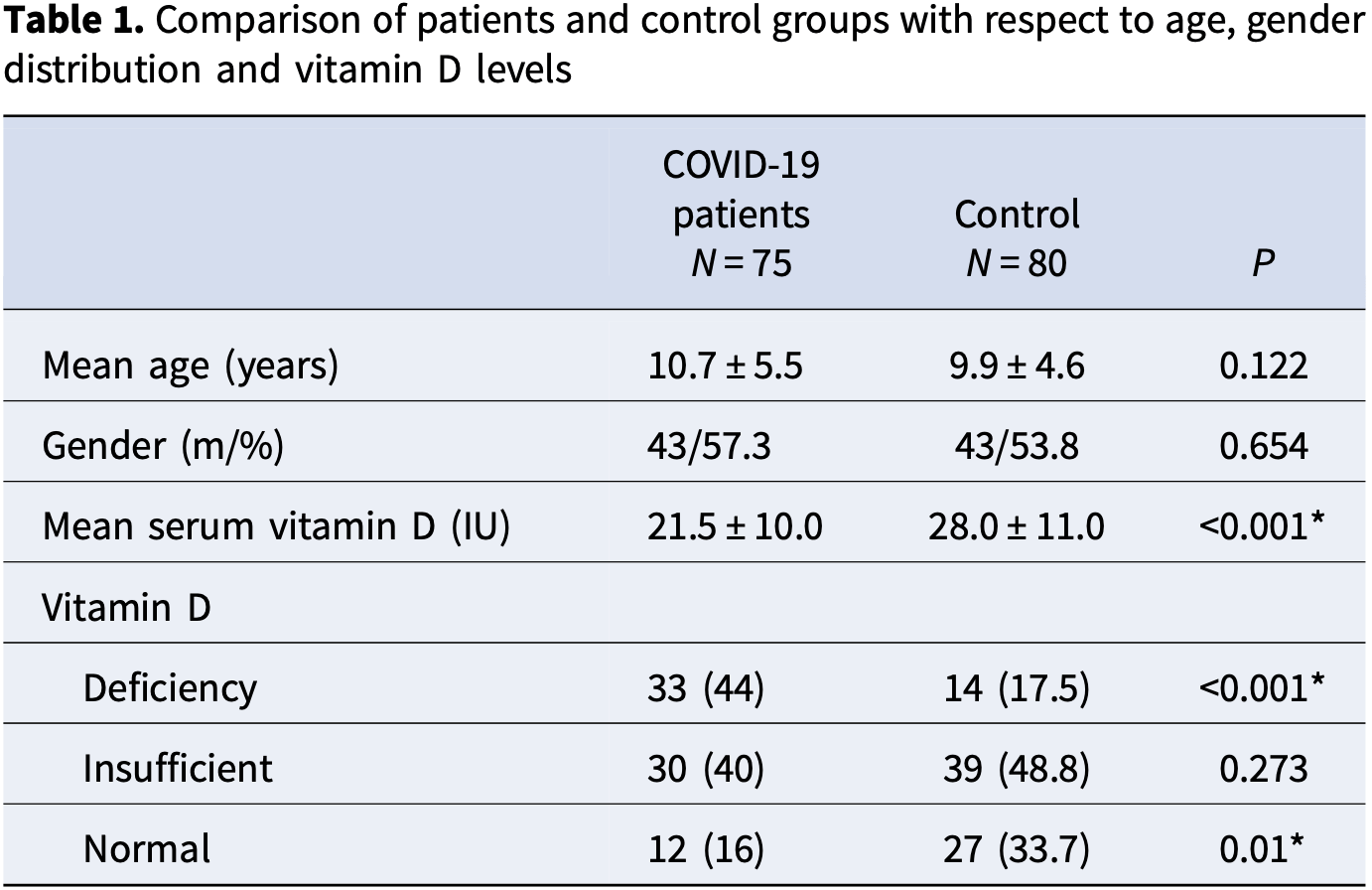 risk of case, 73.0% lower, RR 0.27, p < 0.001, high D levels 42 of 75 (56.0%) cases, 66 of 80 (82.5%) controls, case control OR, >20ng/mL. Alpcan et al., 8/10/2021, retrospective, Turkey, Europe, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Eden et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000270 (Peer Reviewed) | death, ↓63.9%, p=0.10 | Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: a retrospective single-centre service evaluation |
| Details Retrospective 72 ICU patients in the UK, showing higher mortality with vitamin D deficiency, not reaching statistical significance. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Eden et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000270 (Peer Reviewed) |
| Nutritional parameters and outcomes in patients admitted to intensive care with COVID-19: a retrospective single-centre service evaluation |
Retrospective 72 ICU patients in the UK, showing higher mortality with vitamin D deficiency, not reaching statistical significance. 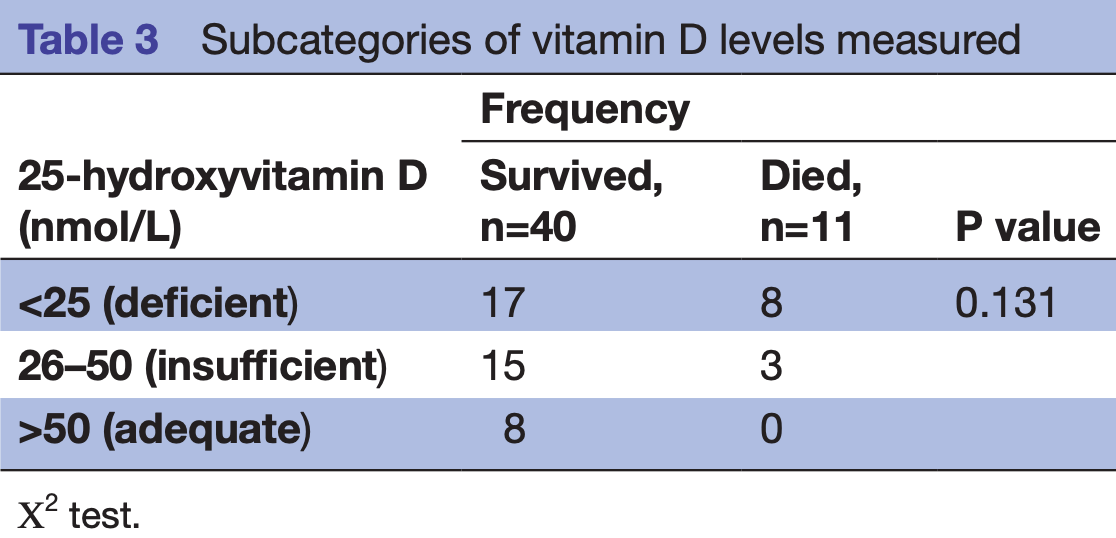 risk of death, 63.9% lower, RR 0.36, p = 0.10, high D levels (≥25nmol/L) 3 of 26 (11.5%), low D levels (<25nmol/L) 8 of 25 (32.0%). risk of death, 92.9% lower, RR 0.07, p = 0.18, high D levels (≥50nmol/L) 0 of 8 (0.0%), low D levels (<50nmol/L) 11 of 43 (25.6%), relative risk is not 0 because of continuity correction due to zero events. Eden et al., 8/5/2021, retrospective, United Kingdom, Europe, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Ribeiro et al., Clinica Chimica Acta, doi:10.1016/j.cca.2021.08.003 (Peer Reviewed) | cases, ↓50.5%, p=0.01 | Previous vitamin D status and total cholesterol are associated with SARS-CoV-2 infection |
| Details Retrospective 1,634 patients tested for SARS-CoV-2 in Brazil, showing vitamin D levels <30ng/mL associated with greater odds of a positive SARS-CoV-2 test in patients older than 49 years. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ribeiro et al., Clinica Chimica Acta, doi:10.1016/j.cca.2021.08.003 (Peer Reviewed) |
| Previous vitamin D status and total cholesterol are associated with SARS-CoV-2 infection |
Retrospective 1,634 patients tested for SARS-CoV-2 in Brazil, showing vitamin D levels <30ng/mL associated with greater odds of a positive SARS-CoV-2 test in patients older than 49 years. 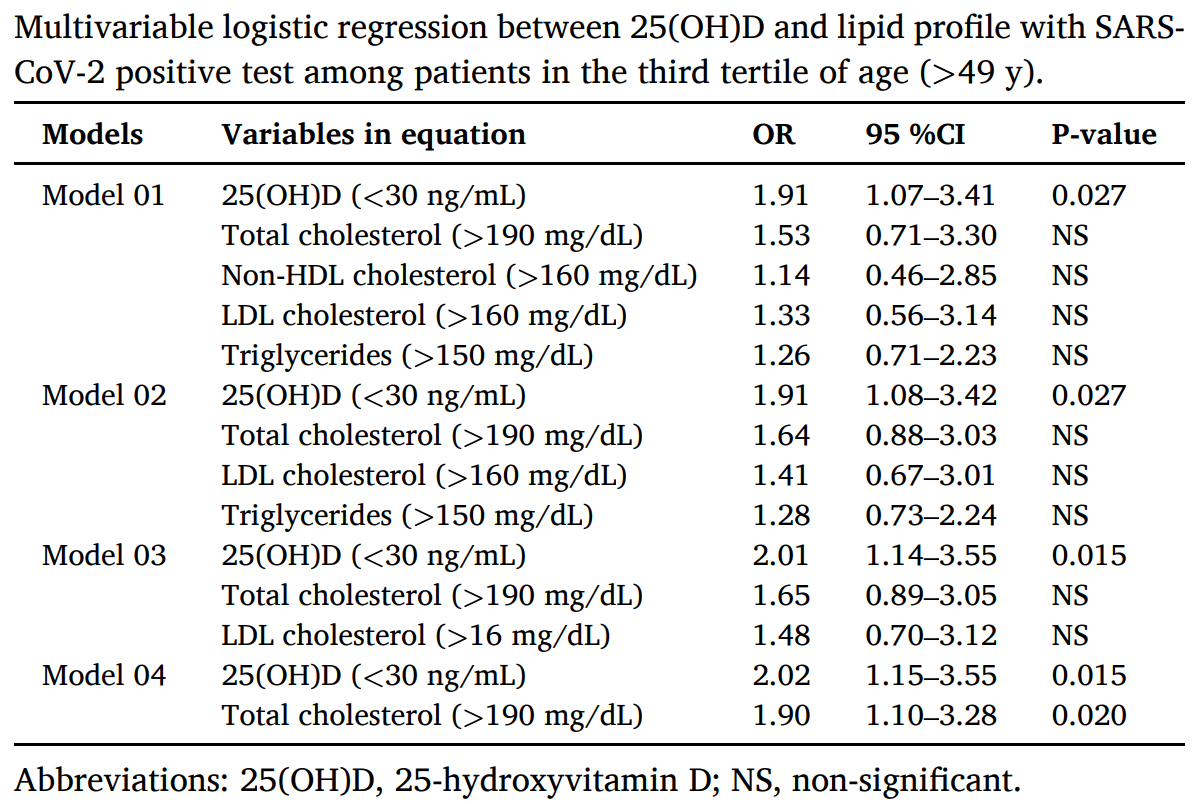 risk of case, 50.5% lower, RR 0.50, p = 0.01, >30ng/mL, multivariate, RR approximated with OR. Ribeiro et al., 8/5/2021, retrospective, Brazil, South America, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Nimavat et al., Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102661 (Peer Reviewed) | death, ↓50.4%, p=0.17 | Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India |
| Details Case control study with 156 PCR+ cases in India and 204 controls, showing more frequent vitamin D deficiency in COVID-19 patients, and an association between lower vitamin D levels and COVID-19 severity. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Nimavat et al., Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102661 (Peer Reviewed) |
| Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India |
Case control study with 156 PCR+ cases in India and 204 controls, showing more frequent vitamin D deficiency in COVID-19 patients, and an association between lower vitamin D levels and COVID-19 severity. 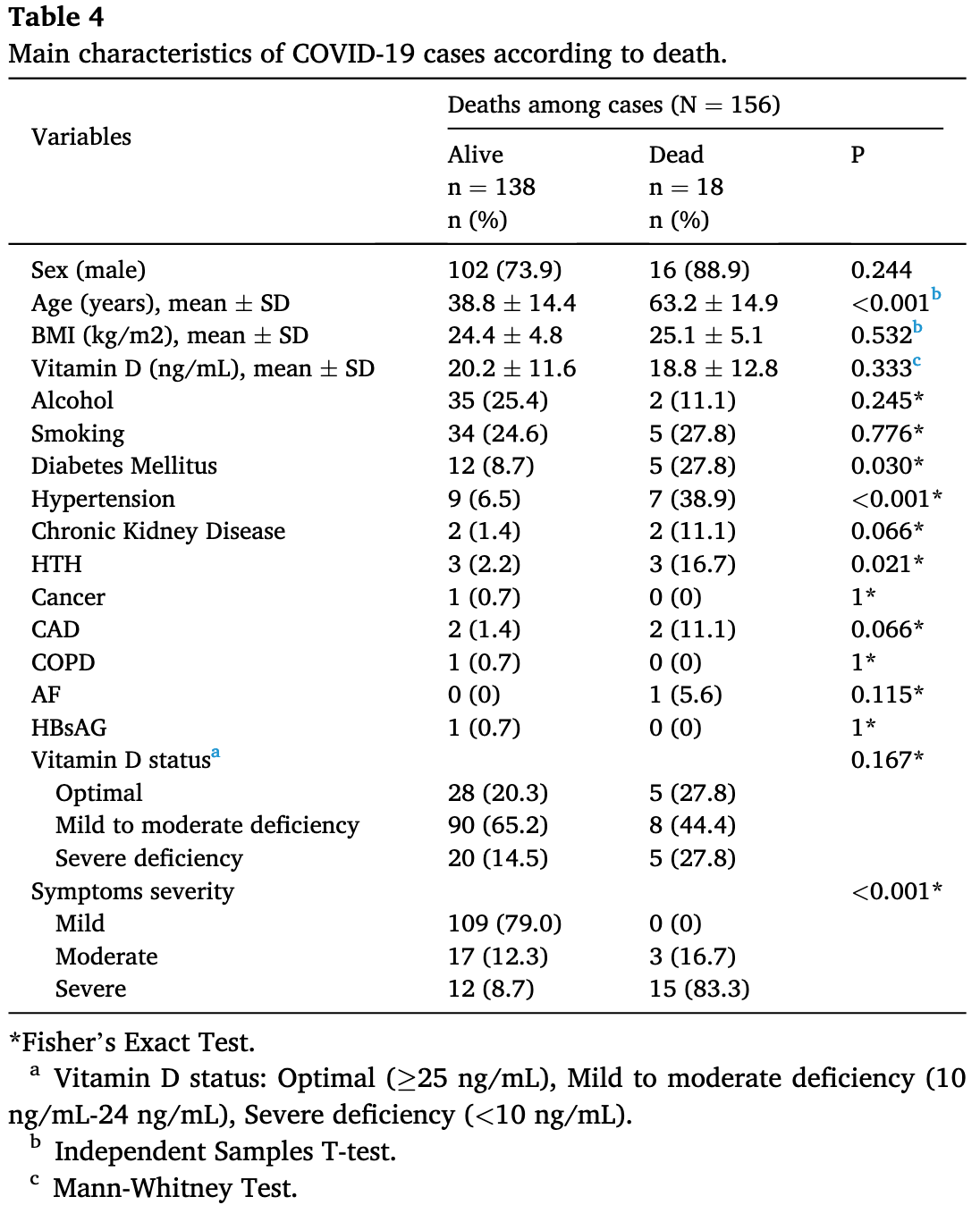 risk of death, 50.4% lower, RR 0.50, p = 0.17, high D levels 13 of 131 (9.9%), low D levels 5 of 25 (20.0%), >10ng/mL, within cases. risk of severe case, 67.6% lower, RR 0.32, p = 0.003, high D levels 17 of 131 (13.0%), low D levels 10 of 25 (40.0%), >10ng/mL, within cases. Nimavat et al., 8/5/2021, retrospective, India, South Asia, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Mohseni et al., Nutrition & Food Science, doi:10.1108/NFS-11-2020-0421 (Peer Reviewed) | cases, ↓12.4%, p=0.09 | Do body mass index (BMI) and history of nutritional supplementation play a role in the severity of COVID-19? A retrospective study |
| Details Retrospective 603 patients in Iran, 192 taking vitamin D supplements, showing no significant difference in COVID-19 cases in unadjusted results. IR.SHOUSHTAR.REC.1399.015. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Mohseni et al., Nutrition & Food Science, doi:10.1108/NFS-11-2020-0421 (Peer Reviewed) |
| Do body mass index (BMI) and history of nutritional supplementation play a role in the severity of COVID-19? A retrospective study |
Retrospective 603 patients in Iran, 192 taking vitamin D supplements, showing no significant difference in COVID-19 cases in unadjusted results. IR.SHOUSHTAR.REC.1399.015. 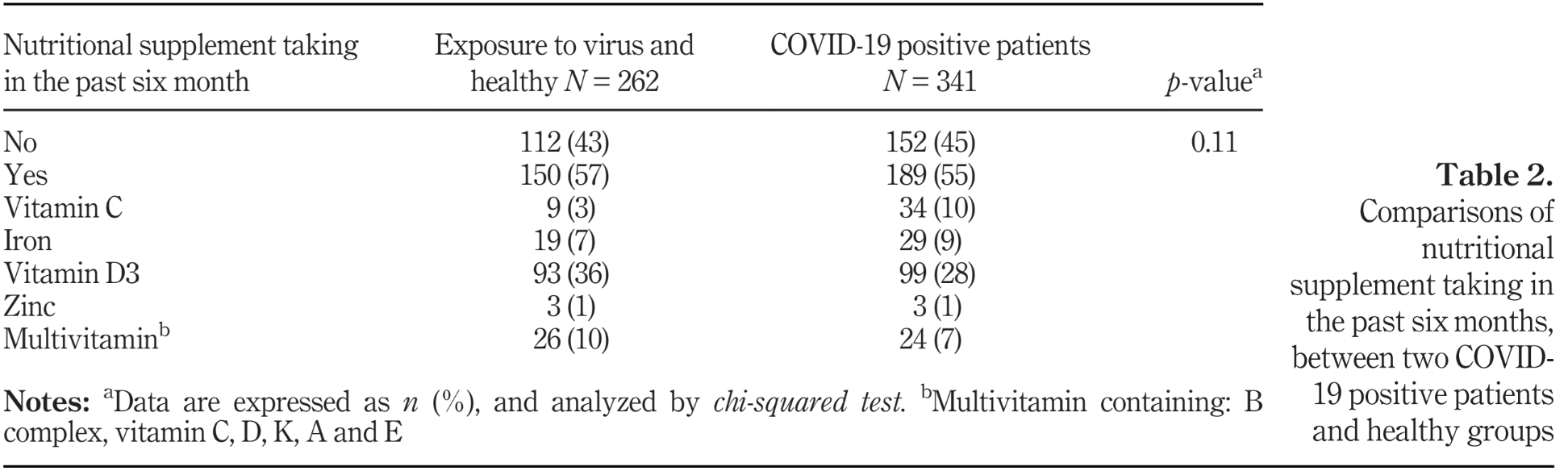 risk of case, 12.4% lower, RR 0.88, p = 0.09, treatment 99 of 192 (51.6%), control 242 of 411 (58.9%). Excluded in after exclusion results of meta analysis: unadjusted results with no group details. Mohseni et al., 8/4/2021, retrospective, Iran, Middle East, peer-reviewed, 4 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Matin et al., Archives of Microbiology, doi:10.1007/s00203-021-02482-5 (Peer Reviewed) | cases, ↓66.1%, p<0.0001 | The sufficient vitamin D and albumin level have a protective effect on COVID-19 infection |
| Details Case control study with 191 COVID-19 patients and 203 healthy controls in Iran, showing an association between vitamin D deficiency and COVID-19 infection and severity. 84.4% of COVID-19 patients had vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Matin et al., Archives of Microbiology, doi:10.1007/s00203-021-02482-5 (Peer Reviewed) |
| The sufficient vitamin D and albumin level have a protective effect on COVID-19 infection |
Case control study with 191 COVID-19 patients and 203 healthy controls in Iran, showing an association between vitamin D deficiency and COVID-19 infection and severity. 84.4% of COVID-19 patients had vitamin D deficiency. 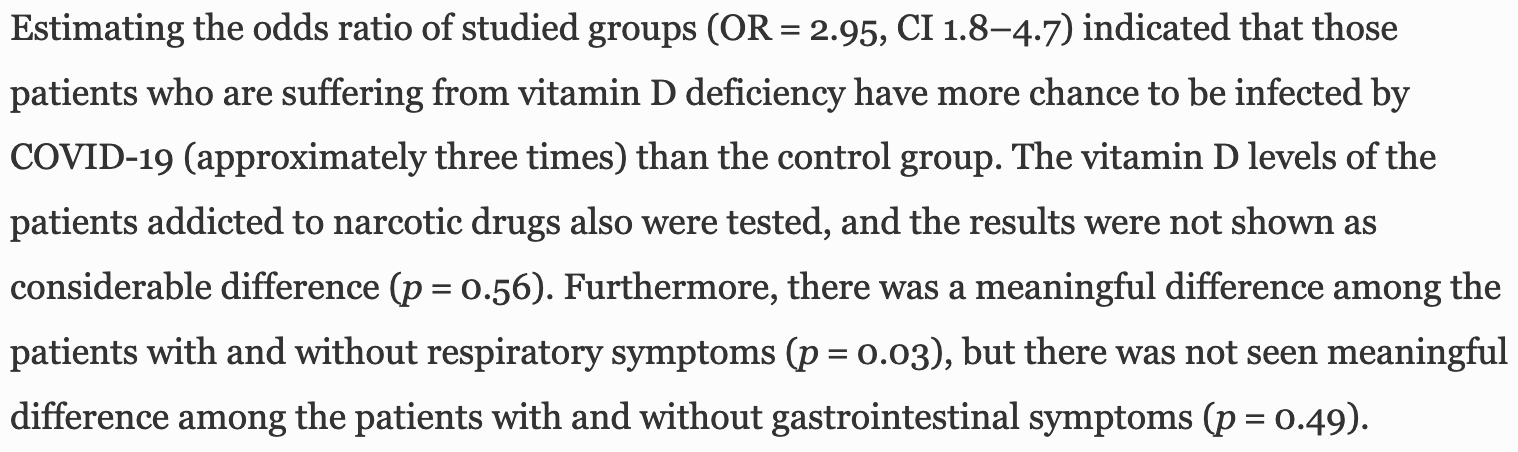 risk of case, 66.1% lower, RR 0.34, p < 0.001, case control OR, >20ng/mL. Matin et al., 7/30/2021, retrospective, case control, Iran, Middle East, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Al-Salman et al., Nutrition & Food Science, doi:10.1108/NFS-05-2021-0143 (Peer Reviewed) | ICU, ↓44.4%, p=0.03 | In COVID-19 patients, low 25-hydroxyvitamin D level in serum is associated with longer viral clearance time and higher risk of intensive care unit admission |
| Details Retrospective 450 hospitalized patients in Bahrain, showing increased risk of ICU admission and slower viral clearance with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Al-Salman et al., Nutrition & Food Science, doi:10.1108/NFS-05-2021-0143 (Peer Reviewed) |
| In COVID-19 patients, low 25-hydroxyvitamin D level in serum is associated with longer viral clearance time and higher risk of intensive care unit admission |
Retrospective 450 hospitalized patients in Bahrain, showing increased risk of ICU admission and slower viral clearance with vitamin D deficiency. risk of ICU admission, 44.4% lower, RR 0.56, p = 0.03, high D levels (≥50nmol/L) 113, low D levels (<50nmol/L) 337, multinomial regression, RR approximated with OR. Al-Salman et al., 7/29/2021, retrospective, Bahrain, Middle East, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Meta | Ghasemian et al., The International Journal of Clinical Practice, doi:10.1111/ijcp.14675 (Peer Reviewed) (meta analysis) | meta-analysis | The Role of Vitamin D in the Age of COVID-19: A Systematic Review and Meta-Analysis |
| Details Systematic review and meta analysis of 23 studies, finding significantly higher risk of COVID-19 cases and severity with vitamin D deficiency. Mortality risk was higher with deficiency, but not reaching statistical significance, OR 1.6 [0.. |
| Details Source PDF Meta Meta |
| Ghasemian et al., The International Journal of Clinical Practice, doi:10.1111/ijcp.14675 (Peer Reviewed) (meta analysis) |
| The Role of Vitamin D in the Age of COVID-19: A Systematic Review and Meta-Analysis |
Systematic review and meta analysis of 23 studies, finding significantly higher risk of COVID-19 cases and severity with vitamin D deficiency. Mortality risk was higher with deficiency, but not reaching statistical significance, OR 1.6 [0.5-4.4]. 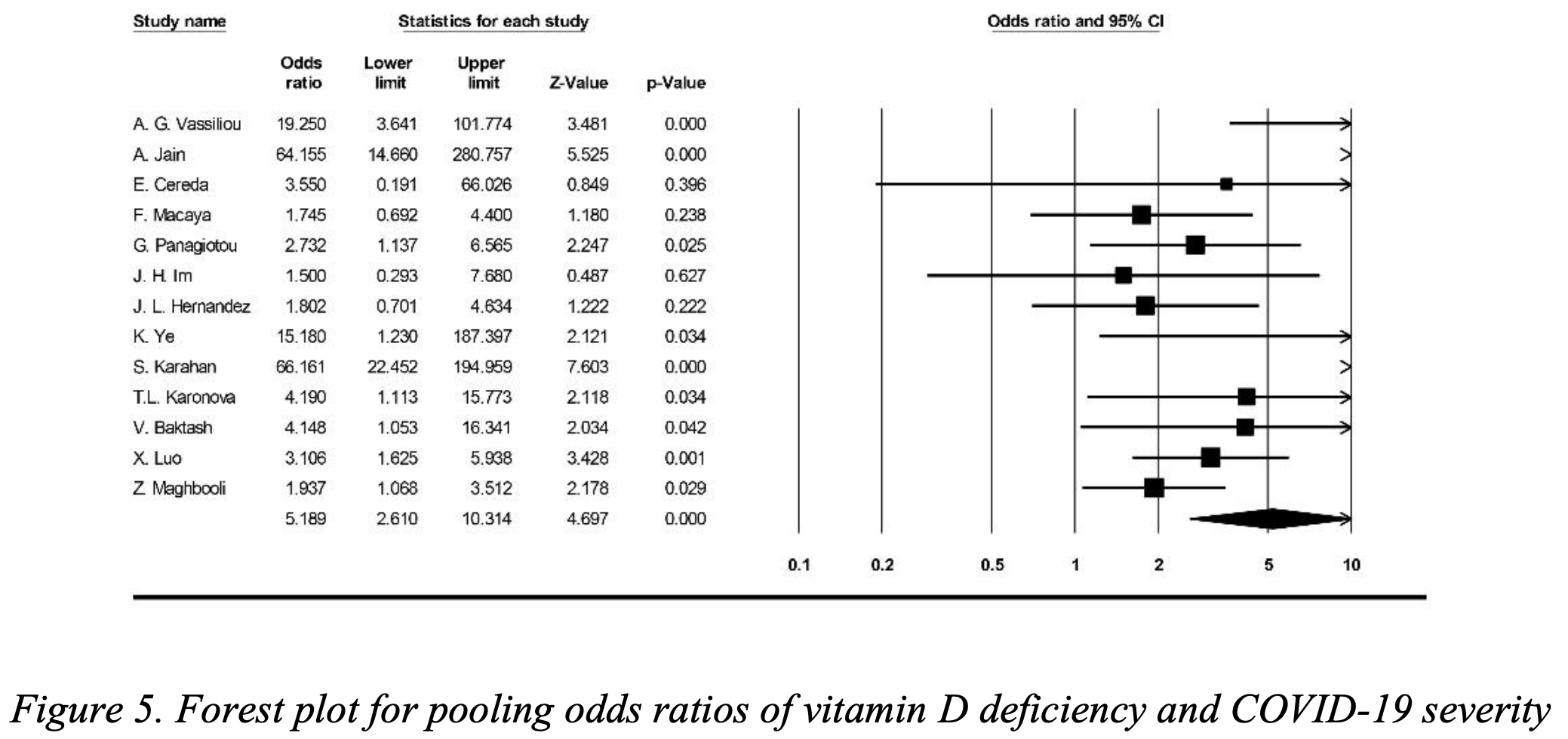 Ghasemian et al., 7/29/2021, peer-reviewed, 25 authors. |
| Submit Corrections or Comments |
| Early, PrEP | Annweiler et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:0.1016/j.jsbmb.2021.105958 (Peer Reviewed) | death, ↓64.2%, p=0.002 | Vitamin D supplementation prior to or during COVID-19 associated with better 3-month survival in geriatric patients: Extension phase of the GERIA-COVID study |
| Details Report on extended results from the GERIA-COVID study, showing significantly lower mortality at 3 months with vitamin D treatment. Results combine prophylaxis and early treatment. |
| Details Source PDF Early, PrEP Early, PrEP |
| Annweiler et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:0.1016/j.jsbmb.2021.105958 (Peer Reviewed) |
| Vitamin D supplementation prior to or during COVID-19 associated with better 3-month survival in geriatric patients: Extension phase of the GERIA-COVID study |
Report on extended results from the GERIA-COVID study, showing significantly lower mortality at 3 months with vitamin D treatment. Results combine prophylaxis and early treatment. 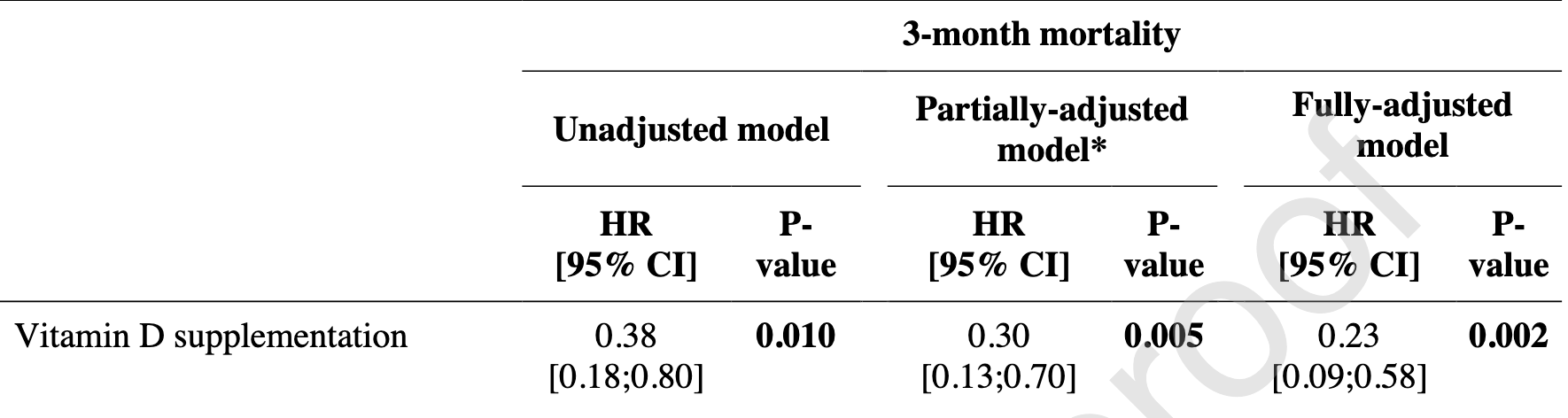 risk of death, 64.2% lower, RR 0.36, p = 0.002, treatment 16 of 67 (23.9%), control 13 of 28 (46.4%), adjusted, OR converted to RR, multiple Cox proportional hazards. Annweiler et al., 7/29/2021, prospective, France, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| In Silico | Qayyum et al., Endocrinology and Metabolism, doi:10.1152/ajpendo.00174.2021 (Peer Reviewed) | Vitamin D and lumisterol novel metabolites can inhibit SARS-CoV-2 replication machinery enzymes |
| Details In Silico analysis showing that vitamin D and lumisterol metabolites may inhibit SARS-CoV-2 Mpro and RdRP. |
| Details Source PDF In Silico In Silico |
| Qayyum et al., Endocrinology and Metabolism, doi:10.1152/ajpendo.00174.2021 (Peer Reviewed) |
| Vitamin D and lumisterol novel metabolites can inhibit SARS-CoV-2 replication machinery enzymes |
In Silico analysis showing that vitamin D and lumisterol metabolites may inhibit SARS-CoV-2 Mpro and RdRP. 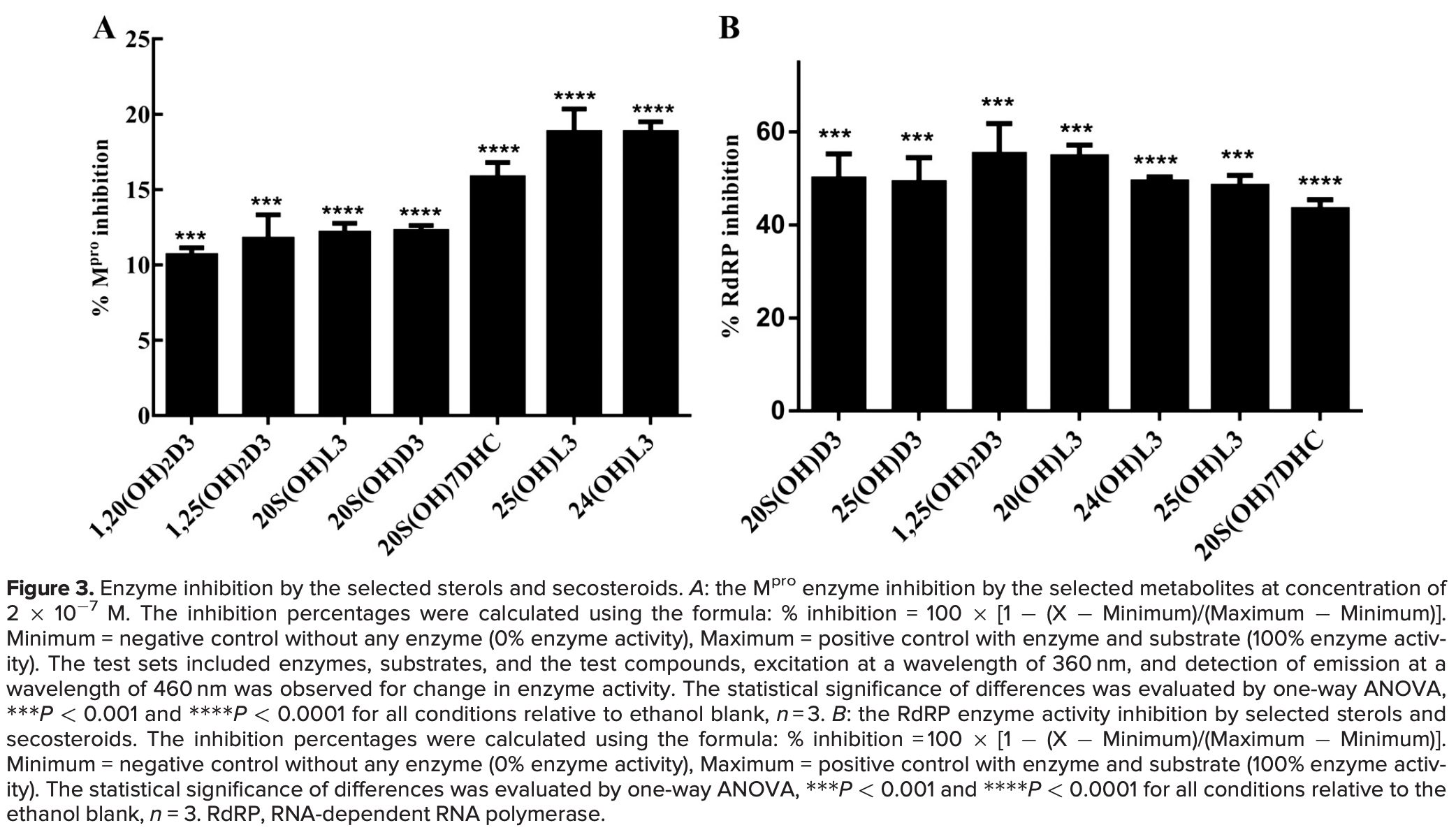 Qayyum et al., 7/27/2021, peer-reviewed, 7 authors. In Silico studies are an important part of preclinical research, however results may be very different in vivo. |
| Submit Corrections or Comments |
| Levels | Cozier et al., PLoS ONE, doi:10.1371/journal.pone.0255132 (Peer Reviewed) | cases, ↓38.6%, p=0.04 | Lower serum 25(OH)D levels associated with higher risk of COVID-19 infection in U.S. Black women |
| Details Prospective study of vitamin D levels and COVID-19 infection in the Black Women's Health Study, showing higher risk of infection for lower vitamin D levels. Vitamin D levels were from 3-7 years before infection. Levels at the time of infe.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Cozier et al., PLoS ONE, doi:10.1371/journal.pone.0255132 (Peer Reviewed) |
| Lower serum 25(OH)D levels associated with higher risk of COVID-19 infection in U.S. Black women |
Prospective study of vitamin D levels and COVID-19 infection in the Black Women's Health Study, showing higher risk of infection for lower vitamin D levels. Vitamin D levels were from 3-7 years before infection. Levels at the time of infection may differ, which may reduce the size of the effect observed. 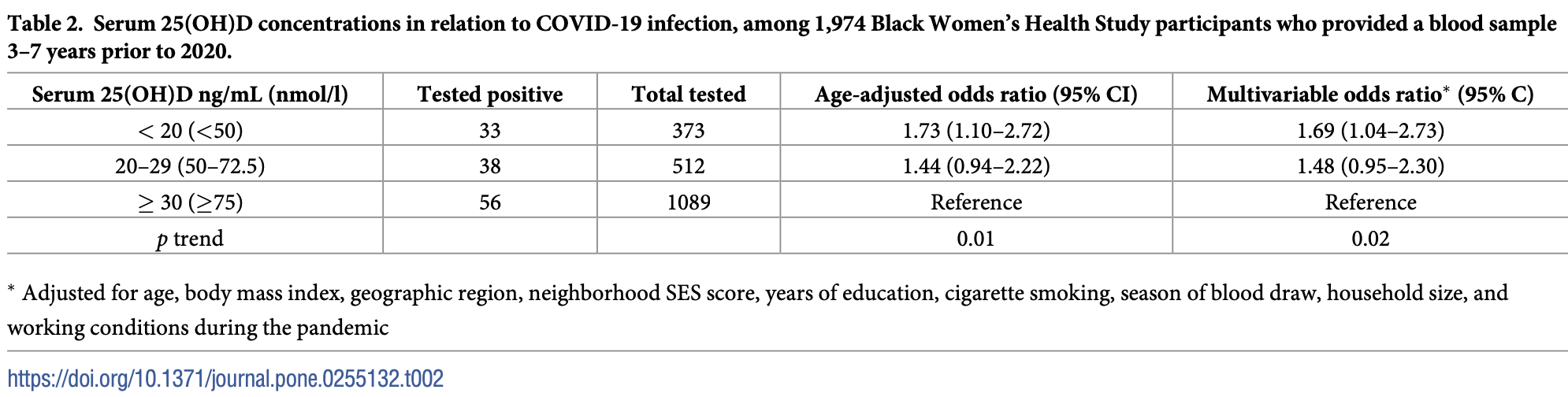 risk of case, 38.6% lower, RR 0.61, p = 0.04, high D levels 94 of 1,601 (5.9%), low D levels 33 of 373 (8.8%), adjusted, OR converted to RR, >20ng/mL, multivariable. Cozier et al., 7/27/2021, prospective, USA, North America, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Israel et al., Epidemiology and Global Health Microbiology and Infectious Disease, doi:10.7554/eLife.68165 (Peer Reviewed) | hosp., ↓9.1%, p=0.003 | Identification of drugs associated with reduced severity of COVID-19: A case-control study in a large population |
| Details Case control study examining medication usage with a healthcare database in Israel, showing lower risk of hospitalization with vitamin D (defined as being picked up within 35 days prior to PCR+). Other patients may have acquired vitamin D.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Israel et al., Epidemiology and Global Health Microbiology and Infectious Disease, doi:10.7554/eLife.68165 (Peer Reviewed) |
| Identification of drugs associated with reduced severity of COVID-19: A case-control study in a large population |
Case control study examining medication usage with a healthcare database in Israel, showing lower risk of hospitalization with vitamin D (defined as being picked up within 35 days prior to PCR+). Other patients may have acquired vitamin D supplements outside of the healthcare system. 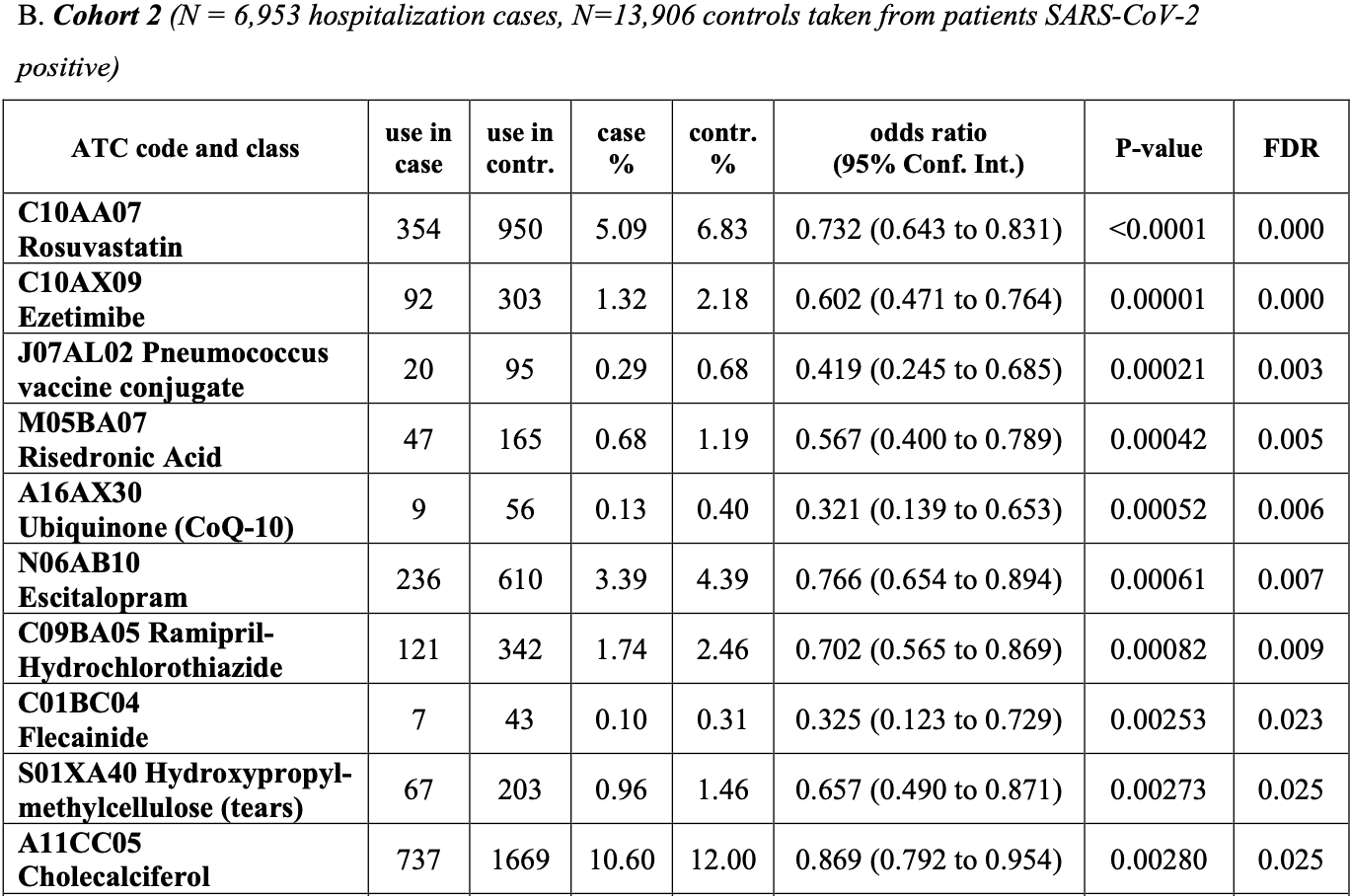 risk of hospitalization, 9.1% lower, RR 0.91, p = 0.003, treatment 737 of 2,406 (30.6%), control 6,216 of 18,453 (33.7%), OR converted to RR, PCR+, cohort 2. Israel et al., 7/27/2021, retrospective, Israel, Middle East, peer-reviewed, 10 authors, dosage not specified. |
| Submit Corrections or Comments |
| PrEPPEP | Jimenez et al., Nutrients, doi:10.3390/nu13082559 (Peer Reviewed) | death, ↓50.1%, p=0.02 | Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics |
| Details Retrospective 288 hemodialysis patients in Spain, 137 with existing vitamin D treatments (94 with paricalcitol), showing lower mortality with treatment. There was no significant difference in outcomes based on serum levels, however author.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Jimenez et al., Nutrients, doi:10.3390/nu13082559 (Peer Reviewed) |
| Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics |
Retrospective 288 hemodialysis patients in Spain, 137 with existing vitamin D treatments (94 with paricalcitol), showing lower mortality with treatment. There was no significant difference in outcomes based on serum levels, however authors do not separate patients that received vitamin D treatment. 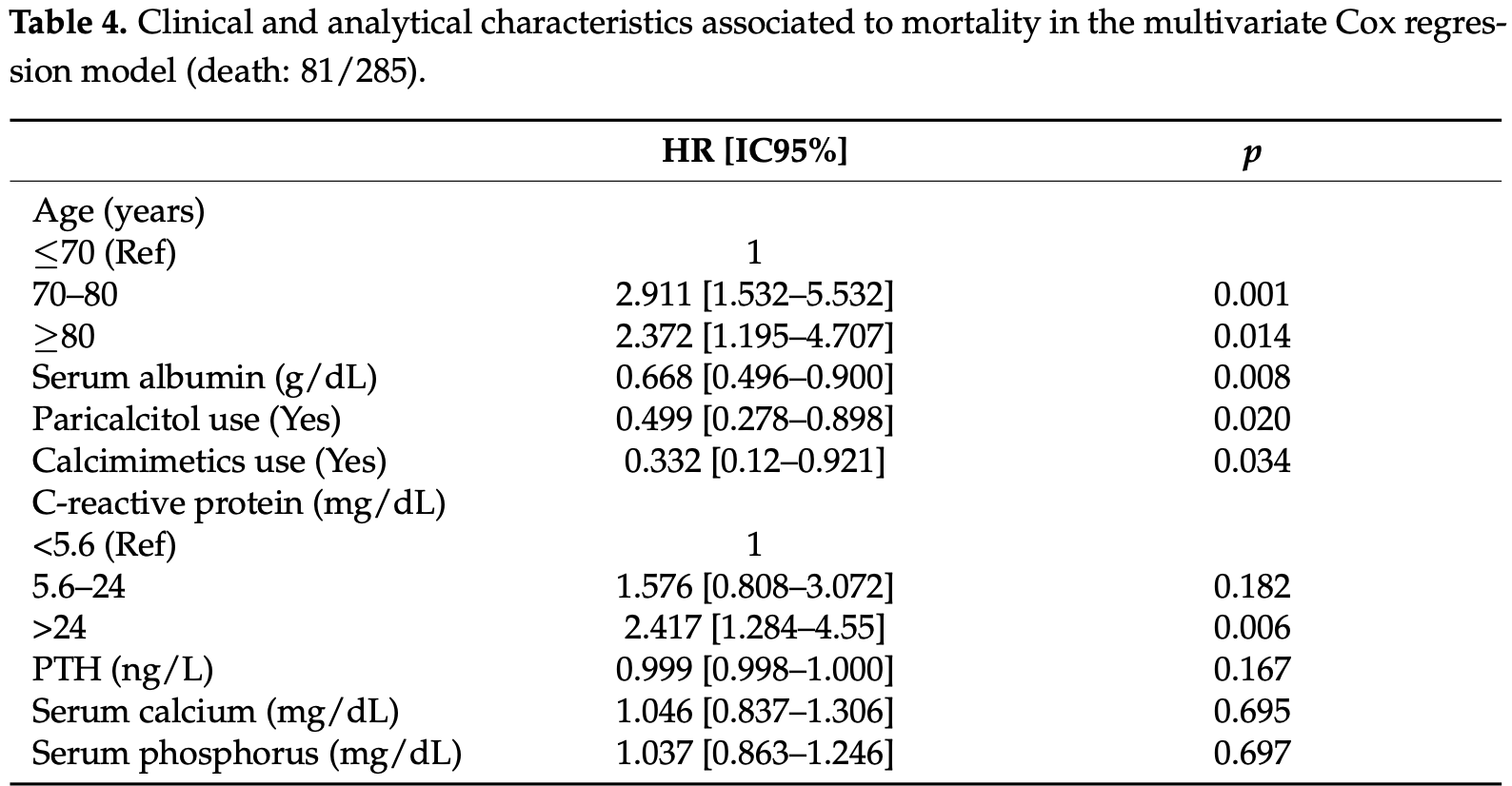 risk of death, 50.1% lower, RR 0.50, p = 0.02, treatment 16 of 94 (17.0%), control 65 of 191 (34.0%), adjusted, paricalcitol, multivariate Cox regression. risk of death, 50.7% lower, RR 0.49, p = 0.003, all vitamin D derivatives, univariate. Jimenez et al., 7/26/2021, retrospective, Spain, Europe, peer-reviewed, 21 authors, dosage paricalcitol 0.9μg weekly. |
| Submit Corrections or Comments |
| Late | Güven et al, European Journal of Clinical Nutrition, doi:10.1038/s41430-021-00984-5 (Peer Reviewed) | death, ↓24.8%, p=0.32 | The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: an observational cohort study |
| Details Retrospective 175 ICU patients, 113 treated with a single dose of 300,000IU intramuscular cholecalciferol, showing lower mortality with treatment, but not reaching statistical significance. Calcifediol or calcitriol, which avoids several .. |
| Details Source PDF Late treatment study Late treatment study |
| Güven et al, European Journal of Clinical Nutrition, doi:10.1038/s41430-021-00984-5 (Peer Reviewed) |
| The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: an observational cohort study |
Retrospective 175 ICU patients, 113 treated with a single dose of 300,000IU intramuscular cholecalciferol, showing lower mortality with treatment, but not reaching statistical significance. Calcifediol or calcitriol, which avoids several days delay in conversion, may be more successful, especially with this very late stage usage. 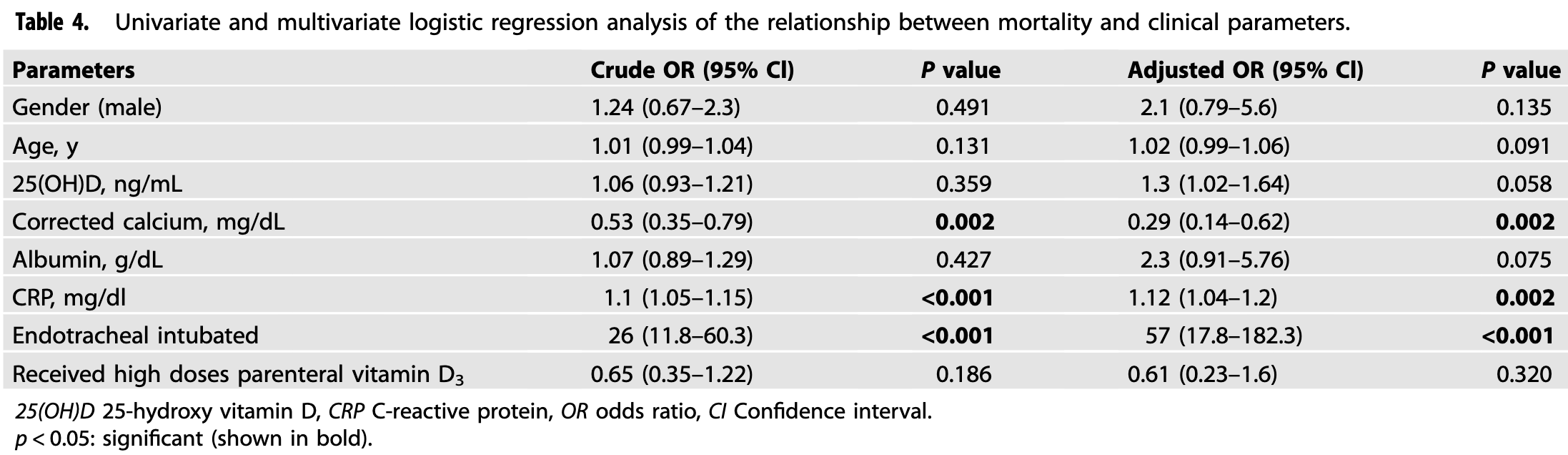 risk of death, 24.8% lower, RR 0.75, p = 0.32, treatment 43 of 113 (38.1%), control 30 of 62 (48.4%), OR converted to RR. Excluded in after exclusion results of meta analysis: very late stage, ICU patients. Güven et al., 7/23/2021, retrospective, Turkey, Europe, peer-reviewed, 2 authors, dosage 300,000IU single dose. |
| Submit Corrections or Comments |
| PrEPPEP | Oristrell et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01639-9 (Peer Reviewed) | death, ↑1.0%, p=0.91 | Vitamin D supplementation and COVID-19 risk: a population-based, cohort study |
| Details Retrospective study of cholecalciferol and calcitriol supplementation in Catalonia showing a small but significant lower risk of cases with cholecalciferol, but no significant difference for mortality, or for calcitriol supplementation. S.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Oristrell et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01639-9 (Peer Reviewed) |
| Vitamin D supplementation and COVID-19 risk: a population-based, cohort study |
Retrospective study of cholecalciferol and calcitriol supplementation in Catalonia showing a small but significant lower risk of cases with cholecalciferol, but no significant difference for mortality, or for calcitriol supplementation. Significant benefit was found for cases, severity, and mortality in patients achieving serum vitamin D levels ≥30ng/ml. 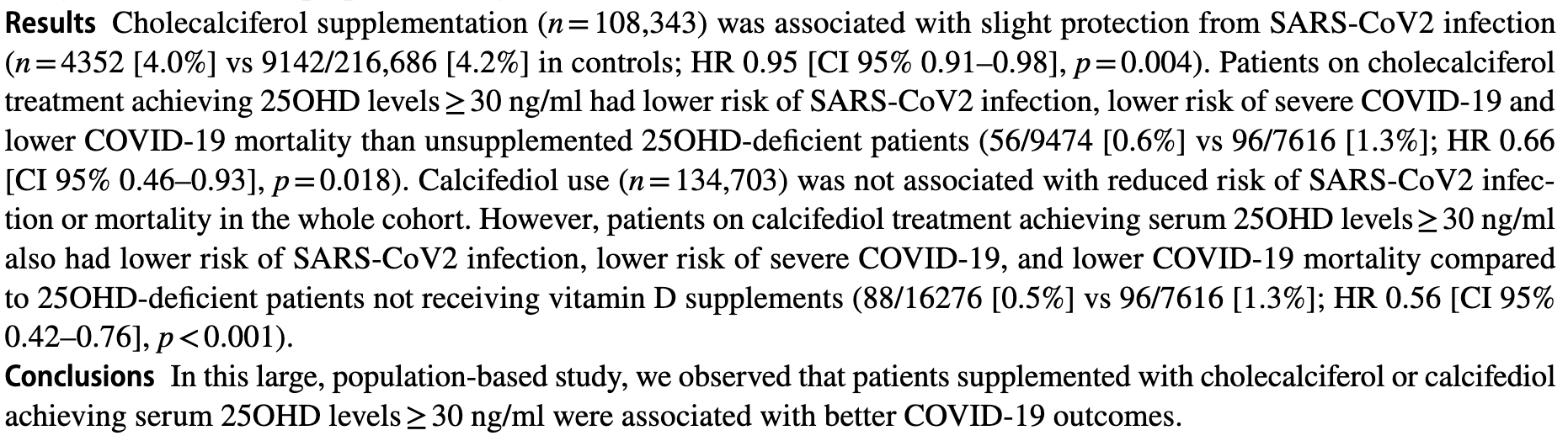 risk of death, 1.0% higher, RR 1.01, p = 0.91, calcifediol, univariate. risk of death, 4.0% lower, RR 0.96, p = 0.37, cholecalciferol, univariate. risk of case, 1.0% lower, RR 0.99, p = 0.65, calcifediol, univariate. risk of case, 5.0% lower, RR 0.95, p = 0.004, cholecalciferol, multivariate. Oristrell et al., 7/17/2021, retrospective, population-based cohort, Spain, Europe, peer-reviewed, 8 authors, dosage varies (calcifediol). |
| Submit Corrections or Comments |
| Early | Rabail et al., Food Science & Nutrition, doi:10.1002/fsn3.2458 (Peer Reviewed) | Nutritional and lifestyle changes required for minimizing the recovery period in home quarantined COVID-19 patients of Punjab, Pakistan |
| Details Survey of 80 recovered COVID-19 patients in Pakistan, showing faster recovery with vitamin C, vitamin D, and zinc supplementation. |
| Details Source PDF Early treatment study Early treatment study |
| Rabail et al., Food Science & Nutrition, doi:10.1002/fsn3.2458 (Peer Reviewed) |
| Nutritional and lifestyle changes required for minimizing the recovery period in home quarantined COVID-19 patients of Punjab, Pakistan |
Survey of 80 recovered COVID-19 patients in Pakistan, showing faster recovery with vitamin C, vitamin D, and zinc supplementation. 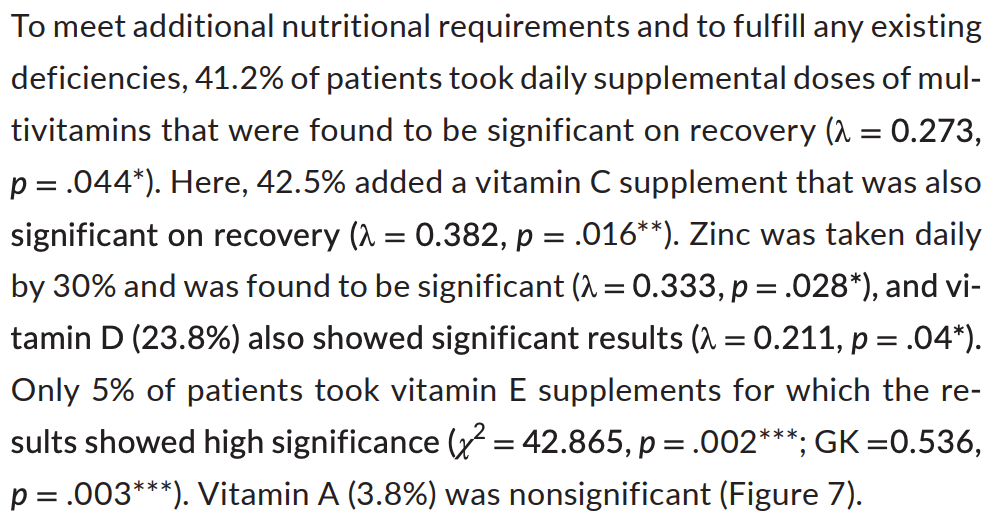 Rabail et al., 7/9/2021, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Margolin et al., Journal of Evidence-Based Integrative Medicine, doi:10.1177/2515690X211026193 (Peer Reviewed) | cases, ↓94.4%, p=0.003 | 20-Week Study of Clinical Outcomes of Over-the-Counter COVID-19 Prophylaxis and Treatment |
| Details Retrospective 113 outpatients, 53 (patient choice) treated with zinc, quercetin, vitamin C/D/E, l-lysine, and Quina, showing lower cases with treatment. Results are subject to selection bias and limited information on the groups is provid.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Margolin et al., Journal of Evidence-Based Integrative Medicine, doi:10.1177/2515690X211026193 (Peer Reviewed) |
| 20-Week Study of Clinical Outcomes of Over-the-Counter COVID-19 Prophylaxis and Treatment |
Retrospective 113 outpatients, 53 (patient choice) treated with zinc, quercetin, vitamin C/D/E, l-lysine, and Quina, showing lower cases with treatment. Results are subject to selection bias and limited information on the groups is provided. See [1]. 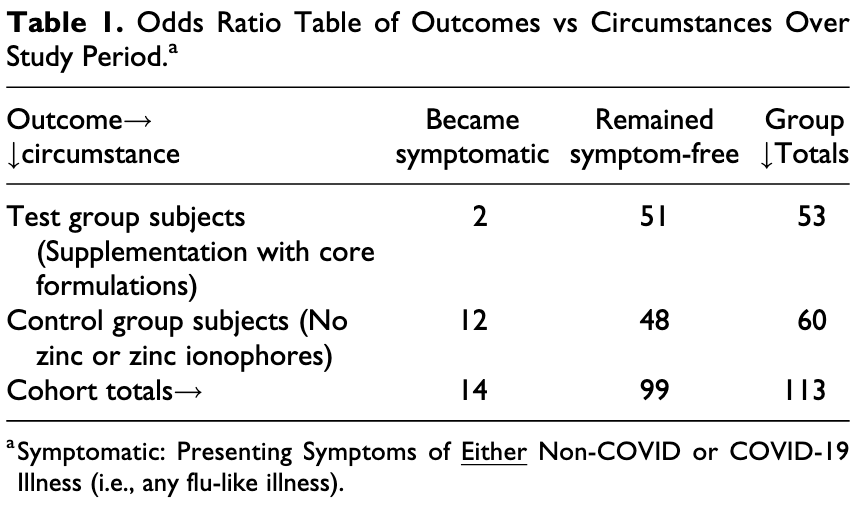 risk of case, 94.4% lower, RR 0.06, p = 0.003, treatment 0 of 53 (0.0%), control 9 of 60 (15.0%), relative risk is not 0 because of continuity correction due to zero events. risk of COVID-19 or flu-like illness, 81.1% lower, RR 0.19, p = 0.01, treatment 2 of 53 (3.8%), control 12 of 60 (20.0%). Margolin et al., 7/6/2021, retrospective, USA, North America, peer-reviewed, 5 authors, this trial uses multiple treatments in the treatment arm (combined with zinc, quercetin, vitamin C/E, l-lysine, and Quina) - results of individual treatments may vary. |
| Submit Corrections or Comments |
| Levels | Bianconi et al., Nutrition, doi:10.1016/j.nut.2021.111408 (Peer Reviewed) | death, ↓17.5%, p=0.58 | Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19 |
| Details Prospective study of 200 hospitalized patients in Italy, showing 80% of patients had vitamin D deficiency. There was no significant differences in outcomes based on vitamin D levels. There was also no significant difference in vitamin D l.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Bianconi et al., Nutrition, doi:10.1016/j.nut.2021.111408 (Peer Reviewed) |
| Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19 |
Prospective study of 200 hospitalized patients in Italy, showing 80% of patients had vitamin D deficiency. There was no significant differences in outcomes based on vitamin D levels. There was also no significant difference in vitamin D levels when compared with sepsis patients. 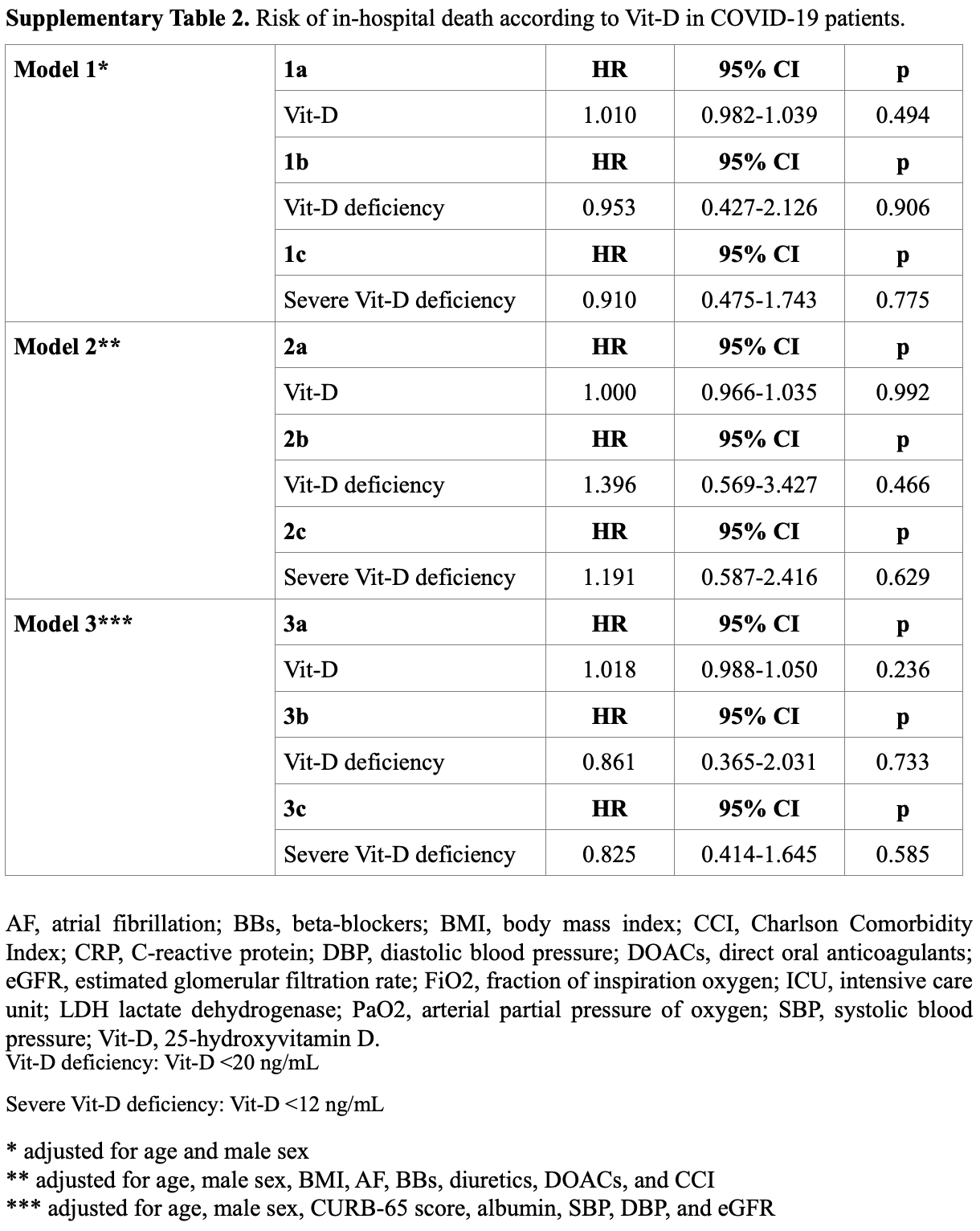 risk of death, 17.5% lower, RR 0.82, p = 0.58, high D levels (≥12ng/ml) 94, low D levels (<12ng/ml) 106, model 3, Table S2, Cox proportional hazards. risk of death, 13.9% lower, RR 0.86, p = 0.73, high D levels (≥20ng/ml) 40, low D levels (<20ng/ml) 160, model 3, Table S2, Cox proportional hazards. risk of death/ICU, 15.9% lower, RR 0.84, p = 0.53, high D levels (≥12ng/ml) 94, low D levels (<12ng/ml) 106, model 3, Cox proportional hazards. risk of death/ICU, 10.9% lower, RR 0.89, p = 0.73, high D levels (≥20ng/ml) 40, low D levels (<20ng/ml) 160, model 3, Cox proportional hazards. Bianconi et al., 7/1/2021, prospective, Italy, Europe, peer-reviewed, 12 authors. |
| Submit Corrections or Comments |
| Late | Sabico et al., Nutrients, doi:10.3390/nu13072170 (Peer Reviewed) | Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial |
| Details Small RCT of 69 hospitalized patients comparing 1000IU and 5000IU daily cholecalciferol, showing faster recovery with the higher dose. |
| Details Source PDF Late treatment study Late treatment study |
| Sabico et al., Nutrients, doi:10.3390/nu13072170 (Peer Reviewed) |
| Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial |
Small RCT of 69 hospitalized patients comparing 1000IU and 5000IU daily cholecalciferol, showing faster recovery with the higher dose. 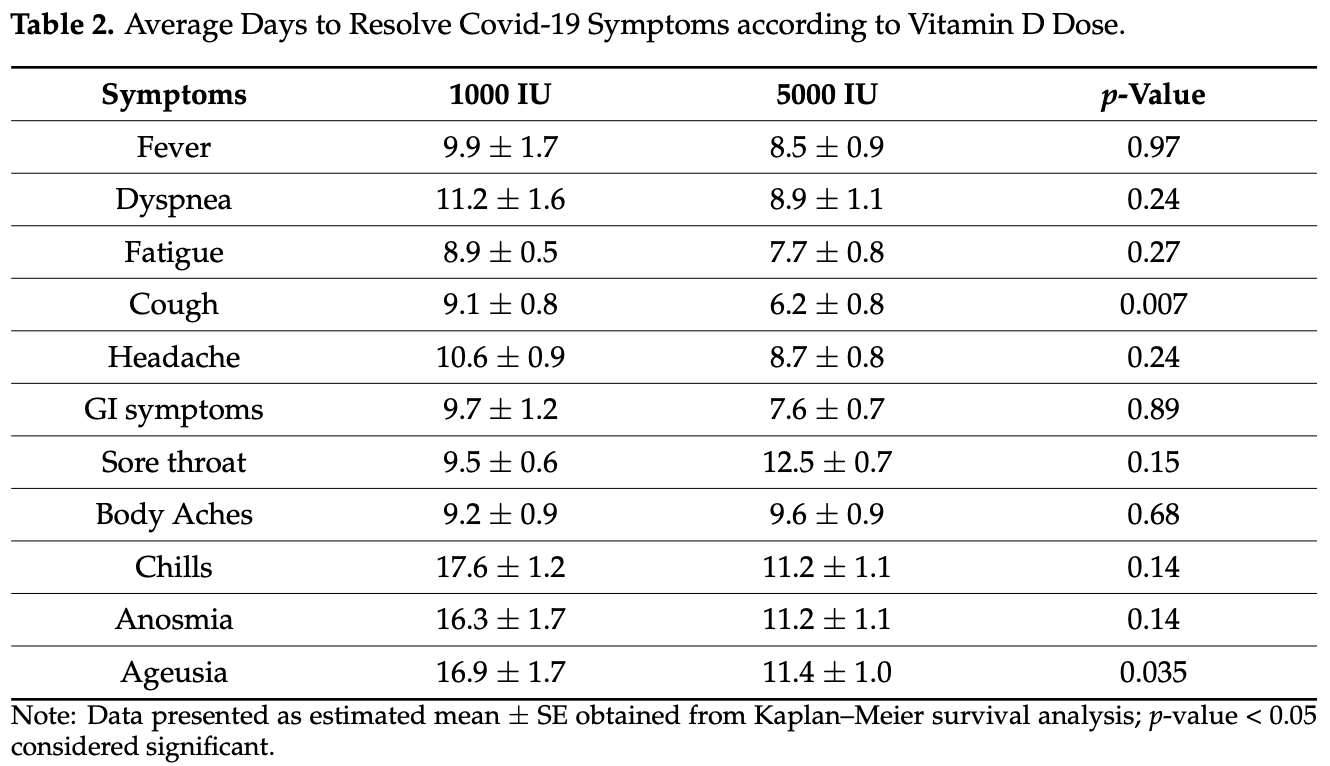 Sabico et al., 6/24/2021, Randomized Controlled Trial, Saudi Arabia, Middle East, peer-reviewed, 12 authors. |
| Submit Corrections or Comments |
| Meta | Pal et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01614-4 (Peer Reviewed) (meta analysis) | meta-analysis | Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis |
| Details Meta analysis of 13 vitamin D treatment studies, showing significantly lower ICU admission/mortality with treatment. |
| Details Source PDF Meta Meta |
| Pal et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01614-4 (Peer Reviewed) (meta analysis) |
| Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis |
Meta analysis of 13 vitamin D treatment studies, showing significantly lower ICU admission/mortality with treatment. 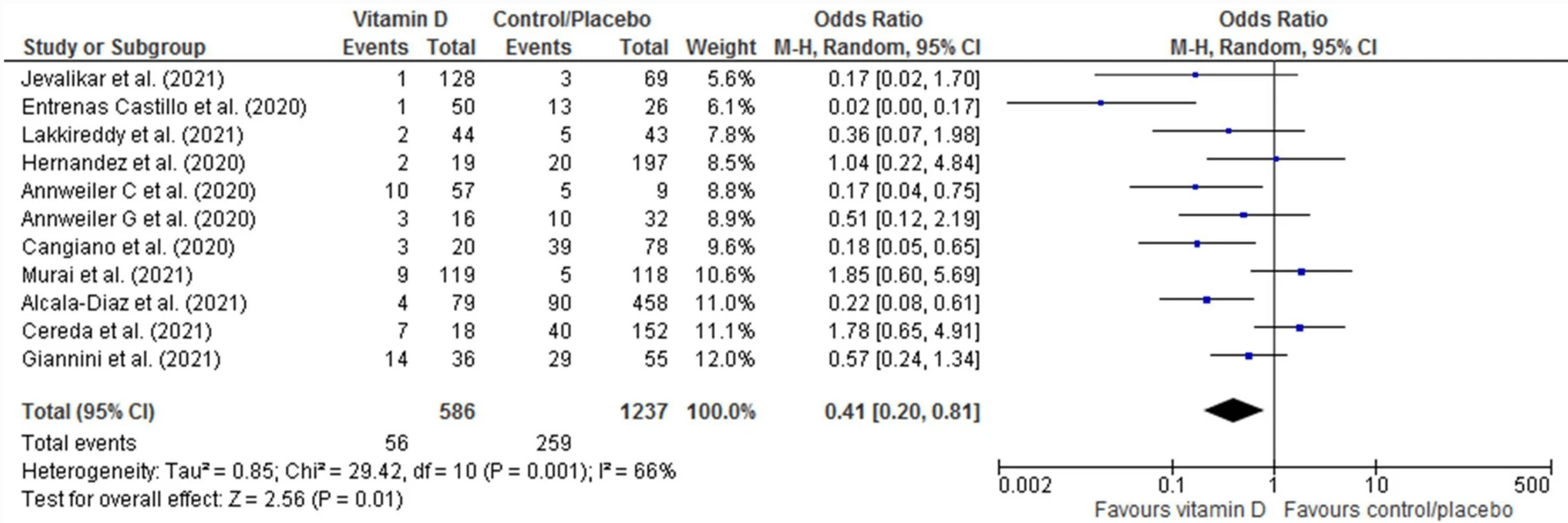 Pal et al., 6/24/2021, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Beigmohammadi et al., Nutrition, doi:10.1016/j.nut.2021.111400 (Peer Reviewed) | The association between serum levels of micronutrients and the severity of disease in patients with COVID-19 |
| Details Retrospective 60 ICU patients in Iran, showing that lower levels of vitamin D, magnesium, and zinc were significantly associated with higher APACHE scores (P = 0.001, 0.028, and <0.001, respectively) and higher lung involvement (P = 0.002.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Beigmohammadi et al., Nutrition, doi:10.1016/j.nut.2021.111400 (Peer Reviewed) |
| The association between serum levels of micronutrients and the severity of disease in patients with COVID-19 |
Retrospective 60 ICU patients in Iran, showing that lower levels of vitamin D, magnesium, and zinc were significantly associated with higher APACHE scores (P = 0.001, 0.028, and <0.001, respectively) and higher lung involvement (P = 0.002, 0.045, and <0.001, respectively). 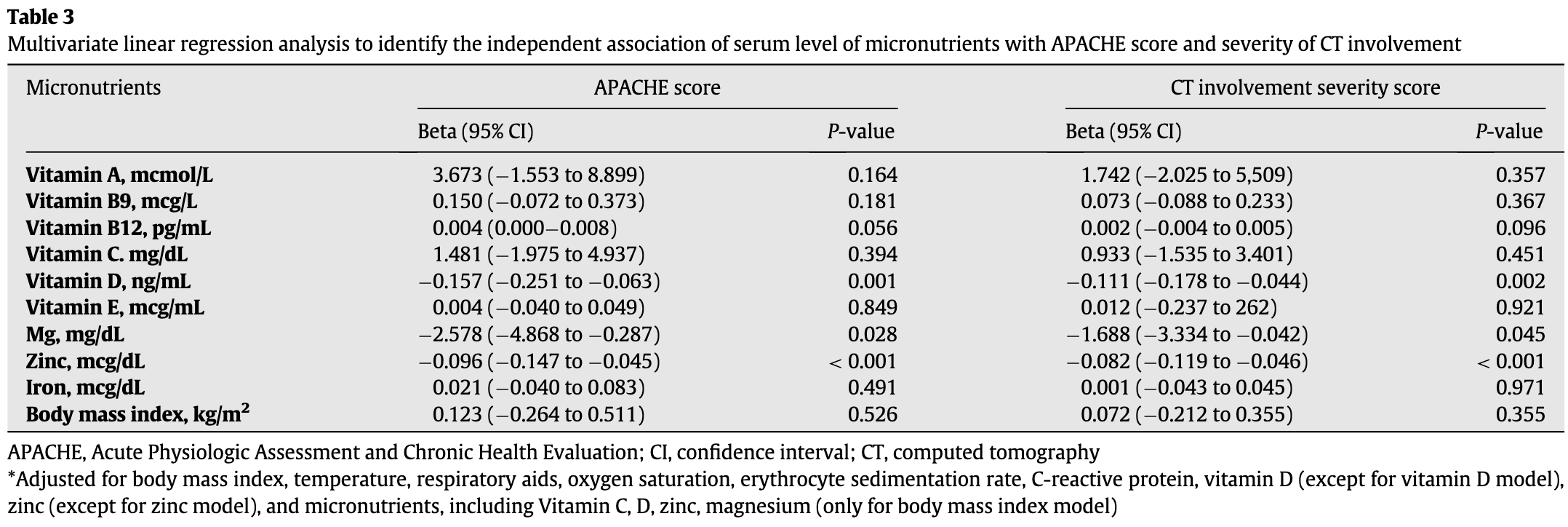 Beigmohammadi et al., 6/24/2021, retrospective, Iran, Middle East, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Zelzer et al., Nutrients, doi:10.3390/nu13072129 (Peer Reviewed) | death, ↓46.4%, p=0.08 | Vitamin D Metabolites and Clinical Outcome in Hospitalized COVID-19 Patients |
| Details Retrospective 148 patients in Austria, showing no statistically significant differences in vitamin D levels and metabolites for mortality or respiratory support. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Zelzer et al., Nutrients, doi:10.3390/nu13072129 (Peer Reviewed) |
| Vitamin D Metabolites and Clinical Outcome in Hospitalized COVID-19 Patients |
Retrospective 148 patients in Austria, showing no statistically significant differences in vitamin D levels and metabolites for mortality or respiratory support. 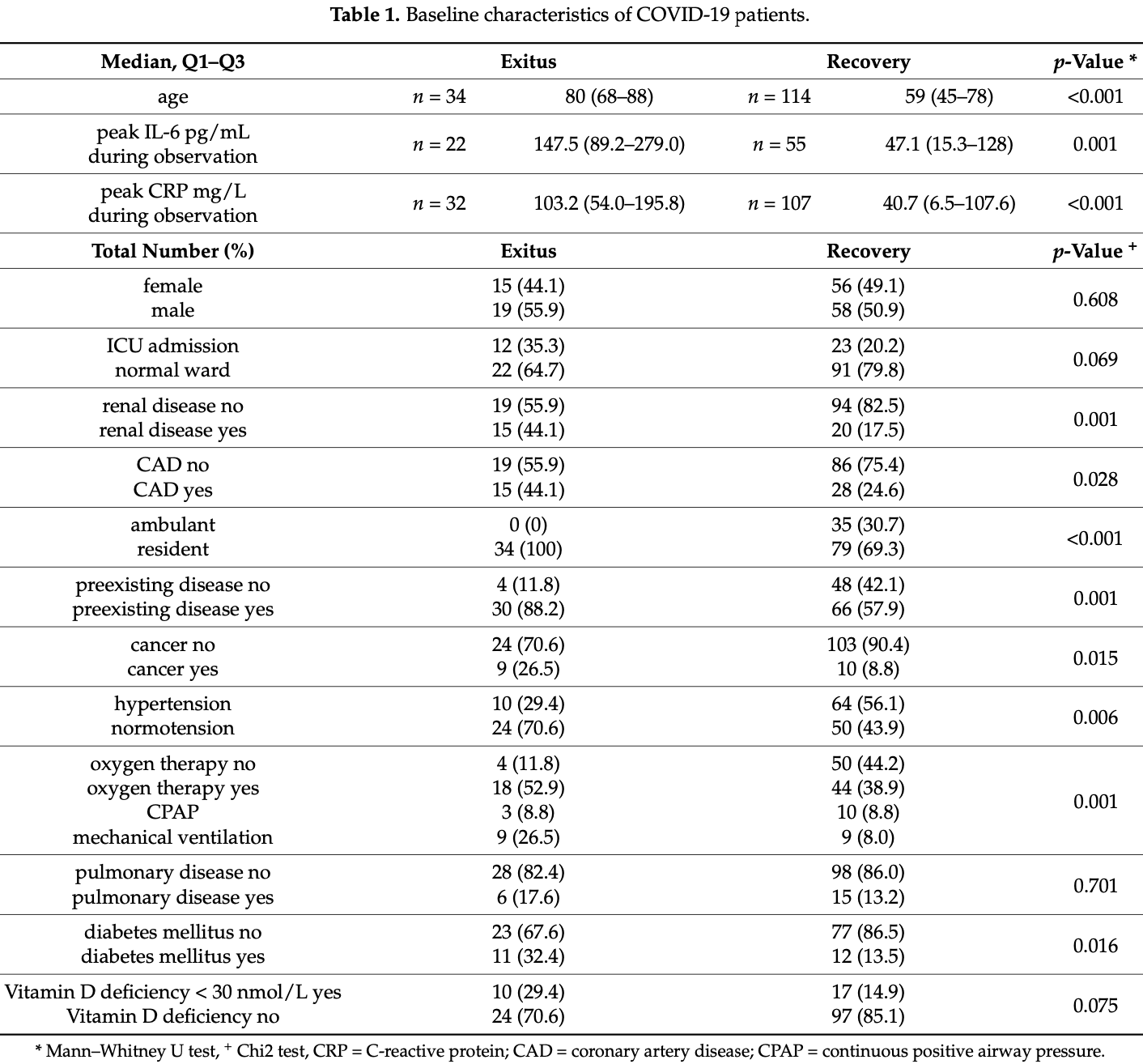 risk of death, 46.4% lower, RR 0.54, p = 0.08, high D levels 24 of 121 (19.8%), low D levels 10 of 27 (37.0%), >30nmol/L. Zelzer et al., 6/22/2021, retrospective, Austria, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Levels | Jude et al., Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab439 (Peer Reviewed) | hosp., ↓71.6%, p<0.0001 | Vitamin D deficiency is associated with higher hospitalisation risk from COVID-19: a retrospective case-control study |
| Details Retrospective 80,670 people in the UK with vitamin D levels measured within the last 12 months, showing higher risk of hospitalization with low vitamin D levels. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Jude et al., Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab439 (Peer Reviewed) |
| Vitamin D deficiency is associated with higher hospitalisation risk from COVID-19: a retrospective case-control study |
Retrospective 80,670 people in the UK with vitamin D levels measured within the last 12 months, showing higher risk of hospitalization with low vitamin D levels. 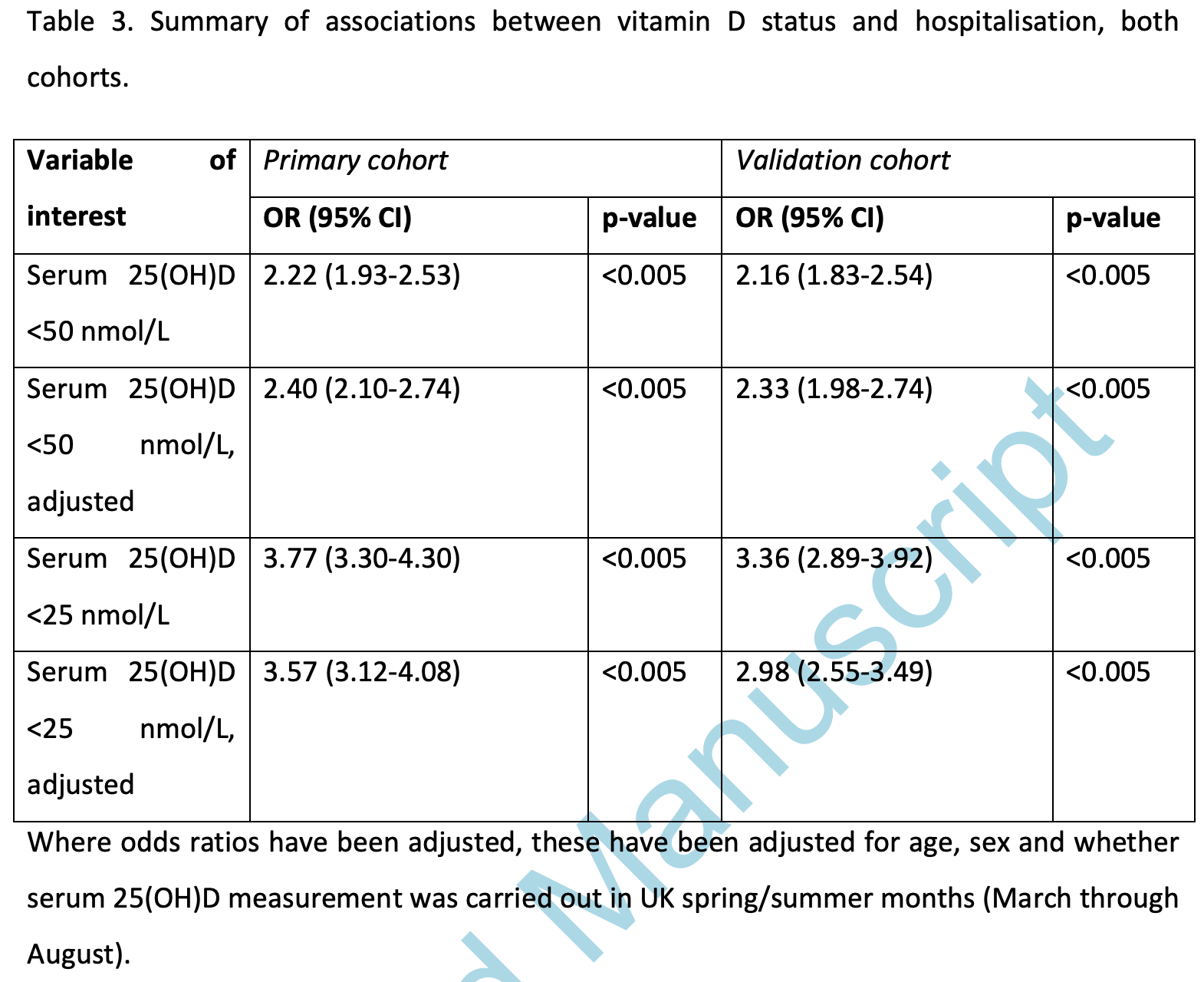 risk of hospitalization, 71.6% lower, RR 0.28, p < 0.001, adjusted, OR converted to RR, >25 nmol/L, control prevalence approximated with overall prevalence. risk of hospitalization, 57.9% lower, RR 0.42, p < 0.001, adjusted, OR converted to RR, >50 nmol/L, control prevalence approximated with overall prevalence. Jude et al., 6/17/2021, retrospective, United Kingdom, Europe, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Campi et al., BMC Infectious Diseases, doi:10.1186/s12879-021-06281-7 (Peer Reviewed) | severe case, ↓88.4%, p<0.0001 | Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy |
| Details |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Campi et al., BMC Infectious Diseases, doi:10.1186/s12879-021-06281-7 (Peer Reviewed) |
| Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy |
 risk of severe case, 88.4% lower, RR 0.12, p < 0.001, treatment 31 of 103 (30.1%) cases, 41 of 52 (78.8%) controls, case control OR. Excluded in after exclusion results of meta analysis: significant unadjusted differences between groups. Campi et al., 6/14/2021, prospective, Italy, Europe, peer-reviewed, 21 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Campi et al., BMC Infectious Diseases, doi:10.1186/s12879-021-06281-7 (Peer Reviewed) | death, ↓24.3%, p=0.53 | Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy |
| Details Prospective study of 103 hospitalized patients in Italy, showing very high prevalence of vitamin D deficiency, and increased severity for lower vitamin D levels. Vitamin D supplementation was significantly less common for cases. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Campi et al., BMC Infectious Diseases, doi:10.1186/s12879-021-06281-7 (Peer Reviewed) |
| Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy |
Prospective study of 103 hospitalized patients in Italy, showing very high prevalence of vitamin D deficiency, and increased severity for lower vitamin D levels. Vitamin D supplementation was significantly less common for cases. 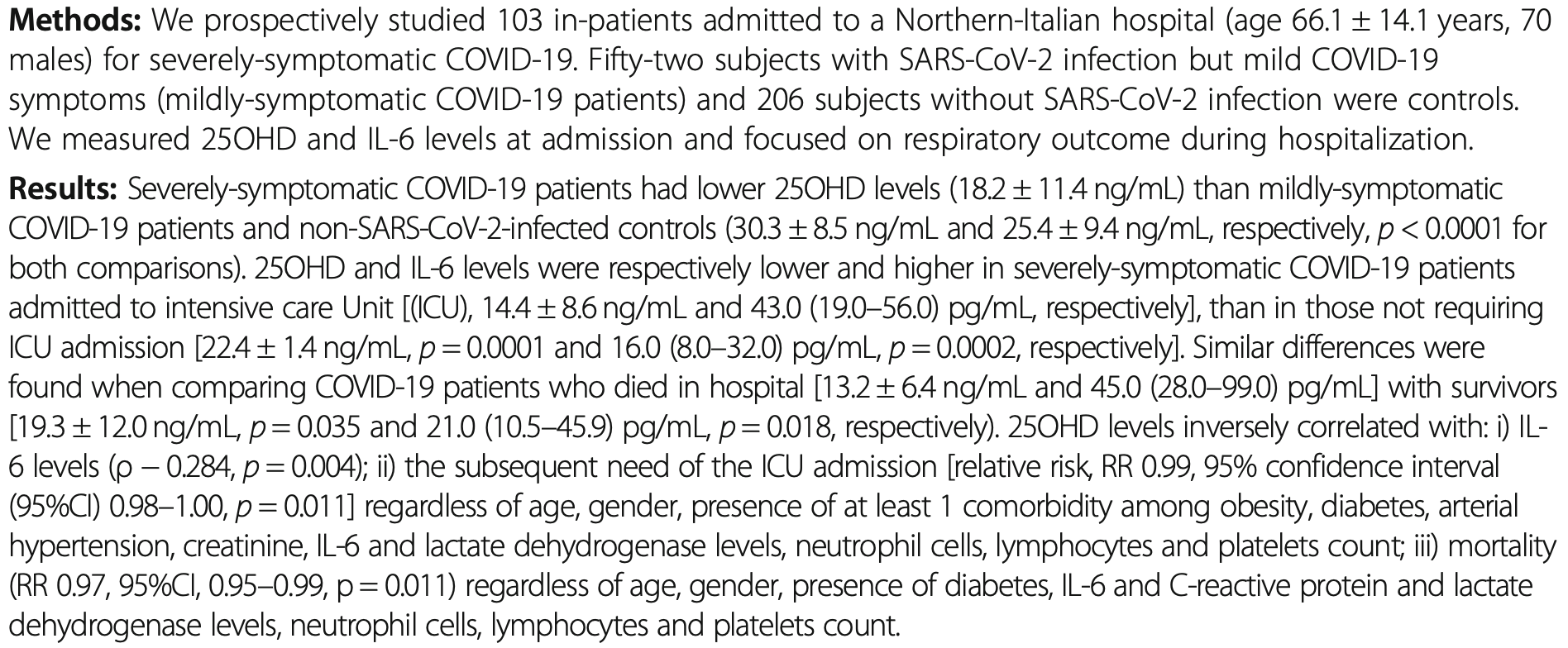 risk of death for severe patients, 24.3% lower, RR 0.76, p = 0.53, high D levels (≥20ng/ml) 6 of 39 (15.4%), low D levels (<20ng/ml) 13 of 64 (20.3%), hospitalized patients. risk of ICU for severe patients, 53.1% lower, RR 0.47, p < 0.001, high D levels (≥20ng/ml) 12 of 39 (30.8%), low D levels (<20ng/ml) 42 of 64 (65.6%), hospitalized patients. Campi et al., 6/14/2021, prospective, Italy, Europe, peer-reviewed, 21 authors. |
| Submit Corrections or Comments |
| Levels | Dror et al., medRxiv, doi:10.1101/2021.06.04.21258358 (Preprint) | severe case, ↓85.1%, p=0.001 | Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness |
| Details Retrospective 253 hospitalized patients in Israel showing higher mortality and higher risk of severe cases with vitamin D deficiency. Vitamin D levels were measured 14 to 730 days before the COVID-19 test. Adjusted results are only provid.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Dror et al., medRxiv, doi:10.1101/2021.06.04.21258358 (Preprint) |
| Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness |
Retrospective 253 hospitalized patients in Israel showing higher mortality and higher risk of severe cases with vitamin D deficiency. Vitamin D levels were measured 14 to 730 days before the COVID-19 test. Adjusted results are only provided for severity. 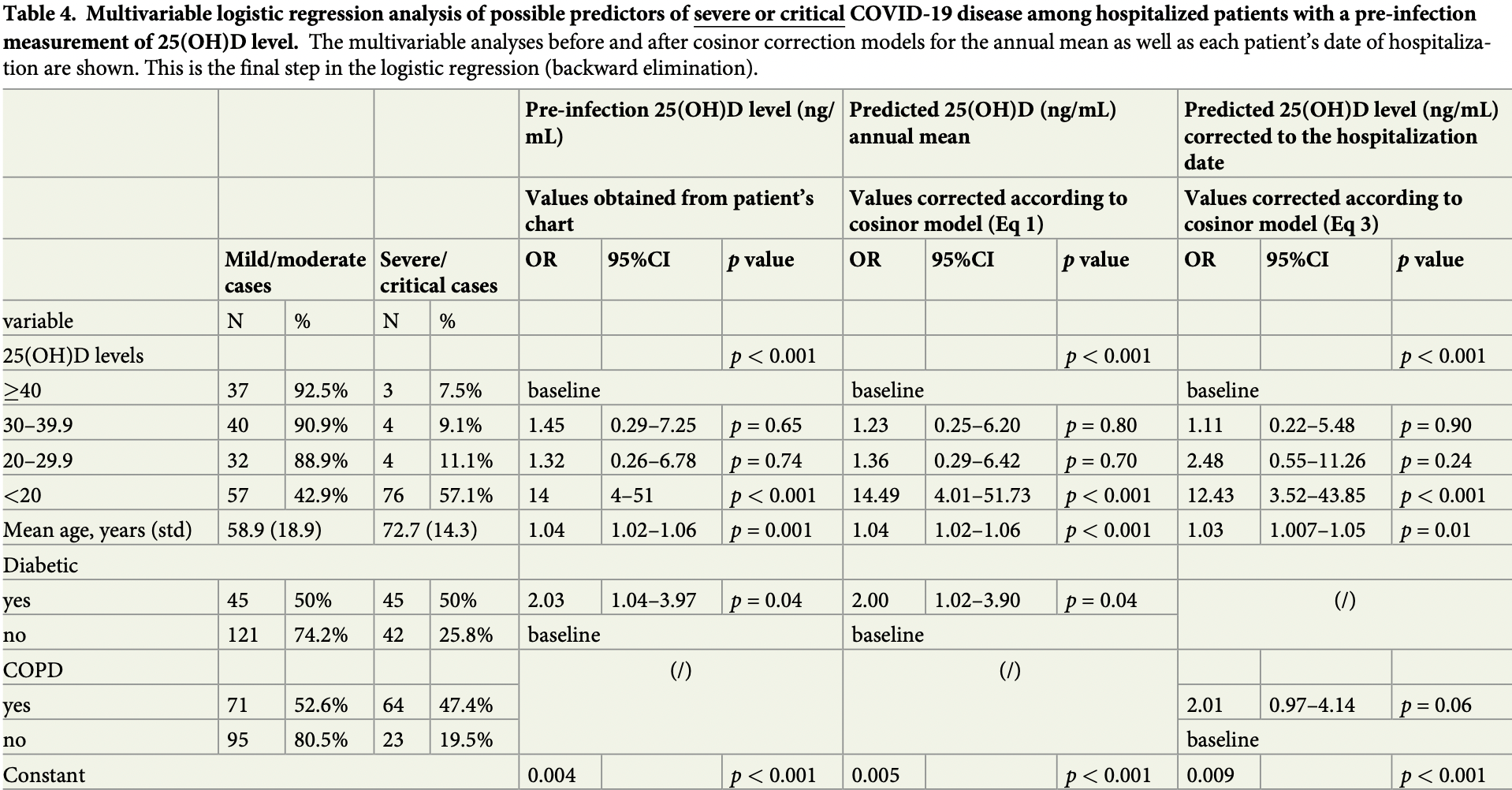 risk of severe or critical case, 85.1% lower, RR 0.15, p = 0.001, high D levels 109 of 120 (90.8%), low D levels 76 of 133 (57.1%), OR converted to RR, >40ng/mL vs. <20ng/mL, multivariate logistic regression. Dror et al., 6/7/2021, retrospective, Israel, Middle East, preprint, 18 authors. |
| Submit Corrections or Comments |
| Levels | Diaz-Curiel, Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105928 (Peer Reviewed) | ICU, ↓73.2%, p=0.02 | The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish patients |
| Details Retrospective 1,549 patients in Spain showing that the frequency of vitamin D deficiency was higher in admitted patients compared to the overall Spanish population, and that vitamin D deficiency was associated with increased risk of ICU a.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Diaz-Curiel, Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105928 (Peer Reviewed) |
| The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish patients |
Retrospective 1,549 patients in Spain showing that the frequency of vitamin D deficiency was higher in admitted patients compared to the overall Spanish population, and that vitamin D deficiency was associated with increased risk of ICU admission amongst admitted patients. Adjusted vitamin D levels were lower in deceased patients, but statistical significance was not reached (authors provide only average levels, they do not provide mortality analysis based on deficiency). 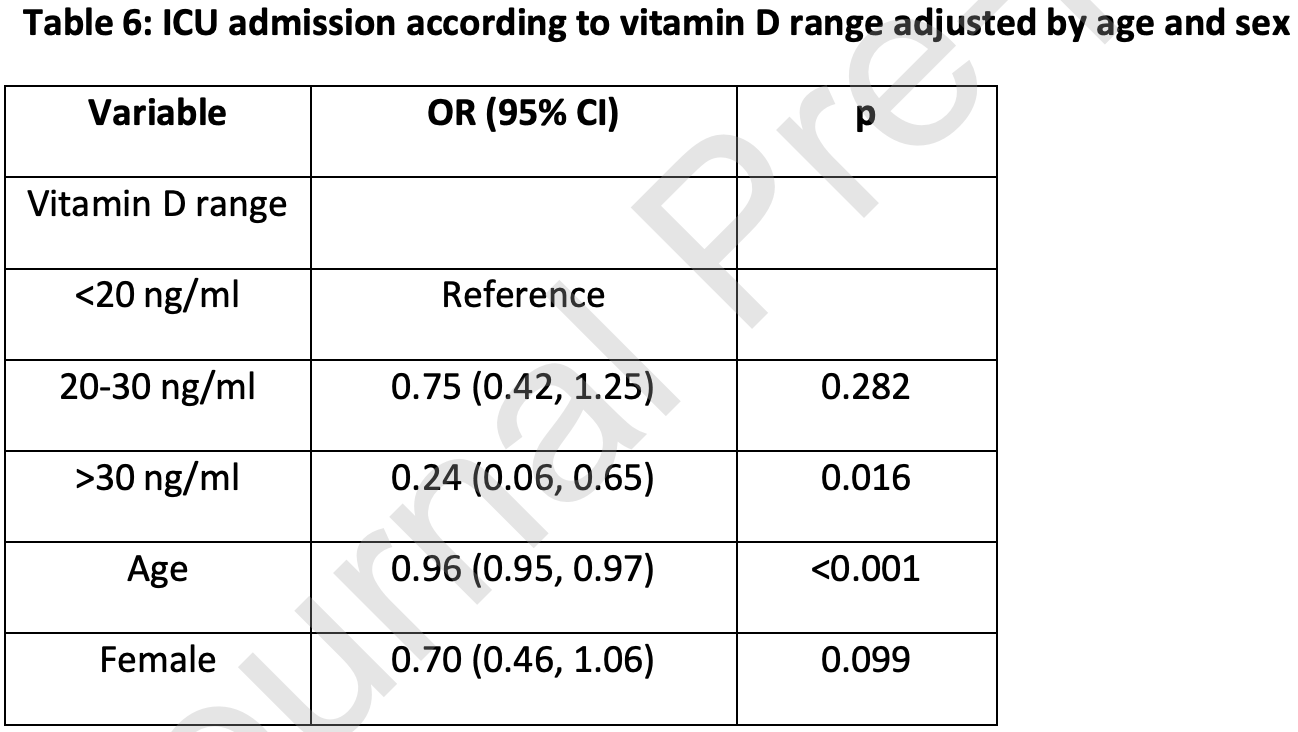 risk of ICU admission, 73.2% lower, RR 0.27, p = 0.02, high D levels 3 of 214 (1.4%), low D levels 91 of 1,017 (8.9%), OR converted to RR, >30ng/mL vs. <20ng/mL. Diaz-Curiel et al., 6/6/2021, retrospective, Spain, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Kotur et al., Frontiers in Nutrition, doi:10.3389/fnut.2021.689419 (Peer Reviewed) | Association of Vitamin D, Zinc and Selenium Related Genetic Variants With COVID-19 Disease Severity |
| Details Analysis of variants in genes significant for the status of vitamin D in 120 Serbian COVID-19 patients, showing that vitamin D related genetic variants DHCR7/NADSYN rs12785878 and CYP2R1 rs10741657 were associated with severe COVID-19 in .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Kotur et al., Frontiers in Nutrition, doi:10.3389/fnut.2021.689419 (Peer Reviewed) |
| Association of Vitamin D, Zinc and Selenium Related Genetic Variants With COVID-19 Disease Severity |
Analysis of variants in genes significant for the status of vitamin D in 120 Serbian COVID-19 patients, showing that vitamin D related genetic variants DHCR7/NADSYN rs12785878 and CYP2R1 rs10741657 were associated with severe COVID-19 in adults. 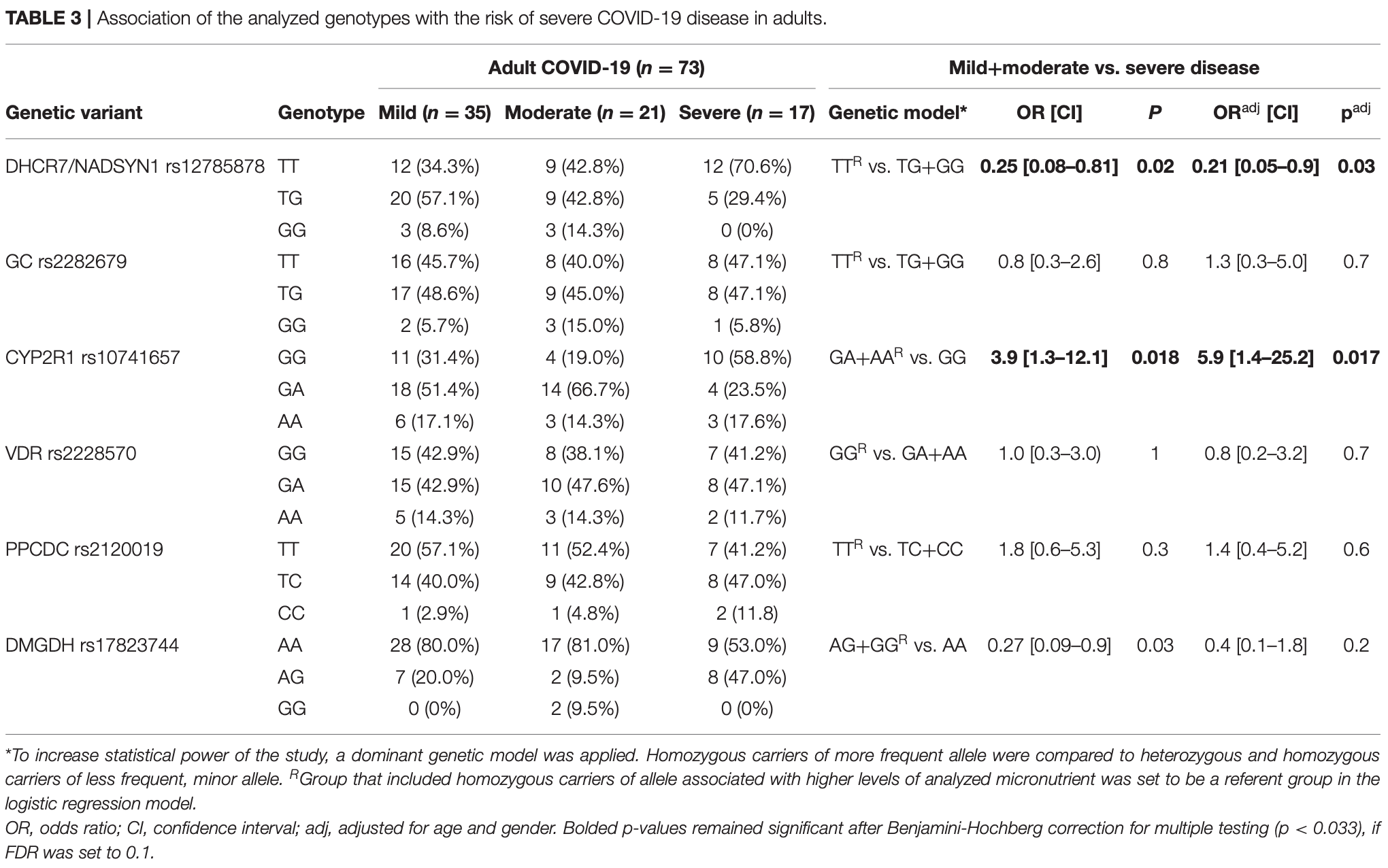 Kotur et al., 6/4/2021, peer-reviewed, 13 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Fasano et al., Movement Disorders, doi:10.1002/mds.28176 (Peer Reviewed) | cases, ↓42.0%, p=0.05 | COVID-19 in Parkinson's Disease Patients Living in Lombardy, Italy |
| Details Retrospective phone survey of 1,486 Parkinson's disease patients in Italy, showing lower risk of COVID-19 cases with vitamin D supplementation. This paper also presents a case control study of PD patients and family member control patients. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Fasano et al., Movement Disorders, doi:10.1002/mds.28176 (Peer Reviewed) |
| COVID-19 in Parkinson's Disease Patients Living in Lombardy, Italy |
Retrospective phone survey of 1,486 Parkinson's disease patients in Italy, showing lower risk of COVID-19 cases with vitamin D supplementation. This paper also presents a case control study of PD patients and family member control patients. 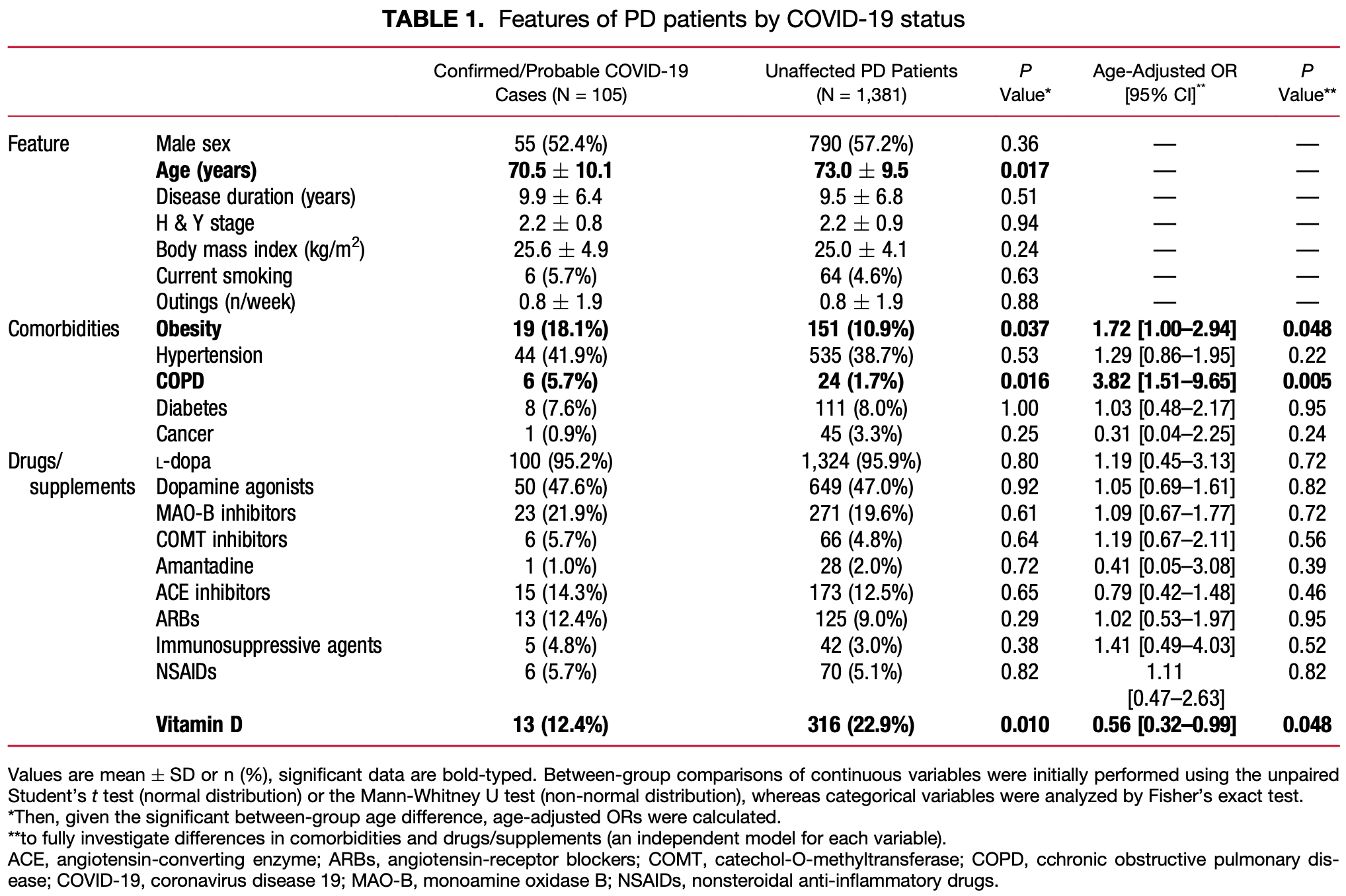 risk of case, 42.0% lower, RR 0.58, p = 0.05, treatment 13 of 329 (4.0%), control 92 of 1,157 (8.0%), OR converted to RR. Fasano et al., 6/2/2021, retrospective, Italy, Europe, peer-reviewed, 7 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Butler-Laporte et al., PLOS Medicine, doi:10.1371/journal.pmed.1003605 (Peer Reviewed) | Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: A Mendelian randomization study |
| Details Mendelian randomization study not finding significant differences in COVID-19 outcomes based on vitamin D level. This study does not compare patients with deficiency/insuffiency/sufficiency, only providing ORs for increase in D levels. Au.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Butler-Laporte et al., PLOS Medicine, doi:10.1371/journal.pmed.1003605 (Peer Reviewed) |
| Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: A Mendelian randomization study |
Mendelian randomization study not finding significant differences in COVID-19 outcomes based on vitamin D level. This study does not compare patients with deficiency/insuffiency/sufficiency, only providing ORs for increase in D levels. Authors note that their results do not apply to individuals with vitamin D deficiency.For some background on Mendelian randomization studies and their limitations see [1].For reasons why Mendelian randomization may fail in this case, see [2]. Authors suggest that it may come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response. For most other purposes, it may not matter much that unbound (free) 25-OHD is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25-OHD and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all.Authors cite only 2 of the 25 vitamin D treatment studies (2 of 5 RCTs), including the only study reporting a negative effect. Authors indicate that they believe Murai et al. was a significant result, however that study used cholecalciferol with very late stage patients. In practice, calcifediol/calcitrol would be used due to the long delay in conversion of cholecalciferol, hence the study is not informative of either normal late stage treatment, or earlier treatment. That authors believe the study is important suggests a strong bias. 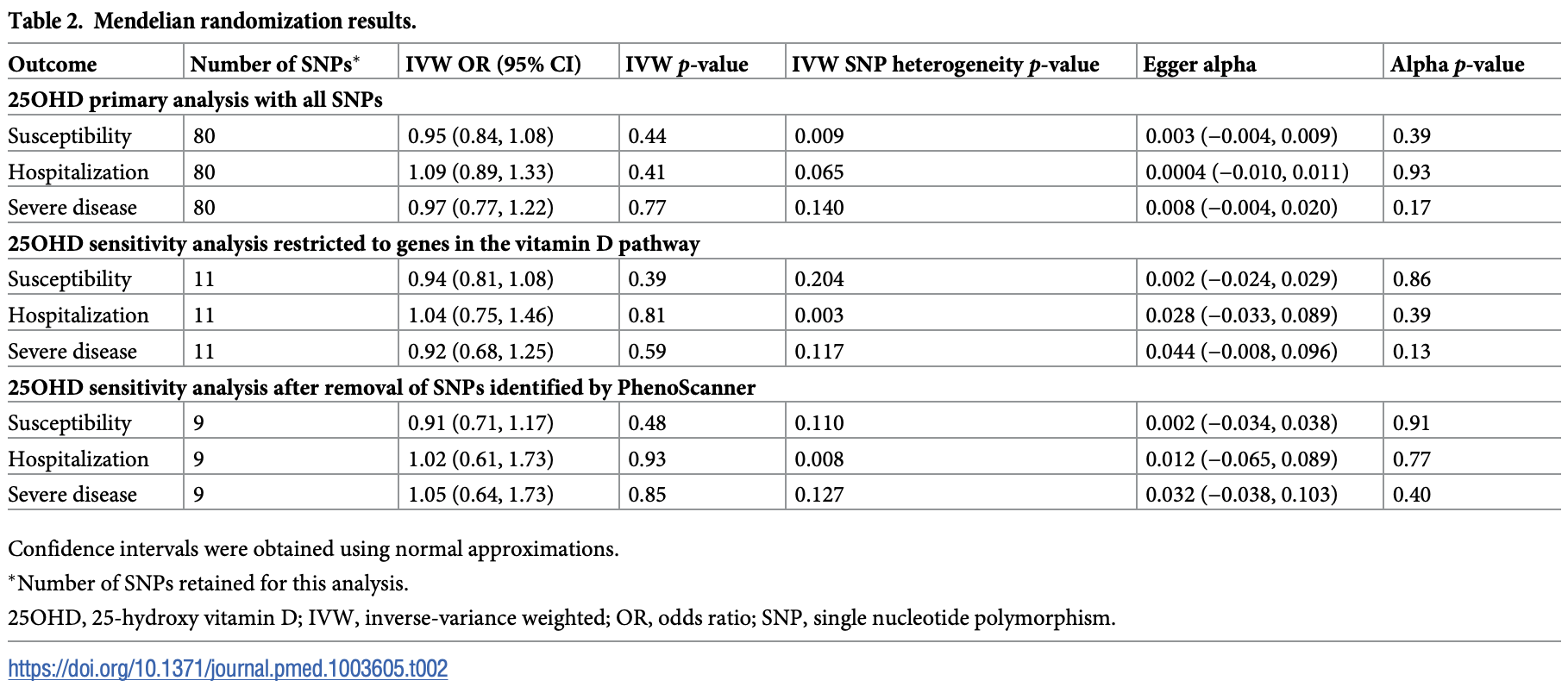 Butler-Laporte et al., 6/1/2021, peer-reviewed. |
| Submit Corrections or Comments |
| Levels | Pimental et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.021 (Peer Reviewed) | death, ↓29.4%, p=1.00 | Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19 |
| Details Retrospective 25 ICU patients in Brazil, showing vitamin D deficiency associated with higher neutrophil-lymphocyte ratio. There appears to be a typo in the mortality percentage for vitamin D deficiency (20% is not valid for the group size.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Pimental et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.021 (Peer Reviewed) |
| Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19 |
Retrospective 25 ICU patients in Brazil, showing vitamin D deficiency associated with higher neutrophil-lymphocyte ratio. There appears to be a typo in the mortality percentage for vitamin D deficiency (20% is not valid for the group size of 8). 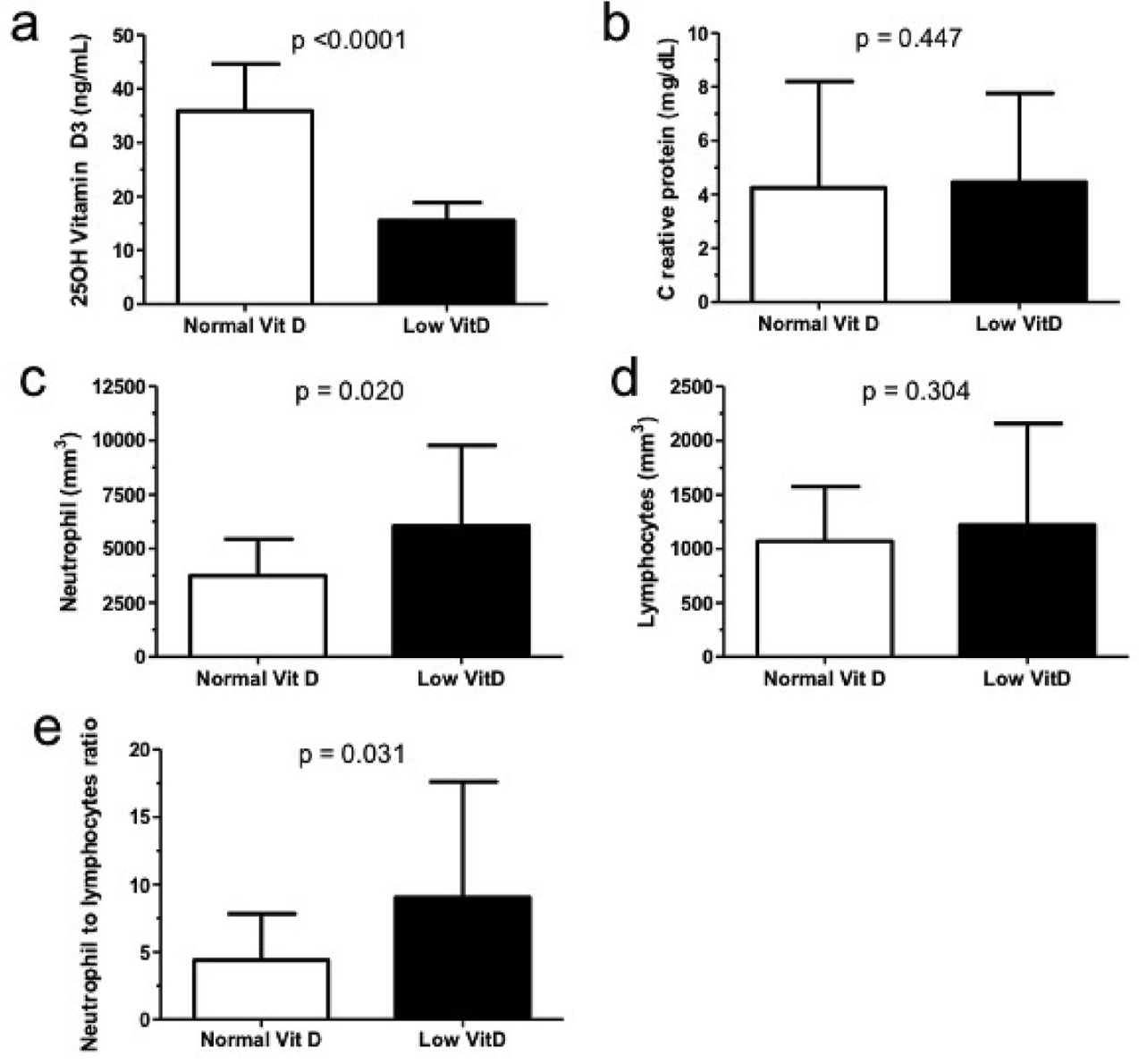 risk of death, 29.4% lower, RR 0.71, p = 1.00, high D levels 3 of 17 (17.6%), low D levels 2 of 8 (25.0%), >20ng/mL. Pimental et al., 5/31/2021, retrospective, Brazil, South America, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Sooriyaarachchi et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.011 (Peer Reviewed) | Impact of vitamin D deficiency on COVID-19 |
| Details Analysis of vitamin D deficiency and COVID-19 cases and deaths in 47 countries, showing vitamin D deficiency significantly associated with mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Sooriyaarachchi et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.011 (Peer Reviewed) |
| Impact of vitamin D deficiency on COVID-19 |
Analysis of vitamin D deficiency and COVID-19 cases and deaths in 47 countries, showing vitamin D deficiency significantly associated with mortality. 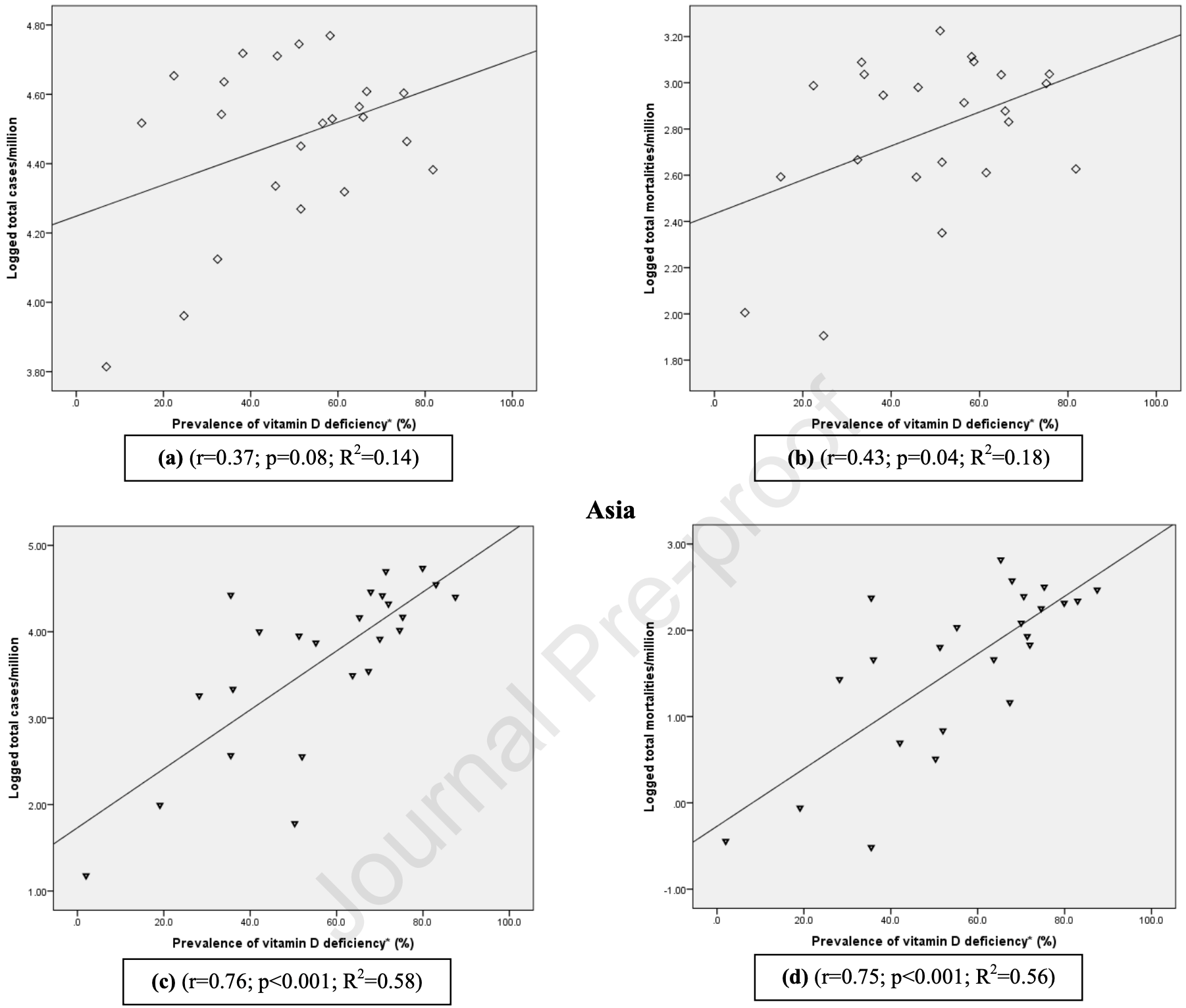 Sooriyaarachchi et al., 5/29/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Early | Sánchez-Zuno, J. Clinical Medicine, doi:10.3390/jcm10112378 (Peer Reviewed) | severe case, ↓89.4%, p=0.04 | Vitamin D Levels in COVID-19 Outpatients from Western Mexico: Clinical Correlation and Effect of Its Supplementation |
| Details Very small 42 PCR+ outpatient RCT in Mexico, 22 treated with vitamin D. Most patients had insufficient vitamin D levels, there were more symptoms in those with insufficient levels, and there were less cases with fever or with >3 symptoms .. |
| Details Source PDF Early treatment study Early treatment study |
| Sánchez-Zuno, J. Clinical Medicine, doi:10.3390/jcm10112378 (Peer Reviewed) |
| Vitamin D Levels in COVID-19 Outpatients from Western Mexico: Clinical Correlation and Effect of Its Supplementation |
Very small 42 PCR+ outpatient RCT in Mexico, 22 treated with vitamin D. Most patients had insufficient vitamin D levels, there were more symptoms in those with insufficient levels, and there were less cases with fever or with >3 symptoms at day 14 for treatment with vitamin D. 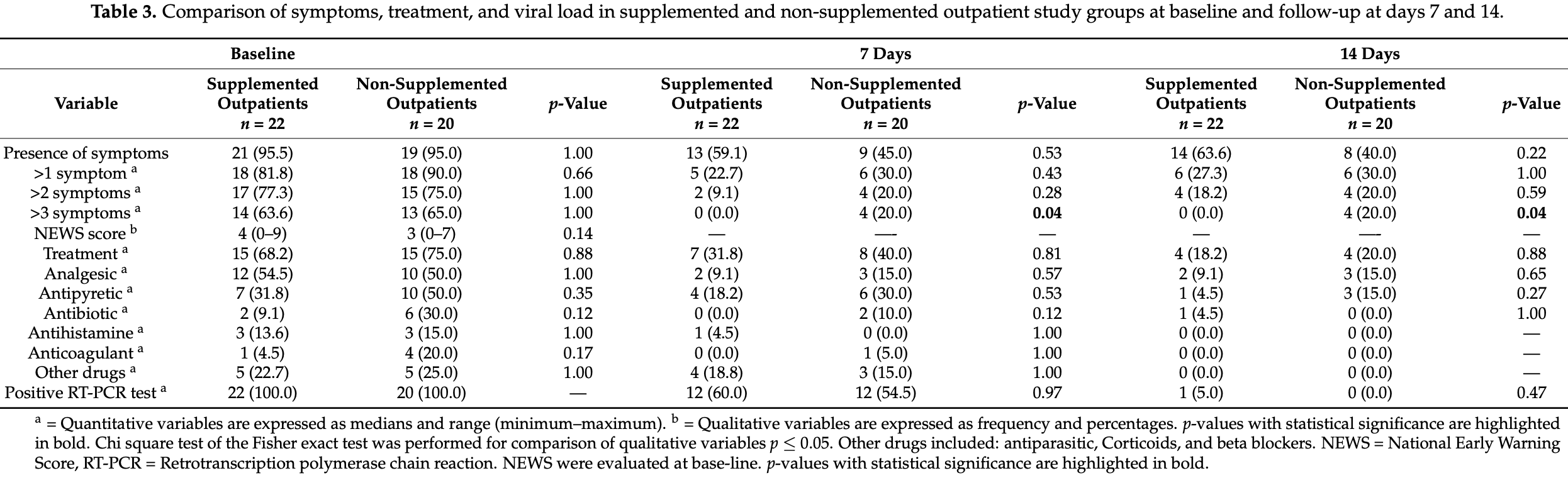 risk of severe case, 89.4% lower, RR 0.11, p = 0.04, treatment 0 of 22 (0.0%), control 4 of 20 (20.0%), relative risk is not 0 because of continuity correction due to zero events, risk of >3 symptoms at day 14. risk of no recovery, 80.8% lower, RR 0.19, p = 0.22, treatment 0 of 22 (0.0%), control 2 of 20 (10.0%), relative risk is not 0 because of continuity correction due to zero events, risk of fever at day 14, Table S1. Sánchez-Zuno et al., 5/28/2021, Randomized Controlled Trial, Mexico, North America, peer-reviewed, 12 authors, dosage 10,000IU days 1-14. |
| Submit Corrections or Comments |
| In Silico | Al-Mazaideh et al., Journal of Pharmaceutical Research International, doi:10.9734/jpri/2021/v33i29B31603 (Peer Reviewed) | Vitamin D is a New Promising Inhibitor to the Main Protease (Mpro) of COVID-19 by Molecular Docking |
| Details In Silico study showing vitamin D binding with Mpro of SARS-CoV-2. Among the compounds tested, vitamin D had the highest potential interaction in terms of total H-bond, van der Waal, torsional, and desolvation energy. Authors recommend ad.. |
| Details Source PDF In Silico In Silico |
| Al-Mazaideh et al., Journal of Pharmaceutical Research International, doi:10.9734/jpri/2021/v33i29B31603 (Peer Reviewed) |
| Vitamin D is a New Promising Inhibitor to the Main Protease (Mpro) of COVID-19 by Molecular Docking |
In Silico study showing vitamin D binding with Mpro of SARS-CoV-2. Among the compounds tested, vitamin D had the highest potential interaction in terms of total H-bond, van der Waal, torsional, and desolvation energy. Authors recommend adding vitamin D to COVID-19 treatment protocols. 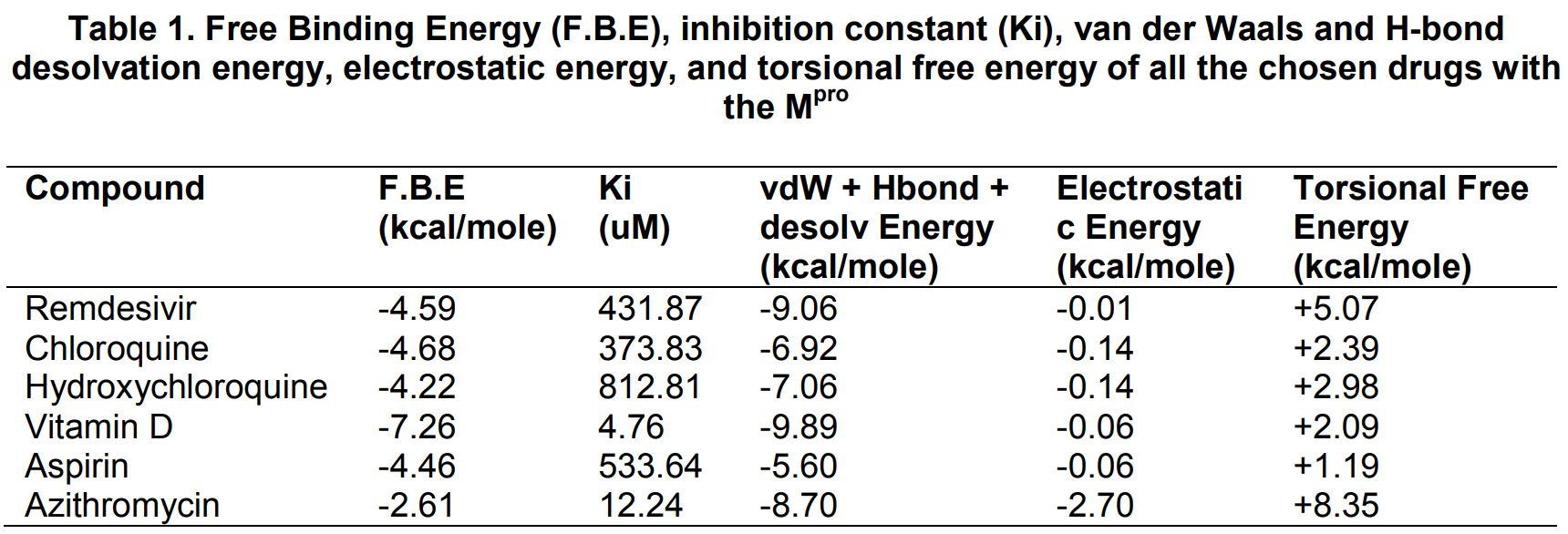 Al-Mazaideh et al., 5/26/2021, peer-reviewed, 4 authors. In Silico studies are an important part of preclinical research, however results may be very different in vivo. |
| Submit Corrections or Comments |
| Levels | Papadimitriou et al., World J. Virology, doi:10.5501/wjv.v10.i3.111] (Peer Reviewed) | Association between population vitamin D status and SARS-CoV-2 related serious-critical illness and deaths: An ecological integrative approach |
| Details Country analysis showing negative correlations between population vitamin D level and severe cases and death (but not with cases overall). Authors conclude that higher vitamin D levels may protect from severe cases and death, even more so.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Papadimitriou et al., World J. Virology, doi:10.5501/wjv.v10.i3.111] (Peer Reviewed) |
| Association between population vitamin D status and SARS-CoV-2 related serious-critical illness and deaths: An ecological integrative approach |
Country analysis showing negative correlations between population vitamin D level and severe cases and death (but not with cases overall). Authors conclude that higher vitamin D levels may protect from severe cases and death, even more so in the elderly. 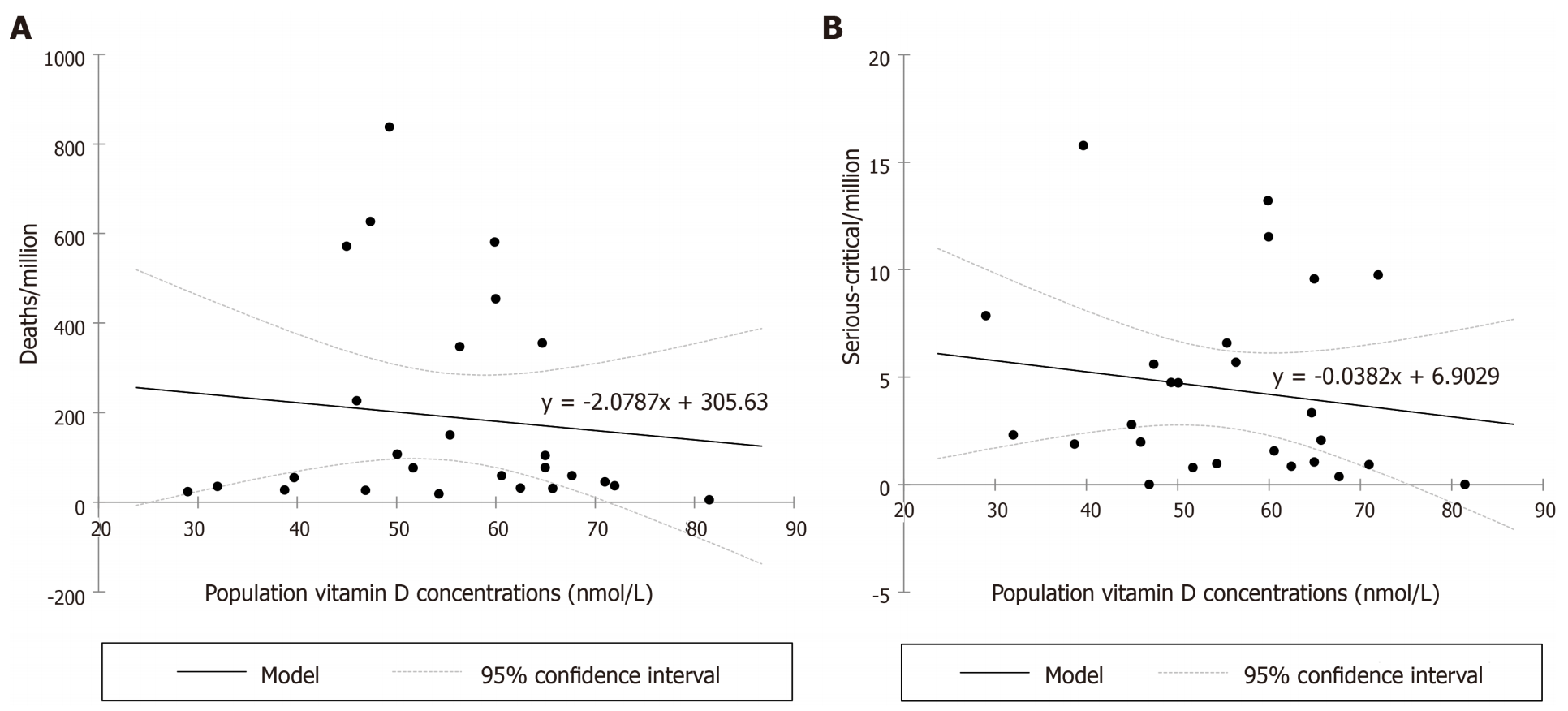 Papadimitriou et al., 5/25/2021, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Early | Asimi et al., Endocrine Abstracts, doi:10.1530/endoabs.73.PEP14.2 (Preprint) | ventilation, ↓97.4%, p<0.0001 | Selenium, zinc, and vitamin D supplementation affect the clinical course of COVID-19 infection in Hashimoto's thyroiditis |
| Details Retrospective 356 Hashimoto's thyroiditis outpatients, 270 taking vitamin D, zinc, and selenium, showing significantly lower hospitalization with treatment. Authors adjust for age, gender, BMI, and smoking status, reporting statistically .. |
| Details Source PDF Early treatment study Early treatment study |
| Asimi et al., Endocrine Abstracts, doi:10.1530/endoabs.73.PEP14.2 (Preprint) |
| Selenium, zinc, and vitamin D supplementation affect the clinical course of COVID-19 infection in Hashimoto's thyroiditis |
Retrospective 356 Hashimoto's thyroiditis outpatients, 270 taking vitamin D, zinc, and selenium, showing significantly lower hospitalization with treatment. Authors adjust for age, gender, BMI, and smoking status, reporting statistically significant associations with p<0.001 for hospitalization and mechanical ventilation, however they do not report the adjusted risks. 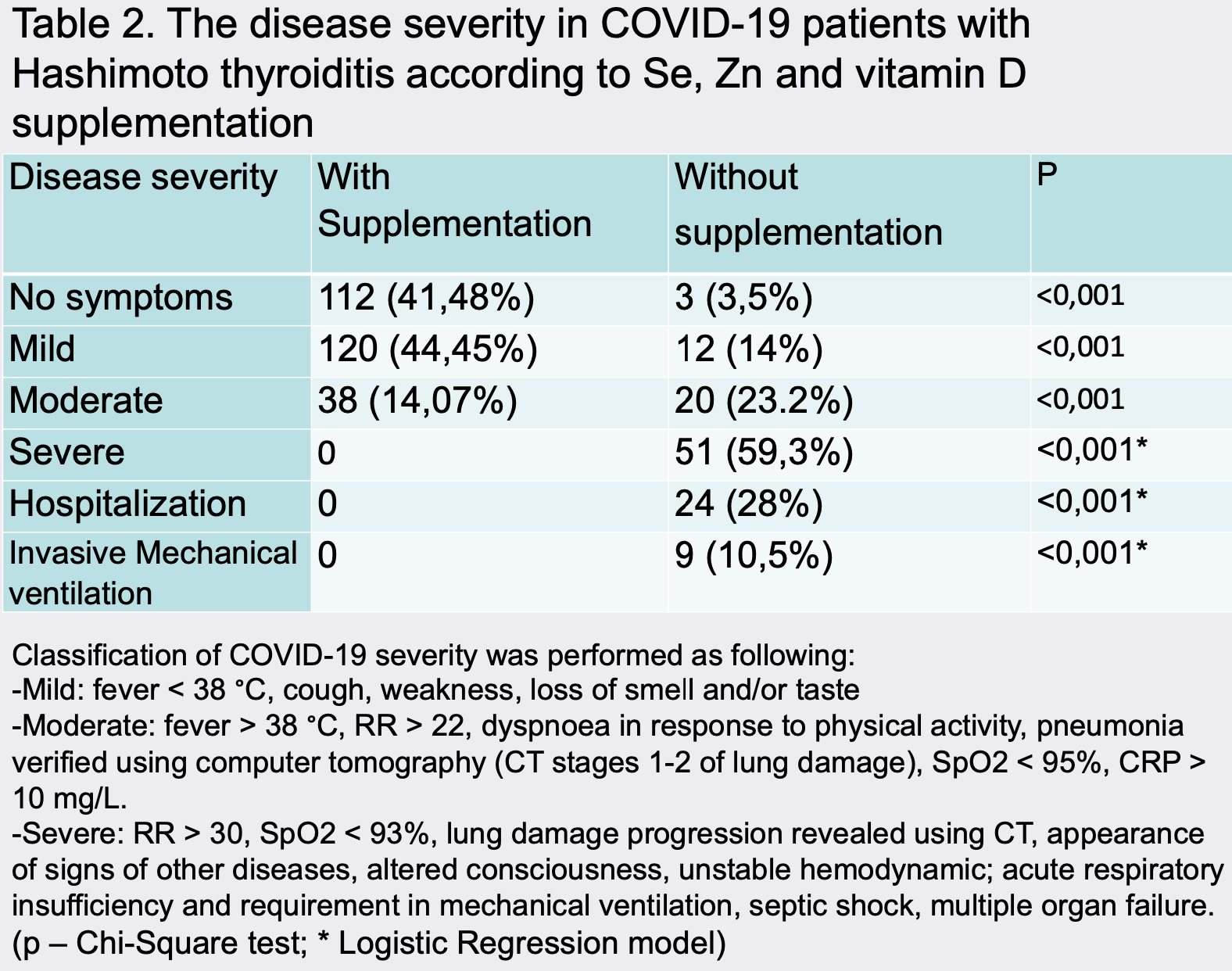 risk of mechanical ventilation, 97.4% lower, RR 0.03, p < 0.001, treatment 0 of 270 (0.0%), control 9 of 86 (10.5%), relative risk is not 0 because of continuity correction due to zero events, unadjusted. risk of hospitalization, 99.0% lower, RR 0.010, p < 0.001, treatment 0 of 270 (0.0%), control 24 of 86 (27.9%), relative risk is not 0 because of continuity correction due to zero events, unadjusted. risk of severe case, 99.5% lower, RR 0.005, p < 0.001, treatment 0 of 270 (0.0%), control 51 of 86 (59.3%), relative risk is not 0 because of continuity correction due to zero events, unadjusted. Excluded in after exclusion results of meta analysis: excessive unadjusted differences between groups. Asimi et al., 5/22/2021, retrospective, Bosnia and Herzegovina, Europe, preprint, 3 authors, dosage 2,000IU daily, this trial uses multiple treatments in the treatment arm (combined with zinc and selenium) - results of individual treatments may vary. |
| Submit Corrections or Comments |
| Late | Alcala-Diaz et al., Nutrients, doi:10.3390/nu13061760 (Peer Reviewed) | death, ↓80.8%, p=0.04 | Calcifediol Treatment and Hospital Mortality Due to COVID-19: A Cohort Study |
| Details Retrospective 537 patients in Spain, 79 treated with calcifediol, showing significantly lower mortality with treatment. The treated group had a higher risk of comorbidity, whereas the control group had lower O2 saturation, higher CURB‐65,.. |
| Details Source PDF Late treatment study Late treatment study |
| Alcala-Diaz et al., Nutrients, doi:10.3390/nu13061760 (Peer Reviewed) |
| Calcifediol Treatment and Hospital Mortality Due to COVID-19: A Cohort Study |
Retrospective 537 patients in Spain, 79 treated with calcifediol, showing significantly lower mortality with treatment. The treated group had a higher risk of comorbidity, whereas the control group had lower O2 saturation, higher CURB‐65, and higher ARDS (serverity measures were included in the multivariate analysis). 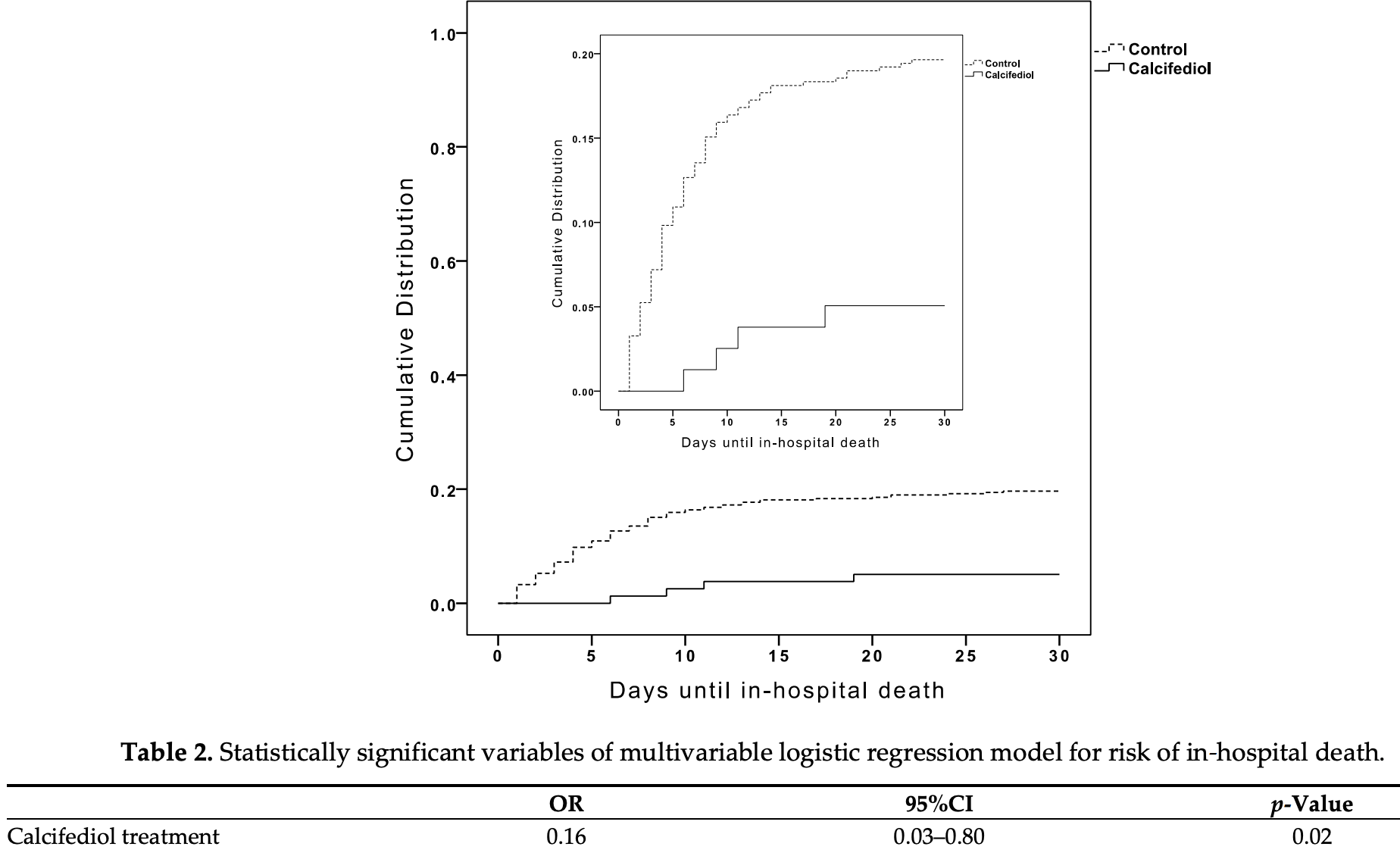 risk of death, 80.8% lower, RR 0.19, p = 0.04, treatment 4 of 79 (5.1%), control 90 of 458 (19.7%), adjusted, OR converted to RR, day 30, multivariate logistic regression. Alcala-Diaz et al., 5/21/2021, retrospective, Spain, Europe, peer-reviewed, 17 authors, dosage calcifediol 0.5mg day 1, 0.27mg day 3, 0.27mg day 7, 0.27mg day 14, 0.27mg day 21, 0.27mg day 28. |
| Submit Corrections or Comments |
| Levels | AlSafar et al., Nutrients, doi:10.3390/nu13051714 (Peer Reviewed) | death, ↓59.3%, p=0.05 | COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents |
| Details Retrospective 464 patients in United Arab Emirates showing low D levels at first hospital visit associated with higher COVID-19 severity and mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| AlSafar et al., Nutrients, doi:10.3390/nu13051714 (Peer Reviewed) |
| COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents |
Retrospective 464 patients in United Arab Emirates showing low D levels at first hospital visit associated with higher COVID-19 severity and mortality. 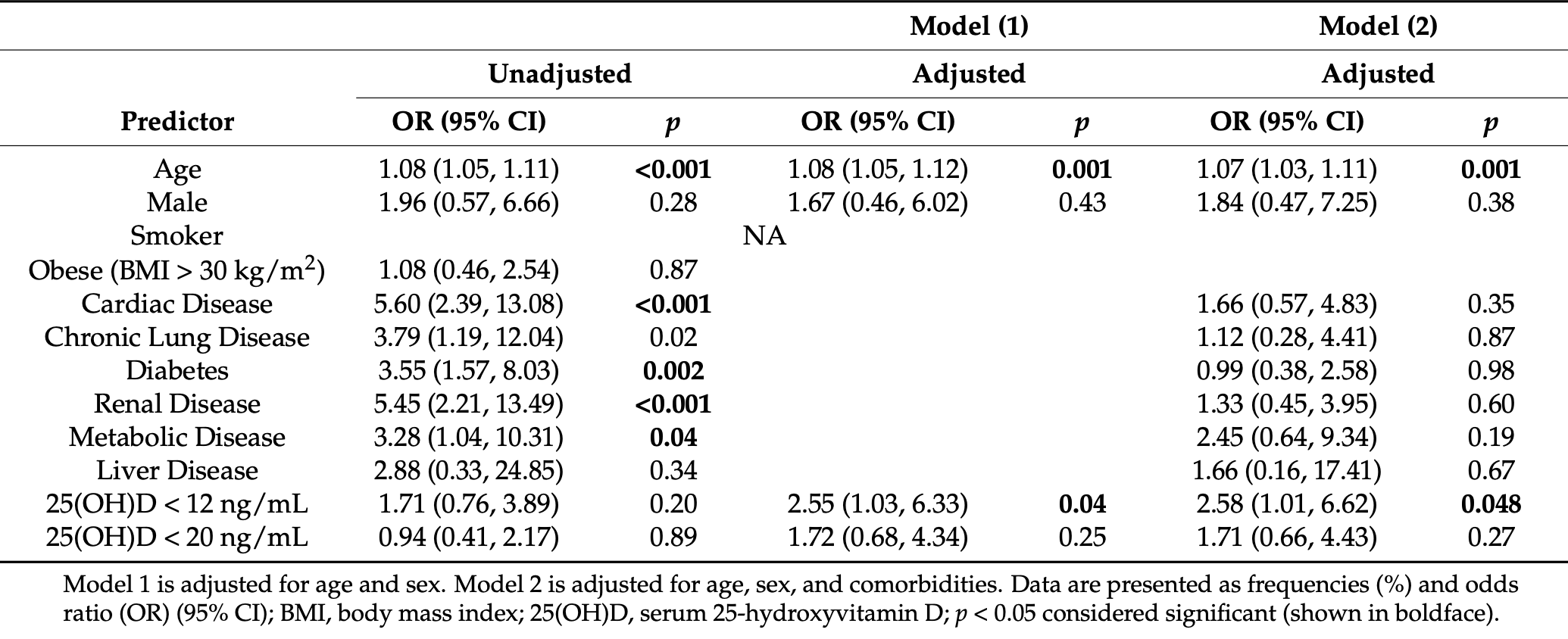 risk of death, 59.3% lower, RR 0.41, p = 0.05, high D levels 16 of 337 (4.7%), low D levels 10 of 127 (7.9%), adjusted, OR converted to RR, >=12ng/mL. risk of severe case, 33.2% lower, RR 0.67, p = 0.005, high D levels 337, low D levels 127, adjusted, OR converted to RR, >=12ng/mL. AlSafar et al., 5/19/2021, retrospective, United Arab Emirates, Middle East, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Li et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2021.11634 (Peer Reviewed) | cases, ↓8.6%, p=0.24 | Assessment of the Association of Vitamin D Level With SARS-CoV-2 Seropositivity Among Working-Age Adults |
| Details Cohort study of 18,148 patients in the USA showing low vitamin D associated with COVID-19 PCR+ status before adjustments but not after. Authors state that "low vitamin D levels were not independently associated with the risk of sero.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Li et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2021.11634 (Peer Reviewed) |
| Assessment of the Association of Vitamin D Level With SARS-CoV-2 Seropositivity Among Working-Age Adults |
Cohort study of 18,148 patients in the USA showing low vitamin D associated with COVID-19 PCR+ status before adjustments but not after.Authors state that "low vitamin D levels were not independently associated with the
risk of seropositivity", however there is significant correlation between some adjustment variables and vitamin D levels in the logistic regression that prevent drawing this conclusion [1]. Details of the logistic regression in the matched sample set are not provided.Authors analyze only 20ng/mL and 30ng/mL cutoff points, other studies use 10ng/mL (or 12), where more significant differences are typically seen. 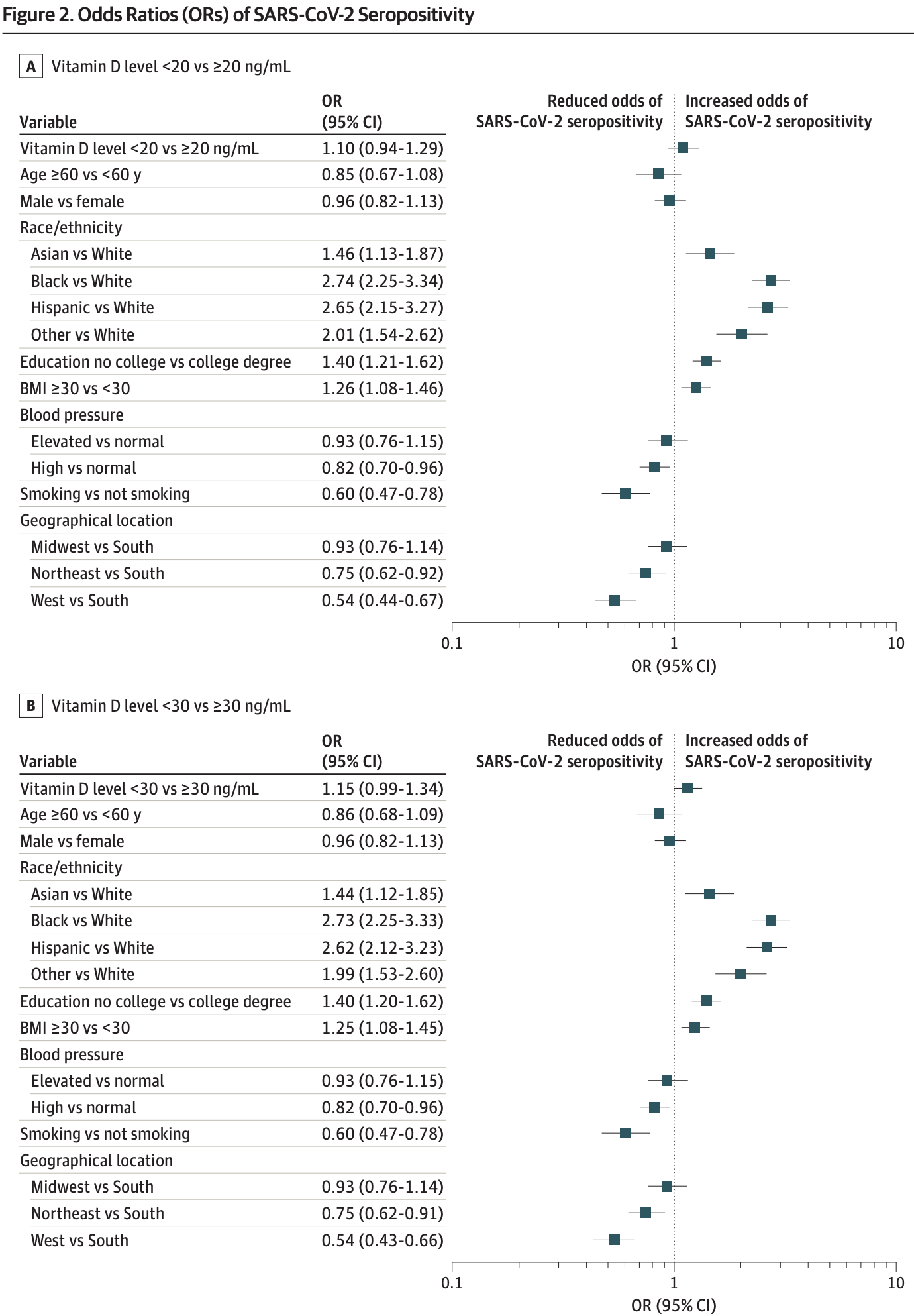 risk of case, 8.6% lower, RR 0.91, p = 0.24, high D levels 610 of 13,650 (4.5%), low D levels 290 of 4,498 (6.4%), adjusted, OR converted to RR, >20ng/mL, Figure 2. risk of case, 12.4% lower, RR 0.88, p = 0.07, high D levels 289 of 7,272 (4.0%), low D levels 611 of 10,876 (5.6%), adjusted, OR converted to RR, >30ng/mL, Figure 2. Li et al., 5/19/2021, retrospective, USA, North America, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Dudley et al., BJPsych Bulletin, doi:10.1192/bjb.2021.55 (Peer Reviewed) | symp. case, ↓22.4%, p=0.65 | Revisiting vitamin D status and supplementation for in-patients with intellectual and developmental disability in the North of England, UK |
| Details Retrospective 64 patients with intellectual and developmental disability in the UK, showing no sigificant difference in COVID-19 status with vitamin D supplementation. Only 6 patients were not on vitamin D supplementation. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Dudley et al., BJPsych Bulletin, doi:10.1192/bjb.2021.55 (Peer Reviewed) |
| Revisiting vitamin D status and supplementation for in-patients with intellectual and developmental disability in the North of England, UK |
Retrospective 64 patients with intellectual and developmental disability in the UK, showing no sigificant difference in COVID-19 status with vitamin D supplementation. Only 6 patients were not on vitamin D supplementation. risk of symptomatic case, 22.4% lower, RR 0.78, p = 0.65, treatment 15 of 58 (25.9%), control 2 of 6 (33.3%), positive test. Dudley et al., 5/18/2021, retrospective, United Kingdom, Europe, peer-reviewed, 5 authors, dosage 800IU daily. |
| Submit Corrections or Comments |
| Levels | Savitri et al., Annals of the Romanian Society for Cell Biology, 25:6 (Peer Reviewed) | symp. case, ↓88.0%, p<0.0001 | Comparison between Vitamin D Level of Asymptomatic Confirmed Covid-19 Patients with Symptomatic Confirmed Covid-19 Patients in Makassar |
| Details Retrospective 42 PCR+ patients in Indonesia, showing significantly higher risk of symptomatic cases with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Savitri et al., Annals of the Romanian Society for Cell Biology, 25:6 (Peer Reviewed) |
| Comparison between Vitamin D Level of Asymptomatic Confirmed Covid-19 Patients with Symptomatic Confirmed Covid-19 Patients in Makassar |
Retrospective 42 PCR+ patients in Indonesia, showing significantly higher risk of symptomatic cases with vitamin D deficiency. 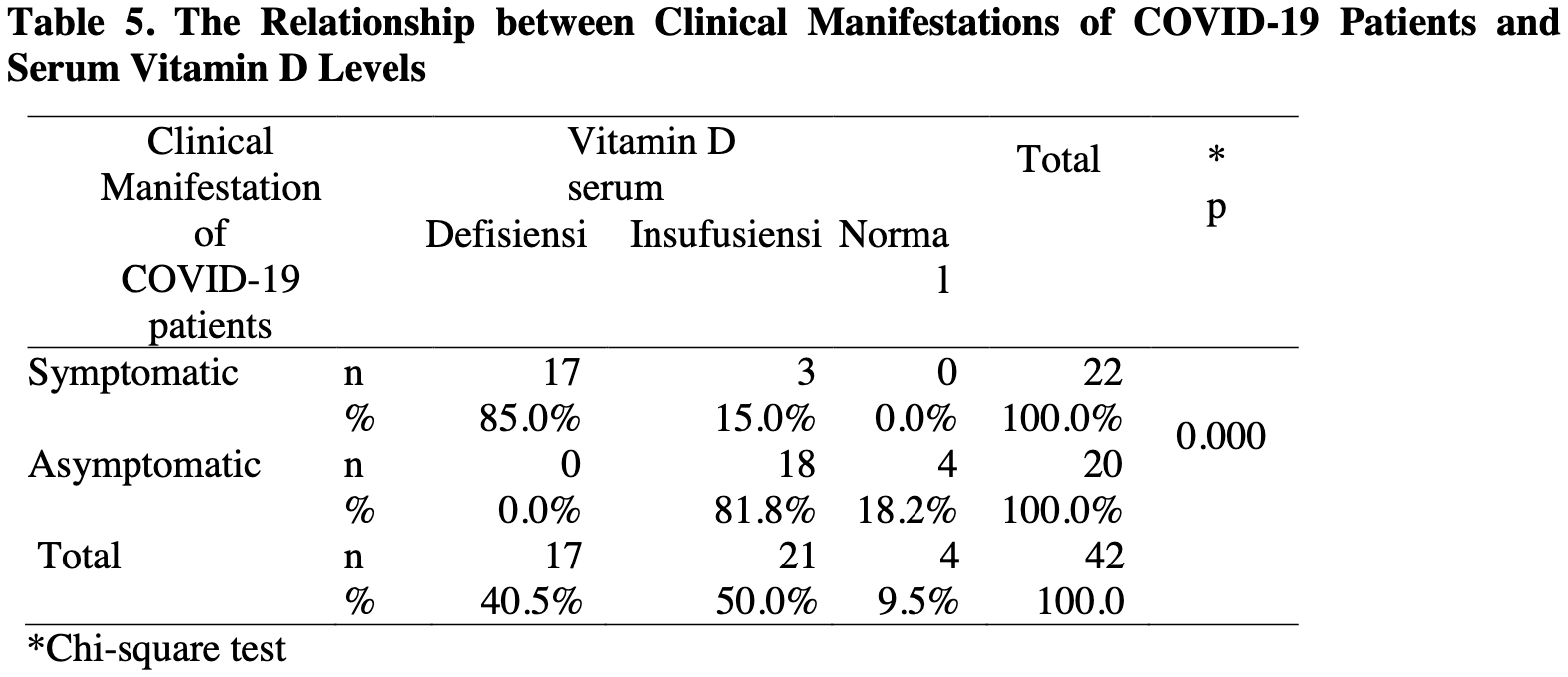 risk of symptomatic case, 88.0% lower, RR 0.12, p < 0.001, high D levels 3 of 25 (12.0%), low D levels 17 of 17 (100.0%), >20ng/ml. Savitri et al., 5/8/2021, retrospective, Indonesia, South Asia, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Levitus et al., Journal of the Endocrine Society, doi: 10.1210/jendso/bvab048.567 (Peer Reviewed) | severe case, ↓30.8%, p=0.25 | The Effect of Vitamin D Supplementation on Severe COVID-19 Outcomes in Patients With Vitamin D Insufficiency |
| Details Retrospective 129 hospitalized patients with vitamin D levels measured within 90 days prior to admission, showing lower, but not statistically significant, risk of severe cases with vitamin D supplementation among patients with levels <20.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Levitus et al., Journal of the Endocrine Society, doi: 10.1210/jendso/bvab048.567 (Peer Reviewed) |
| The Effect of Vitamin D Supplementation on Severe COVID-19 Outcomes in Patients With Vitamin D Insufficiency |
Retrospective 129 hospitalized patients with vitamin D levels measured within 90 days prior to admission, showing lower, but not statistically significant, risk of severe cases with vitamin D supplementation among patients with levels <20ng/mL or <12ng/mL. For <30ng/mL, lower (but not statistically significant) risk was seen overall but not for ≥50,000IU (the sample size is not given, it may be extremely small for this case). Only minimal details for <30ng/mL are provided, and no details for <20ng/mL or <12ng/mL are provided. The potential effect of supplementation on the risk of a case severe enough for hospitalization is not included. 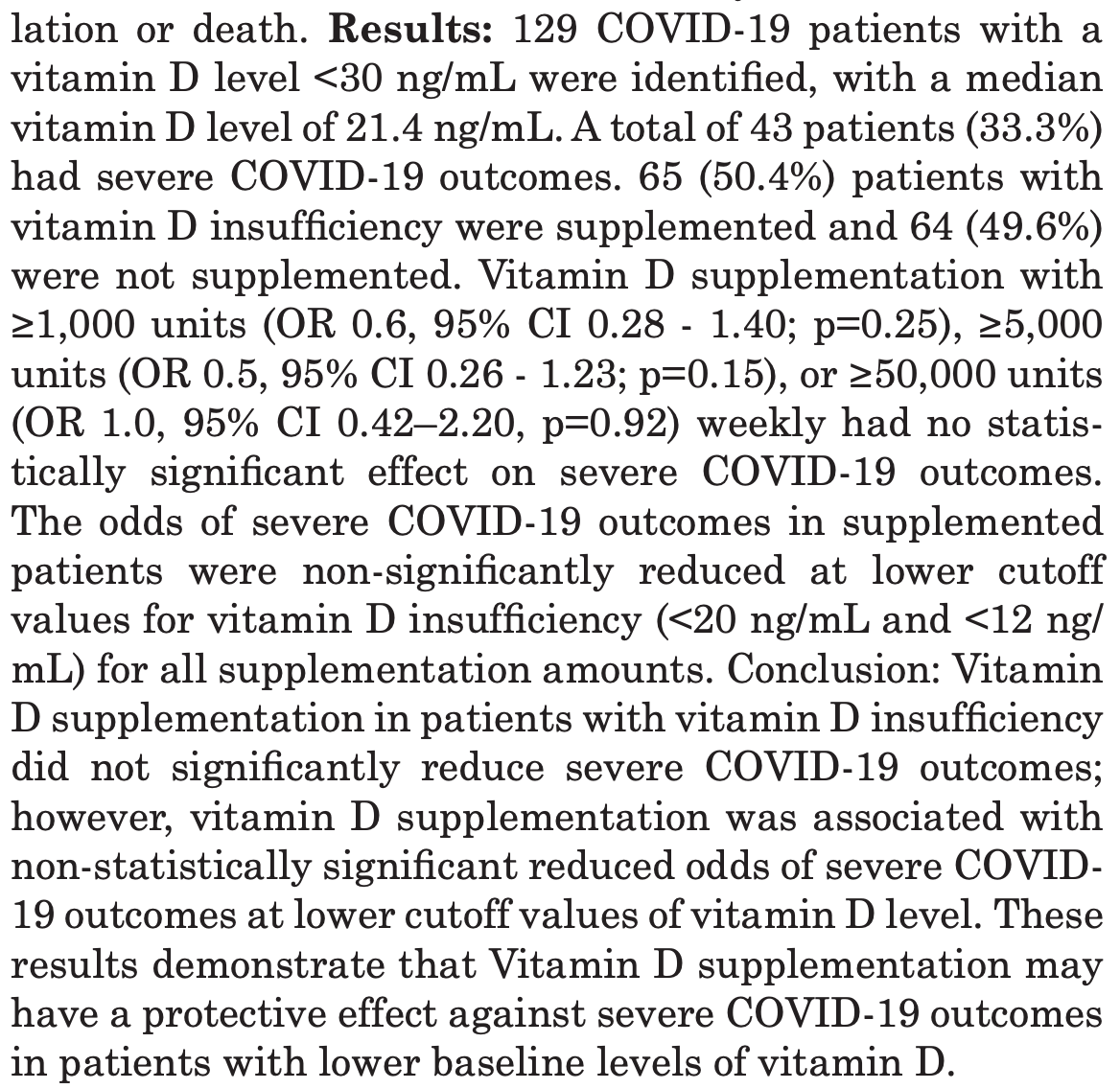 risk of severe case, 30.8% lower, RR 0.69, p = 0.25, treatment 65, control 64, OR converted to RR, ≥1,000IU, control prevalence approximated with overall prevalence. risk of severe case, 40.0% lower, RR 0.60, p = 0.15, treatment 65, control 64, OR converted to RR, ≥5,000IU, control prevalence approximated with overall prevalence. risk of severe case, no change, RR 1.00, p = 0.92, treatment 65, control 64, OR converted to RR, ≥50,000IU, control prevalence approximated with overall prevalence. Levitus et al., 5/3/2021, retrospective, USA, North America, peer-reviewed, 9 authors, dosage varies. |
| Submit Corrections or Comments |
| Early | Loucera et al., Scientific Reports, doi:10.1038/s41598-021-02701-5 (preprint 4/29/21) (Peer Reviewed) | death, ↓33.0%, p=0.009 | Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients |
| Details Retrospective 15,968 hospitalized patients in Spain showing a significant reduction in mortality associated with the prescription of vitamin D, especially calcifediol, within 15-30 days prior to hospitalization. |
| Details Source PDF Early treatment study Early treatment study |
| Loucera et al., Scientific Reports, doi:10.1038/s41598-021-02701-5 (preprint 4/29/21) (Peer Reviewed) |
| Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients |
Retrospective 15,968 hospitalized patients in Spain showing a significant reduction in mortality associated with the prescription of vitamin D, especially calcifediol, within 15-30 days prior to hospitalization. 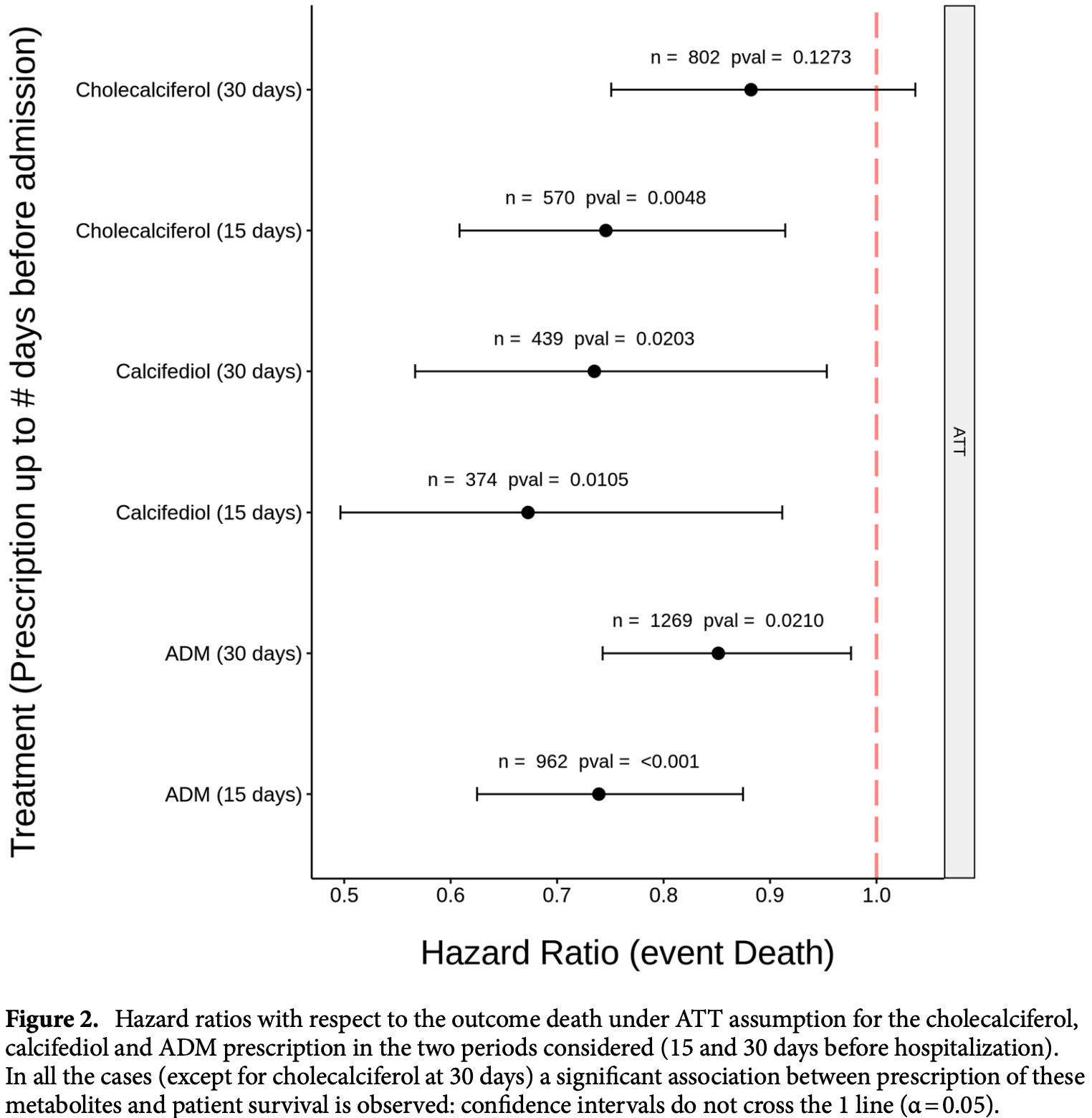 risk of death, 33.0% lower, RR 0.67, p = 0.009, treatment 374, control 374, calcifediol, <15 days before hospitalization, Cox model with inverse propensity weighting. risk of death, 27.0% lower, RR 0.73, p = 0.02, treatment 439, control 439, calcifediol, <30 days before hospitalization, Cox model with inverse propensity weighting. risk of death, 25.0% lower, RR 0.75, p = 0.005, treatment 570, control 570, cholecalciferol, <15 days before hospitalization, Cox model with inverse propensity weighting. risk of death, 12.0% lower, RR 0.88, p = 0.11, treatment 802, control 802, cholecalciferol, <30 days before hospitalization, Cox model with inverse propensity weighting. Loucera et al., 4/29/2021, retrospective, propensity score matching, Spain, Europe, peer-reviewed, 11 authors, dosage varies (calcifediol). |
| Submit Corrections or Comments |
| Levels | Al-Daghri et al., Journal of Translational Medicine, doi:10.1186/s12967-021-02838-x (Peer Reviewed) | Vitamin D status of Arab Gulf residents screened for SARS-CoV-2 and its association with COVID-19 infection: a multi-centre case–control study |
| Details Case control study with 220 adults showing significantly lower vitamin D levels in PCR+ patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Al-Daghri et al., Journal of Translational Medicine, doi:10.1186/s12967-021-02838-x (Peer Reviewed) |
| Vitamin D status of Arab Gulf residents screened for SARS-CoV-2 and its association with COVID-19 infection: a multi-centre case–control study |
Case control study with 220 adults showing significantly lower vitamin D levels in PCR+ patients. 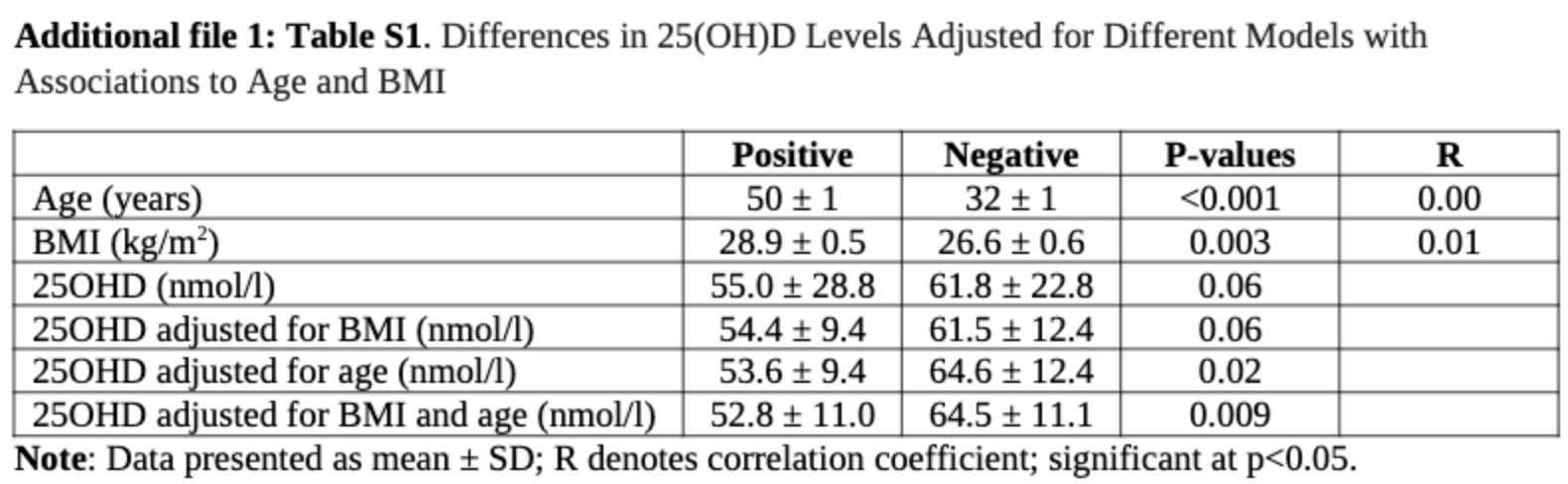 Al-Daghri et al., 4/26/2021, peer-reviewed, 13 authors. |
| Submit Corrections or Comments |
| Levels | Elham et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.03.040 (Peer Reviewed) | Serum vitamin D, calcium, and zinc levels in patients with COVID-19 |
| Details Case control study with 93 hospitalized patients in Iran and 186 control patients, showing significantly lower vitamin D, zinc, and calcium levels in cases. IR.SHOUSHTAR.REC.1399.017. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Elham et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.03.040 (Peer Reviewed) |
| Serum vitamin D, calcium, and zinc levels in patients with COVID-19 |
Case control study with 93 hospitalized patients in Iran and 186 control patients, showing significantly lower vitamin D, zinc, and calcium levels in cases. IR.SHOUSHTAR.REC.1399.017. 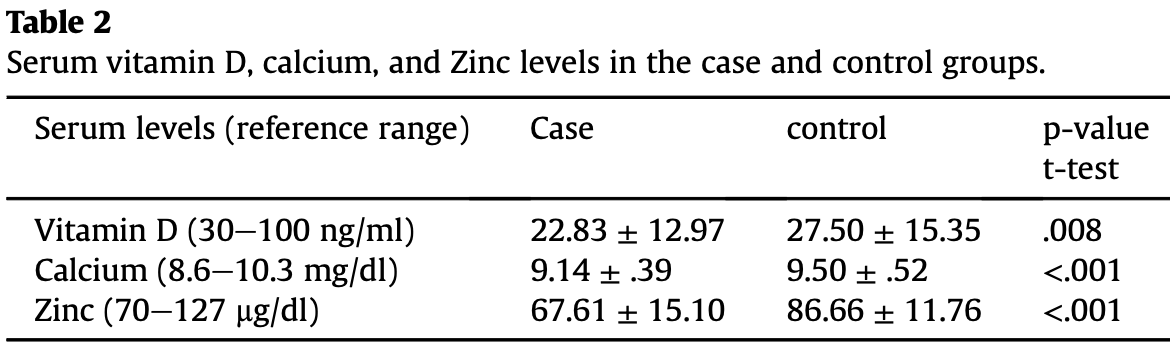 Elham et al., 4/18/2021, retrospective, case control, Iran, Middle East, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Review | Shah Alam et al., International Immunopharmacology, doi:10.1016/j.intimp.2021.107686 (Review) (Peer Reviewed) | review | The role of vitamin D in reducing SARS-CoV-2 infection: An update |
| Details Review of vitamin D for COVID-19 noting that infections are likely to be more prevalent in the winter season; clinical trials show vitamin D as a potential therapeutic agent; vitamin D is beneficial against COVID-19 by reducing inflammato.. |
| Details Source PDF Review Review |
| Shah Alam et al., International Immunopharmacology, doi:10.1016/j.intimp.2021.107686 (Review) (Peer Reviewed) |
| The role of vitamin D in reducing SARS-CoV-2 infection: An update |
Review of vitamin D for COVID-19 noting that infections are likely to be more prevalent in the winter season; clinical trials show vitamin D as a potential therapeutic agent; vitamin D is beneficial against COVID-19 by reducing inflammatory response; vitamin D boosts immune response against SARS-CoV-2 infection; and vitamin D deficiency increases the risk of COVID-19 severity and mortality. 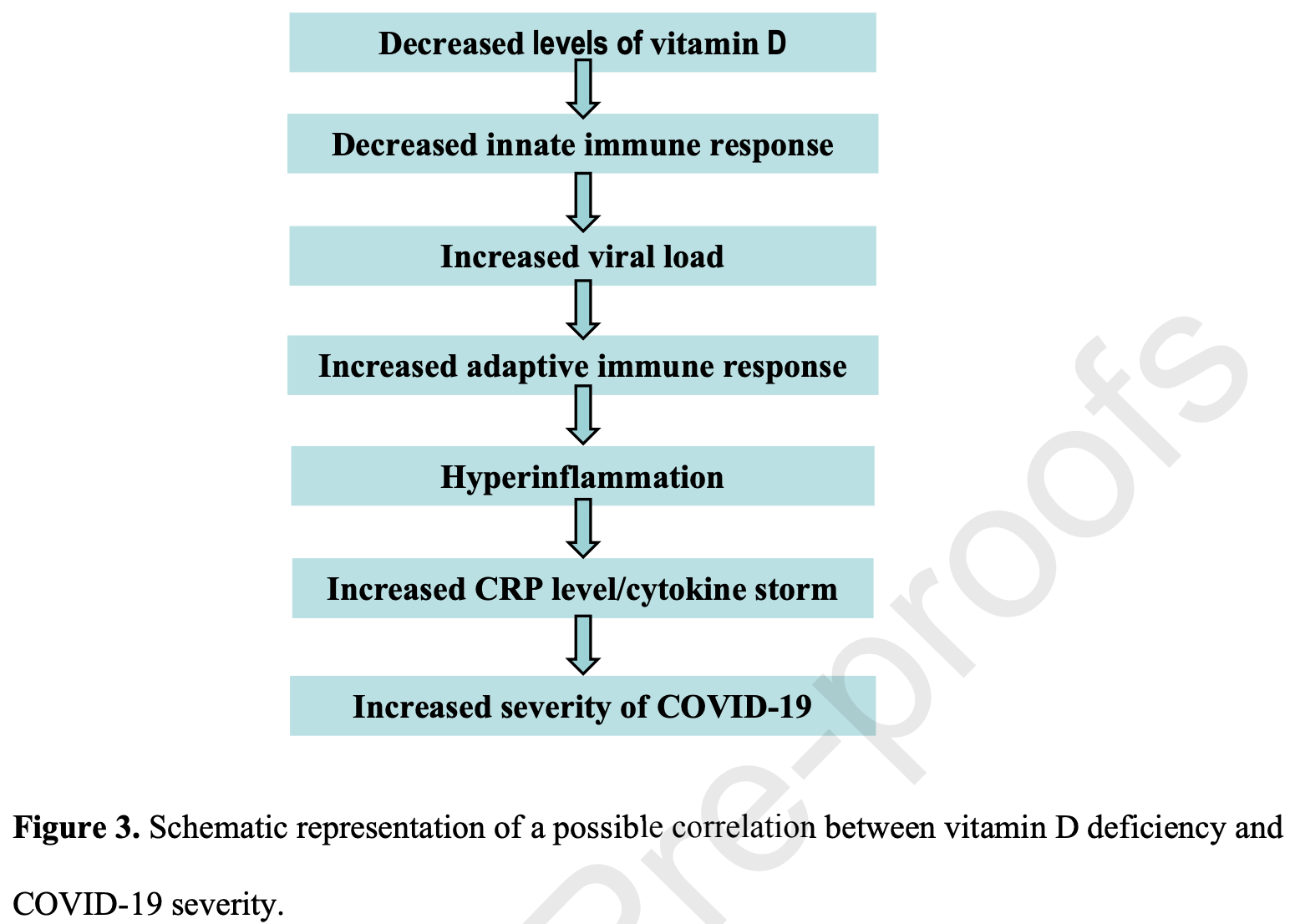 Shah Alam et al., 4/17/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Oristrell et al., Biomedicines, doi:10.3390/biomedicines9050509 (preprint 4/6/21) (Peer Reviewed) | death, ↓43.0%, p=0.001 | Association of Calcitriol Supplementation with Reduced COVID-19 Mortality in Patients with Chronic Kidney Disease: A Population-based Study |
| Details Retrospective study of calcitriol supplementation with chronic kidney disease patients in Catalonia showing lower cases, severe cases, and mortality with supplementation. A dose-response relationship was found for severe cases and mortali.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Oristrell et al., Biomedicines, doi:10.3390/biomedicines9050509 (preprint 4/6/21) (Peer Reviewed) |
| Association of Calcitriol Supplementation with Reduced COVID-19 Mortality in Patients with Chronic Kidney Disease: A Population-based Study |
Retrospective study of calcitriol supplementation with chronic kidney disease patients in Catalonia showing lower cases, severe cases, and mortality with supplementation. A dose-response relationship was found for severe cases and mortality. 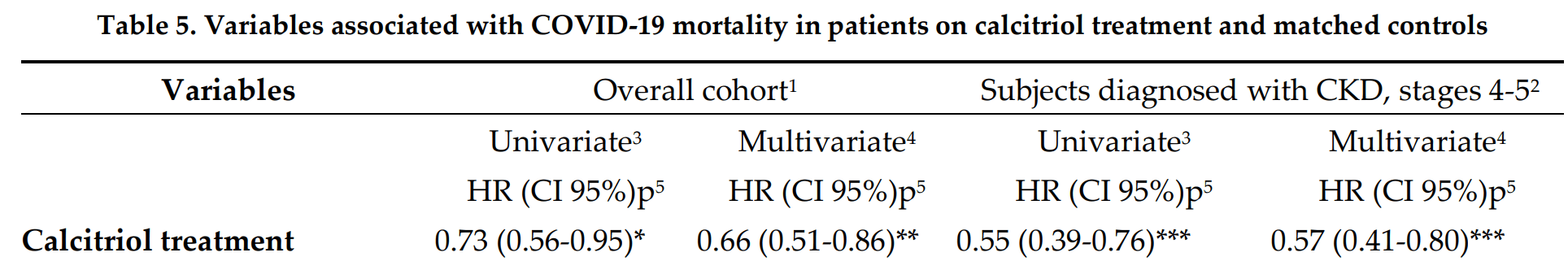 risk of death, 43.0% lower, RR 0.57, p = 0.001, treatment 2,296, control 3,407, multivariate, patients with CKD stages 4-5. risk of severe case, 43.0% lower, RR 0.57, p < 0.001, treatment 2,296, control 3,407, multivariate, patients with CKD stages 4-5. risk of case, 22.0% lower, RR 0.78, p = 0.01, treatment 163 of 2,296 (7.1%), control 326 of 3,407 (9.6%), multivariate, patients with CKD stages 4-5. Oristrell et al., 4/6/2021, retrospective, Spain, Europe, peer-reviewed, 10 authors, dosage calcitriol 0.3μg daily, mean daily dose. |
| Submit Corrections or Comments |
| Levels | Ünsal et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01566-9 (Peer Reviewed) | death, ↓80.6%, p=0.23 | Retrospective analysis of vitamin D status on ınflammatory markers and course of the disease in patients with COVID-19 infection |
| Details Retrospective 56 patients in Turkey showing greater need for oxygen therapy and higher mortality with vitamin D deficiency, and significantly lower risk of pneumonia with vitamin D supplementation. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ünsal et al., Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01566-9 (Peer Reviewed) |
| Retrospective analysis of vitamin D status on ınflammatory markers and course of the disease in patients with COVID-19 infection |
Retrospective 56 patients in Turkey showing greater need for oxygen therapy and higher mortality with vitamin D deficiency, and significantly lower risk of pneumonia with vitamin D supplementation. 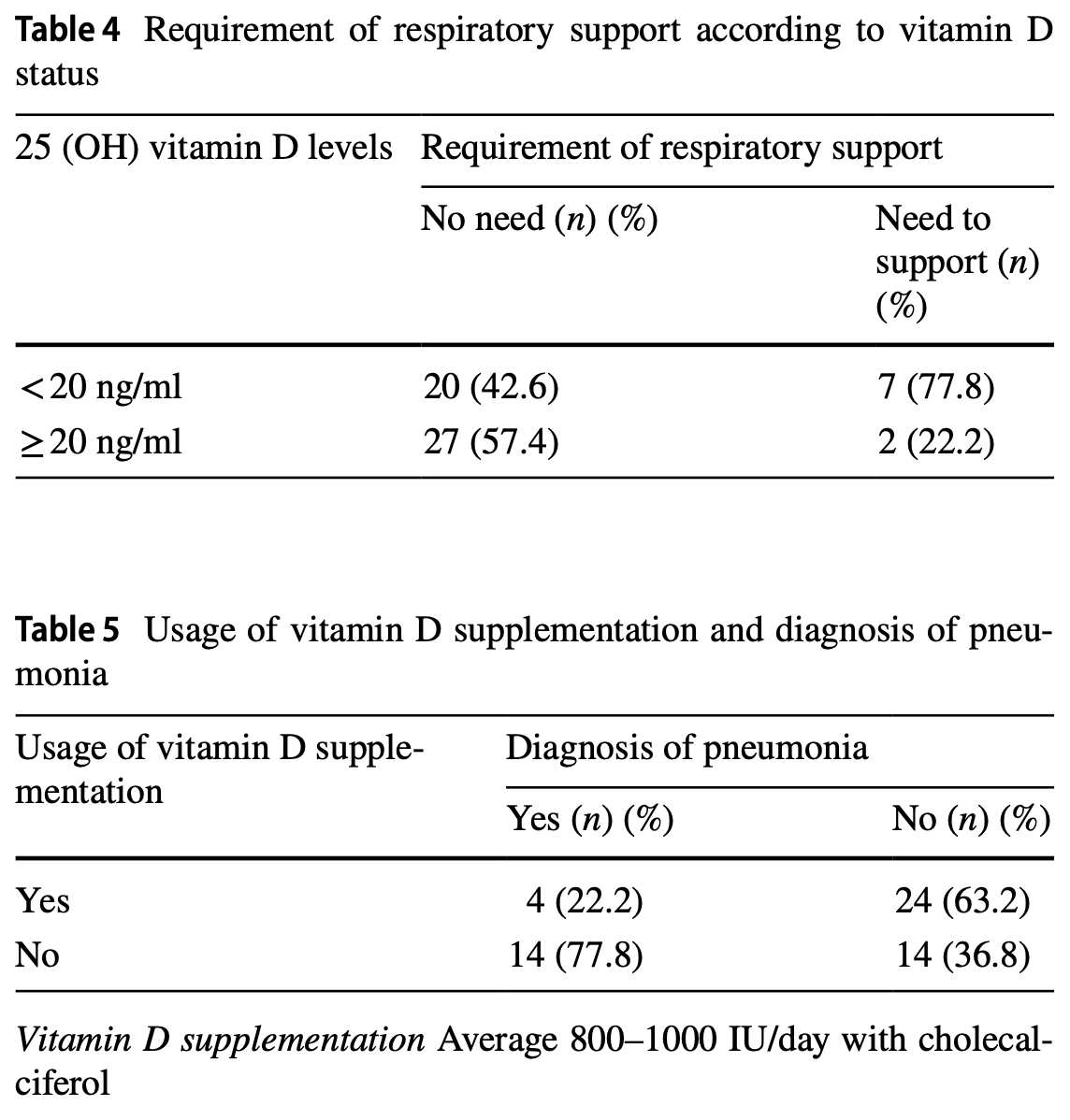 risk of death, 80.6% lower, RR 0.19, p = 0.23, high D levels 0 of 29 (0.0%), low D levels 2 of 27 (7.4%), relative risk is not 0 because of continuity correction due to zero events, >=20ng/mL. risk of oxygen therapy, 73.4% lower, RR 0.27, p = 0.07, high D levels 2 of 29 (6.9%), low D levels 7 of 27 (25.9%), >=20ng/mL. Ünsal et al., 4/5/2021, retrospective, Turkey, Europe, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Levels | Livingston et al., Int. J. Clinical Practive, doi:10.1111/ijcp.14166 (Peer Reviewed) | cases, ↓50.9%, p=0.02 | Detectable respiratory SARS‐CoV‐2 RNA is associated with low vitamin D levels and high social deprivation |
| Details Retrospective 104 consecutive patients tested for COVID-19 in a hospital in the UK, showing lower vitamin D and higher social deprivation associated with COVID-19 positive results. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Livingston et al., Int. J. Clinical Practive, doi:10.1111/ijcp.14166 (Peer Reviewed) |
| Detectable respiratory SARS‐CoV‐2 RNA is associated with low vitamin D levels and high social deprivation |
Retrospective 104 consecutive patients tested for COVID-19 in a hospital in the UK, showing lower vitamin D and higher social deprivation associated with COVID-19 positive results. 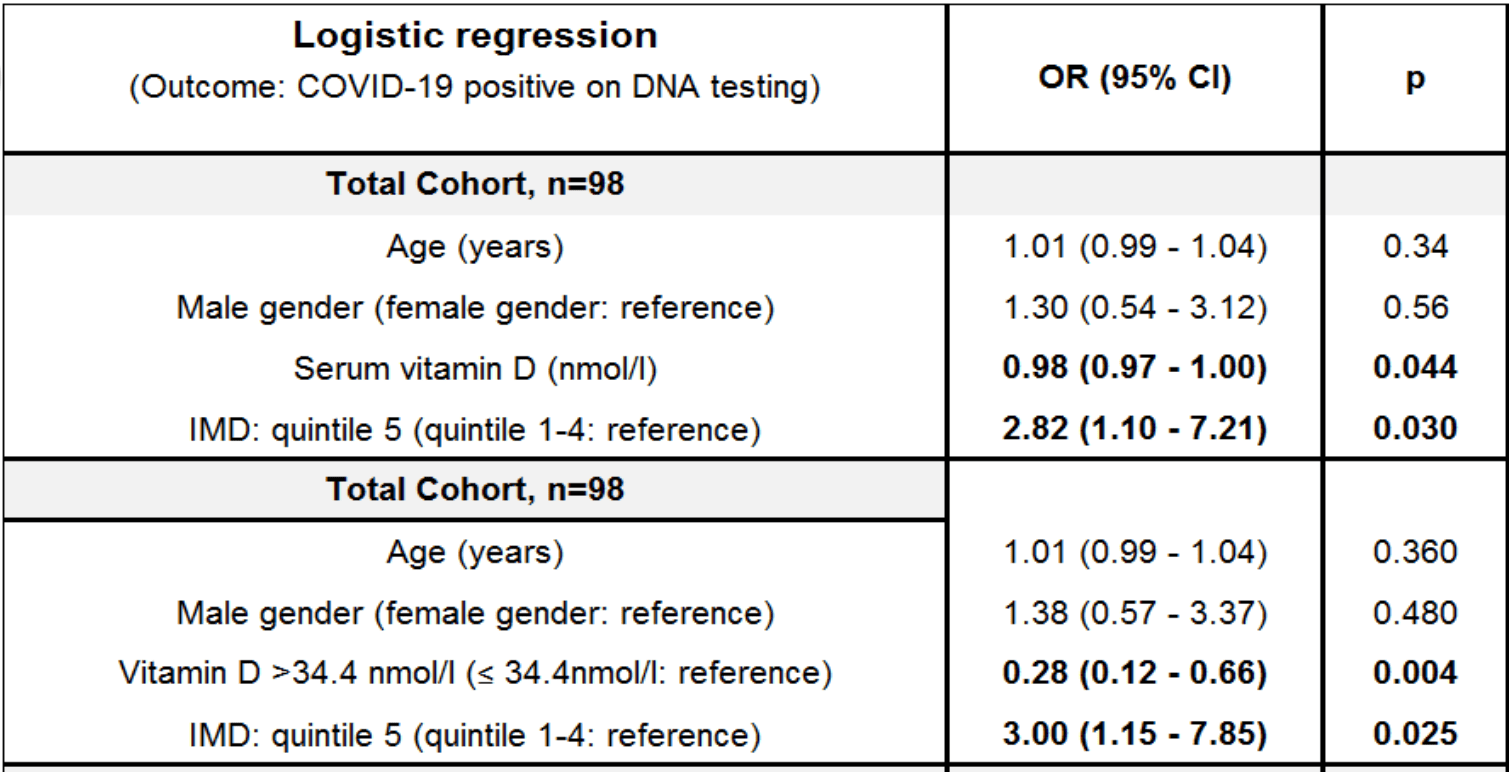 risk of case, 50.9% lower, RR 0.49, p = 0.02, high D levels 16 of 52 (30.8%), low D levels 31 of 52 (59.6%), OR converted to RR, >34.4nmol/L. Livingston et al., 4/2/2021, retrospective, United Kingdom, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Levels | Bayramoğlu et al., European Journal of Pediatrics, doi:10.1007/s00431-021-04030-1 (Peer Reviewed) | severe case, ↓69.5%, p=0.03 | The association between vitamin D levels and the clinical severity and inflammation markers in pediatric COVID-19 patients: single-center experience from a pandemic hospital |
| Details Retrospective 103 pediatric hospitalized COVID-19 patients, showing an association between vitamin D deficiency and clinical severity. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Bayramoğlu et al., European Journal of Pediatrics, doi:10.1007/s00431-021-04030-1 (Peer Reviewed) |
| The association between vitamin D levels and the clinical severity and inflammation markers in pediatric COVID-19 patients: single-center experience from a pandemic hospital |
Retrospective 103 pediatric hospitalized COVID-19 patients, showing an association between vitamin D deficiency and clinical severity. 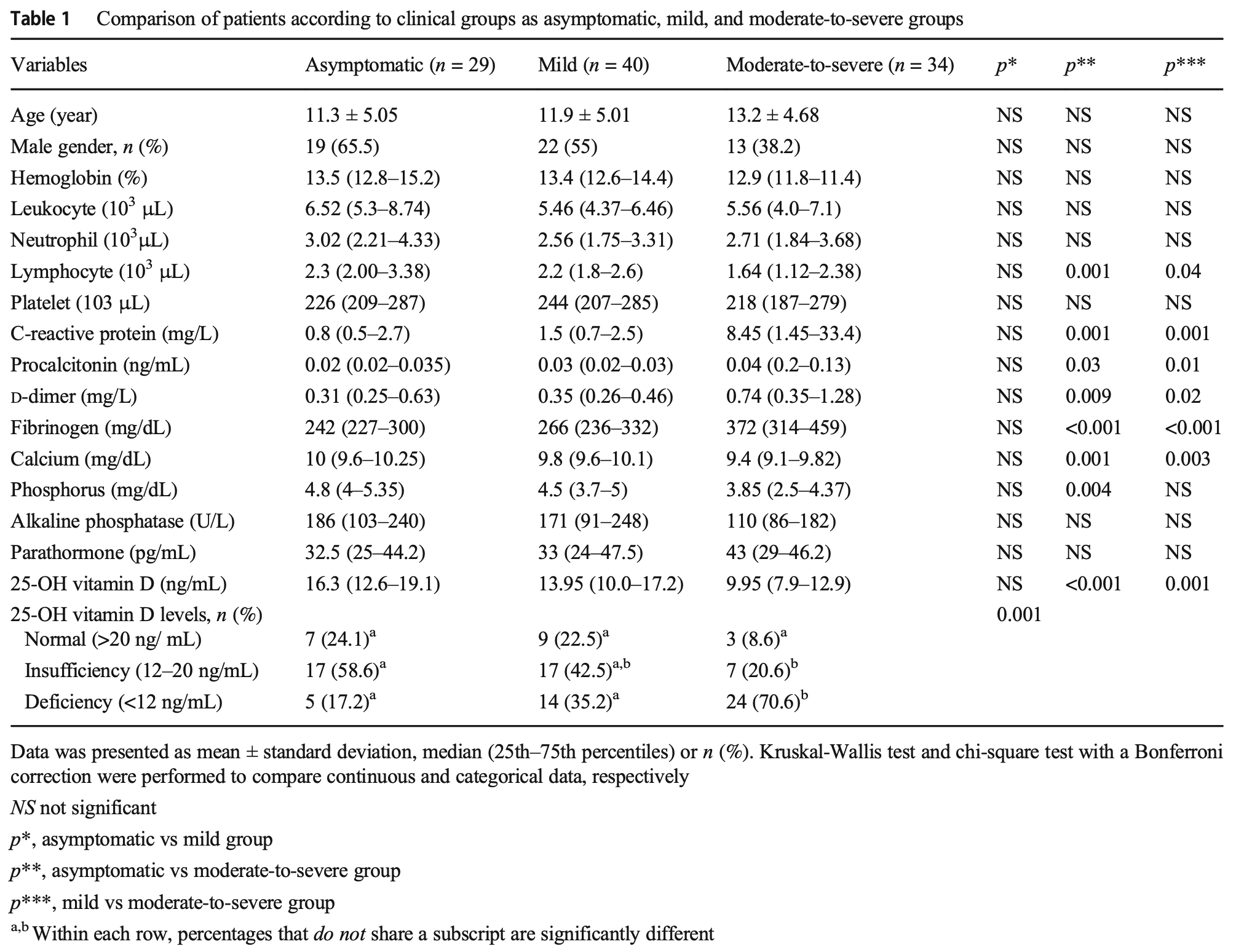 risk of moderate/severe case, 69.5% lower, RR 0.30, p = 0.03, high D levels 10 of 60 (16.7%), low D levels 24 of 43 (55.8%), adjusted, OR converted to RR, >12 ng/mL, multivariate logistic regression. Bayramoğlu et al., 3/31/2021, retrospective, Turkey, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Holt et al., medRxiv, doi:10.1101/2021.03.27.21254452 (Preprint) | cases, ↓6.8%, p=0.53 | Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK) |
| Details Prospective survey-based study with 15,227 people in the UK, showing lower risk of COVID-19 cases with vitamin A, vitamin D, zinc, selenium, probiotics, and inhaled corticosteroids; and higher risk with metformin and vitamin C. Statistica.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Holt et al., medRxiv, doi:10.1101/2021.03.27.21254452 (Preprint) |
| Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK) |
Prospective survey-based study with 15,227 people in the UK, showing lower risk of COVID-19 cases with vitamin A, vitamin D, zinc, selenium, probiotics, and inhaled corticosteroids; and higher risk with metformin and vitamin C. Statistical significance was not reached for any of these. Results are subject to confounding, with only the vitamin D result fully adjusted. NCT04330599. COVIDENCE UK. 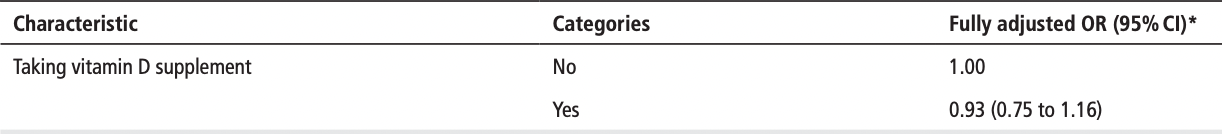 risk of case, 6.8% lower, RR 0.93, p = 0.53, treatment 141 of 5,640 (2.5%), control 305 of 9,587 (3.2%), adjusted, OR converted to RR, fully adjusted, group sizes approximated. Excluded in after exclusion results of meta analysis: significant unadjusted confounding possible. Holt et al., 3/30/2021, prospective, United Kingdom, Europe, preprint, 31 authors, dosage not specified. |
| Submit Corrections or Comments |
| Meta | Akbar et al., Front. Nutr. 8:660420, doi:10.3389/fnut.2021.660420 (Peer Reviewed) (meta analysis) | meta-analysis | Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated With Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis |
| Details Systematic review and meta analysis showing that low vitamin D levels was associated with COVID-19 cases, severity, and mortality. |
| Details Source PDF Meta Meta |
| Akbar et al., Front. Nutr. 8:660420, doi:10.3389/fnut.2021.660420 (Peer Reviewed) (meta analysis) |
| Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated With Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis |
Systematic review and meta analysis showing that low vitamin D levels was associated with COVID-19 cases, severity, and mortality. 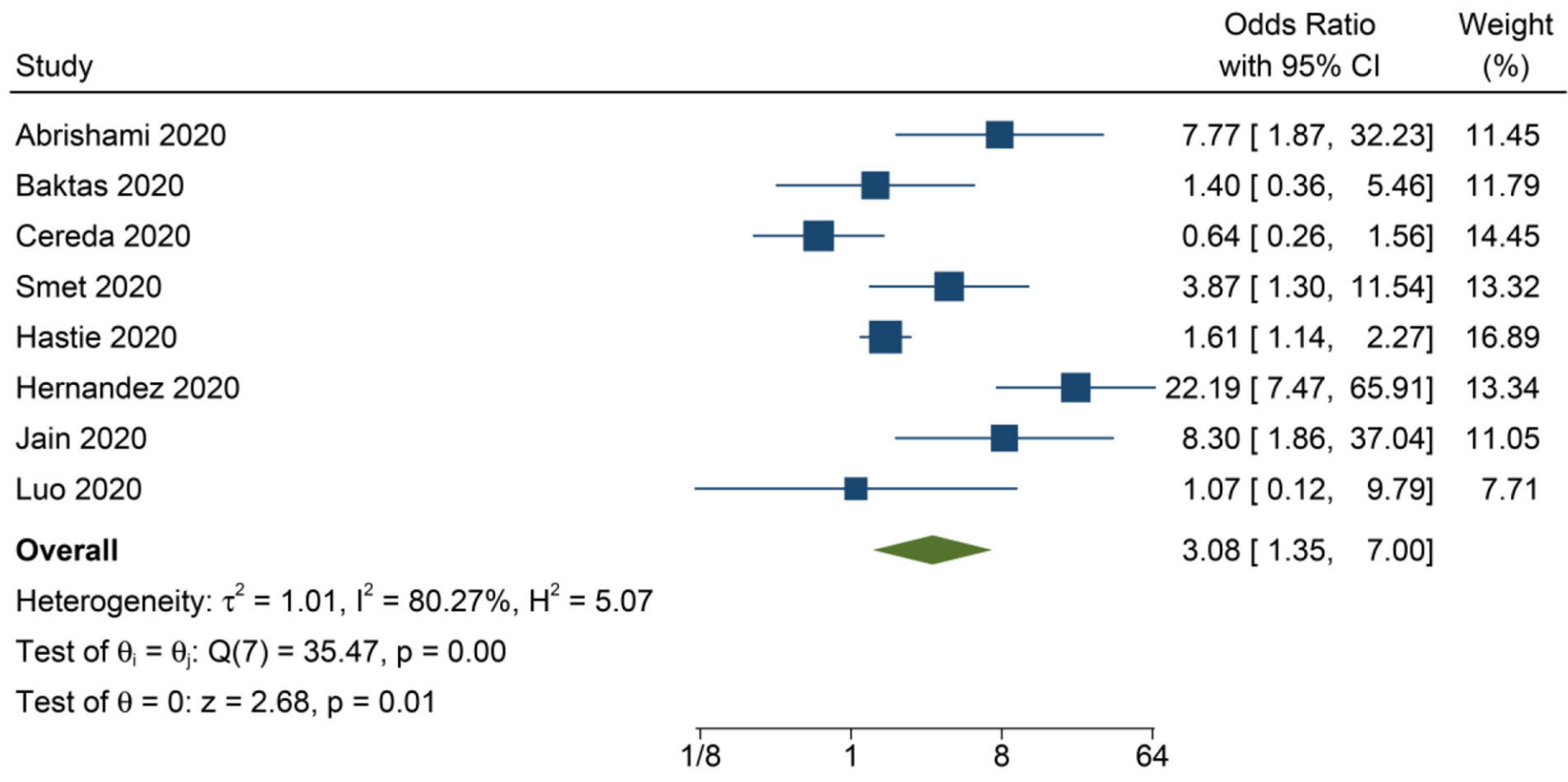 Akbar et al., 3/29/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Gaudio et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph18073491 (Peer Reviewed) | cases, ↓79.3%, p<0.0001 | Vitamin D Levels Are Reduced at the Time of Hospital Admission in Sicilian SARS-CoV-2-Positive Patients |
| Details Retrospective 50 COVID-19 hospitalized patients in Italy with vitamin D levels measured on admission, and 100 matched control patients, showing significantly lower vitamin D levels in COVID-19 patients. Vitamin D levels were also lower in.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Gaudio et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph18073491 (Peer Reviewed) |
| Vitamin D Levels Are Reduced at the Time of Hospital Admission in Sicilian SARS-CoV-2-Positive Patients |
Retrospective 50 COVID-19 hospitalized patients in Italy with vitamin D levels measured on admission, and 100 matched control patients, showing significantly lower vitamin D levels in COVID-19 patients. Vitamin D levels were also lower in COVID-19 patients with severe cases, without reaching statistical significance (p = 0.08, details not provided). 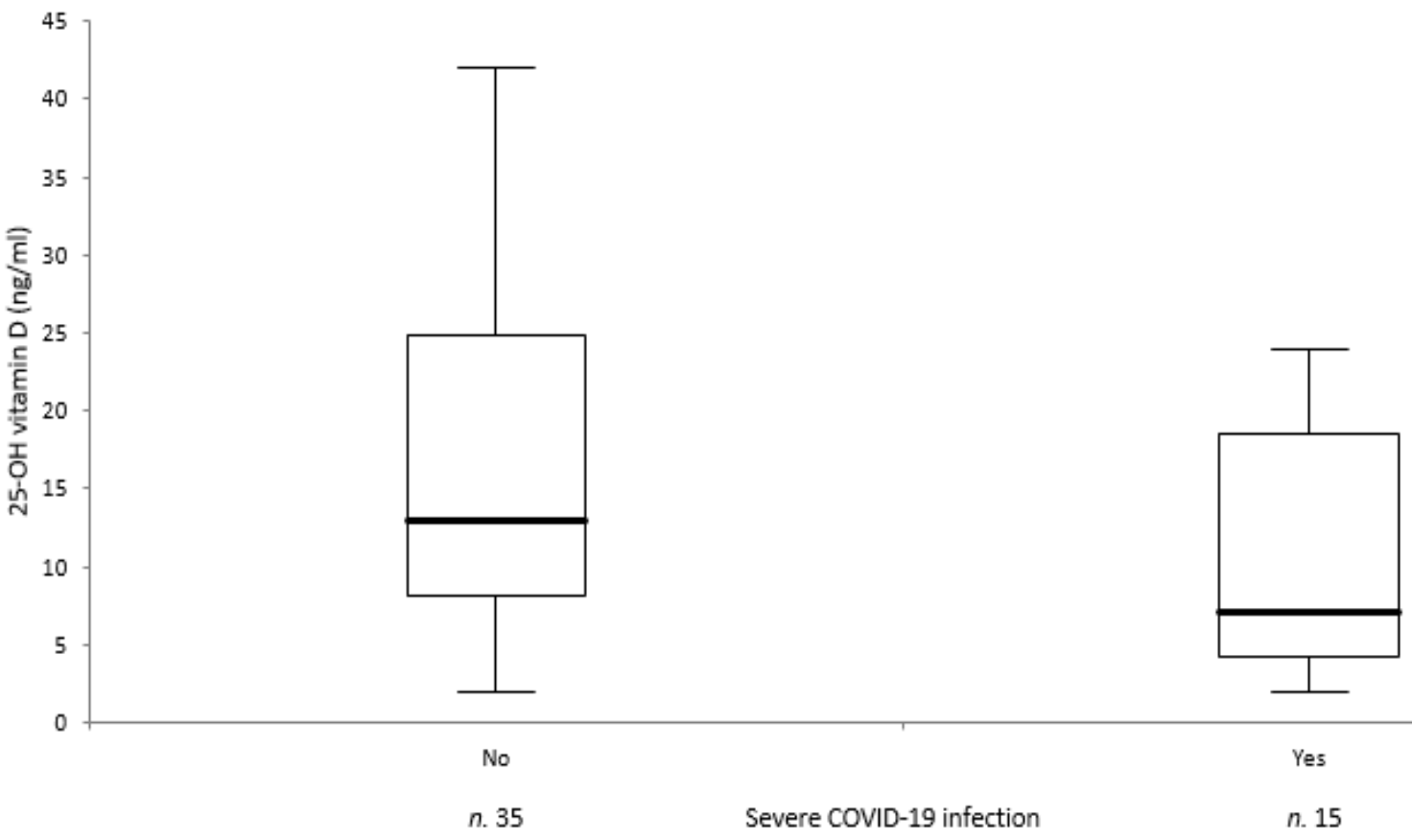 risk of case, 79.3% lower, RR 0.21, p < 0.001, high D levels 27 of 50 (54.0%) cases, 85 of 100 (85.0%) controls, case control OR. Gaudio et al., 3/27/2021, retrospective, Italy, Europe, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Freitas et al., medRxiv, doi:10.1101/2021.03.22.21254032 (Preprint) | death, ↓41.2%, p=0.02 | Vitamin D-related polymorphisms and vitamin D levels as risk biomarkers of COVID-19 infection severity |
| Details Analysis of 491 hospitalized patients in Portugal showing that polymorphisms in the vitamin D binding protein encoded by the GC gene are related to COVID-19 severity (p = 0.005). There was an association between vitamin D polygenic risk s.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Freitas et al., medRxiv, doi:10.1101/2021.03.22.21254032 (Preprint) |
| Vitamin D-related polymorphisms and vitamin D levels as risk biomarkers of COVID-19 infection severity |
Analysis of 491 hospitalized patients in Portugal showing that polymorphisms in the vitamin D binding protein encoded by the GC gene are related to COVID-19 severity (p = 0.005). There was an association between vitamin D polygenic risk score and vitamin D levels (p = 0.042), and between vitamin D levels and mortality (p = 1.5e-4). Authors conclude that a genetic susceptibility for vitamin D deficiency may explain higher severity in COVID-19.  risk of death, 41.2% lower, RR 0.59, p = 0.02, high D levels 23 of 179 (12.8%), low D levels 68 of 311 (21.9%), >20ng/mL. Freitas et al., 3/27/2021, retrospective, Portugal, Europe, preprint, 36 authors. |
| Submit Corrections or Comments |
| Meta | Petrelli et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883 (Peer Reviewed) (meta analysis) | meta-analysis | Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies |
| Details Meta analysis showing vitamin D deficiency associated with higher risk of COVID-19, worse severity, and higher mortality. Supplementation with vitamin D reduced the risk of severe cases and mortality. |
| Details Source PDF Meta Meta |
| Petrelli et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883 (Peer Reviewed) (meta analysis) |
| Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies |
Meta analysis showing vitamin D deficiency associated with higher risk of COVID-19, worse severity, and higher mortality.Supplementation with vitamin D reduced the risk of severe cases and mortality. 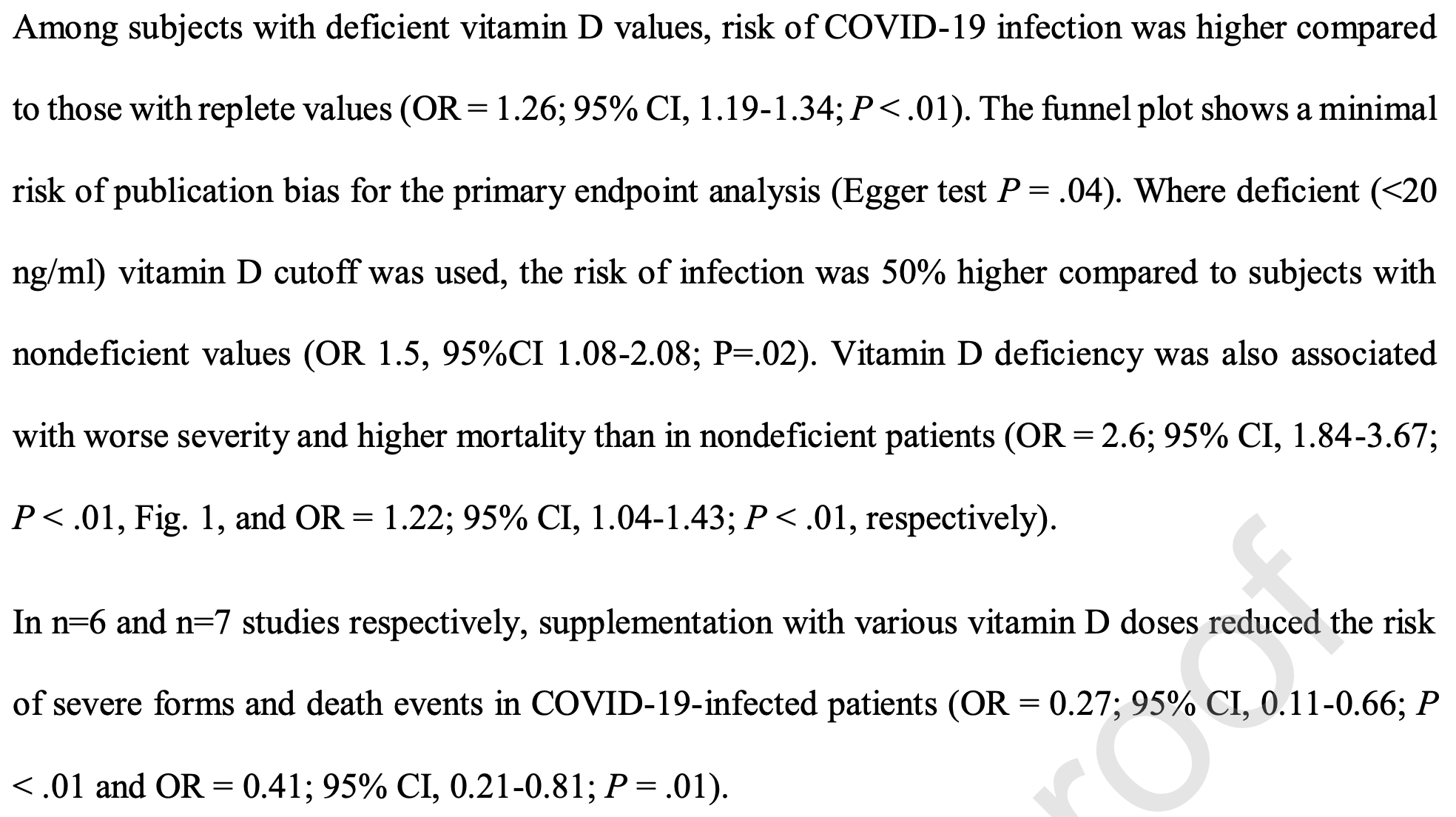 Petrelli et al., 3/26/2021, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Review | Kohlmeier et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265 (Review) (Peer Reviewed) | review | When Mendelian randomisation fails |
| Details Analysis of why Mendelian randomization may fail in vitamin D studies. Authors suggest that it may come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune respo.. |
| Details Source PDF Review Review |
| Kohlmeier et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265 (Review) (Peer Reviewed) |
| When Mendelian randomisation fails |
Analysis of why Mendelian randomization may fail in vitamin D studies. Authors suggest that it may come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response. For most other purposes, it may not matter much that unbound (free) 25-OHD is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25-OHD and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all.
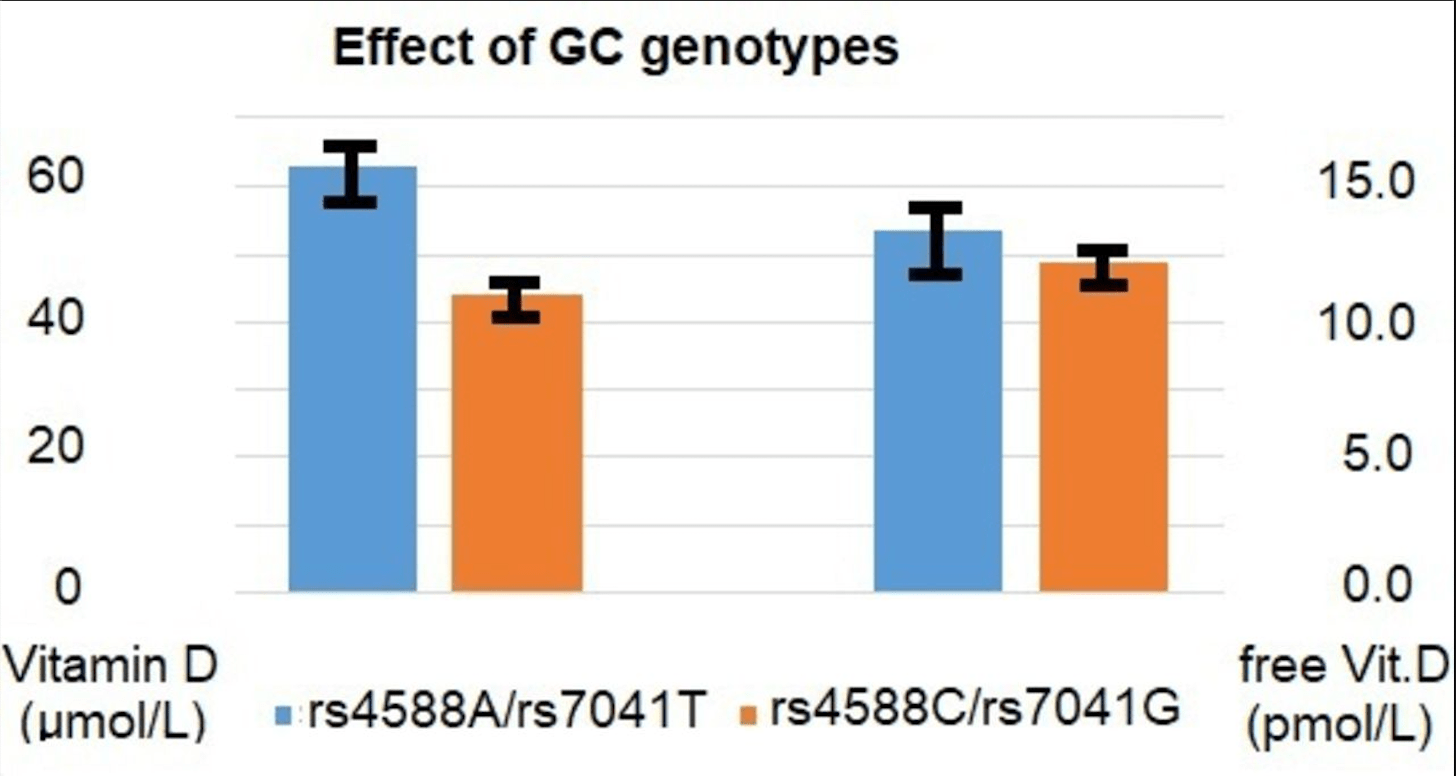 Kohlmeier et al., 3/22/2021, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| Levels | Meltzer et al., JAMA Netw Open., doi:10.1001/jamanetworkopen.2021.4117 (Peer Reviewed) | cases, ↓34.6%, p=0.11 | Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results |
| Details Retrospective 4,638 individuals with vitamin D levels within 1 year before COVID-19 testing, showing higher risk of COVID-19 PCR+ for vitamin D deficient individuals, and lower (but not statistically significant) cases for individuals usi.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Meltzer et al., JAMA Netw Open., doi:10.1001/jamanetworkopen.2021.4117 (Peer Reviewed) |
| Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results |
Retrospective 4,638 individuals with vitamin D levels within 1 year before COVID-19 testing, showing higher risk of COVID-19 PCR+ for vitamin D deficient individuals, and lower (but not statistically significant) cases for individuals using vitamin D supplementation. 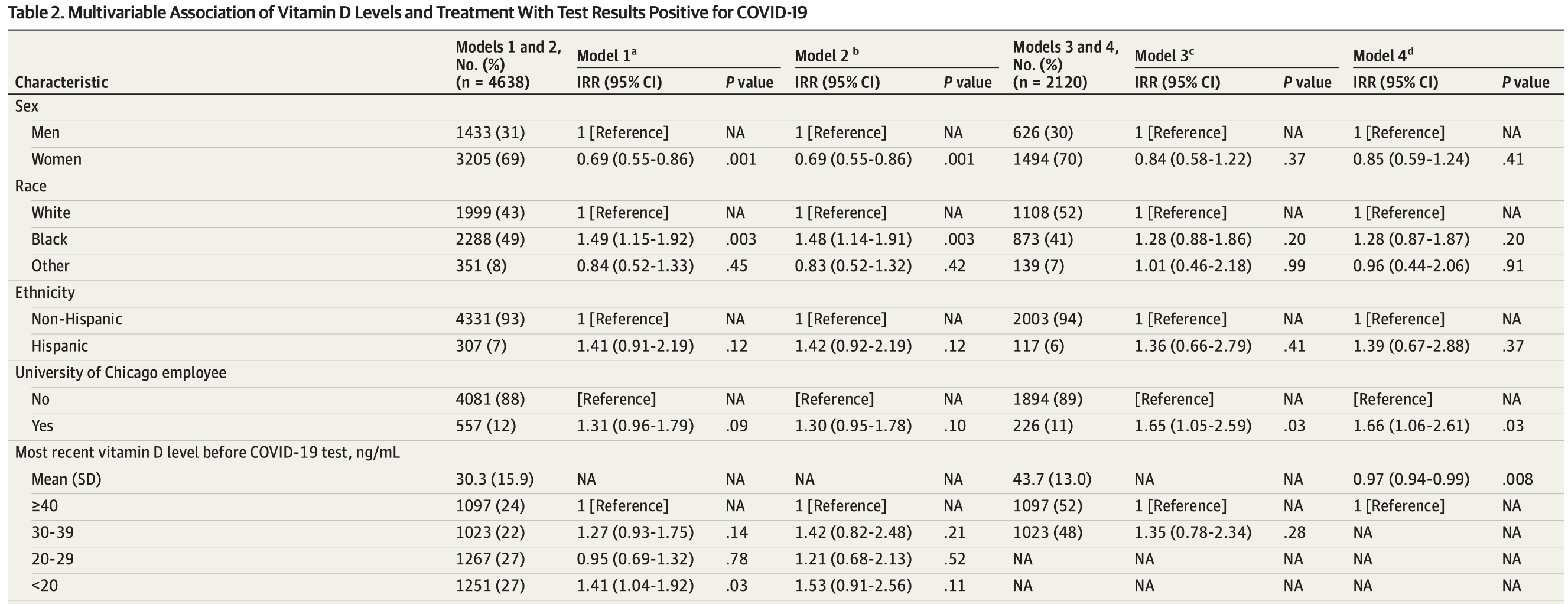 risk of case, 34.6% lower, RR 0.65, p = 0.11, high D levels 61 of 1,097 (5.6%), low D levels 118 of 1,251 (9.4%), adjusted, >40ng/mL vs. <20ng/mL, Table 2, Model 2. risk of case, 36.0% lower, RR 0.64, p = 0.38, high D levels 6 of 131 (4.6%), low D levels 239 of 3,338 (7.2%), supplementation, >=2,000IU/d. risk of case, 31.1% lower, RR 0.69, p = 0.16, high D levels 15 of 304 (4.9%), low D levels 239 of 3,338 (7.2%), supplementation, >=1,001IU/d. risk of case, 8.9% lower, RR 0.91, p = 0.56, high D levels 60 of 920 (6.5%), low D levels 239 of 3,338 (7.2%), supplementation, >=1IU/d. Meltzer et al., 3/19/2021, retrospective, database analysis, USA, North America, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Vanegas-Cedillo, medRxiv, doi:10.1101/2021.03.12.21253490 (Preprint) | death, ↓52.6%, p=0.006 | Serum Vitamin D levels are associated with increased COVID-19 severity markers and mortality independent of visceral adiposity |
| Details Retrospective 551 moderate to severe COVID-19 patients in Mexico showing vitamin D ≤12ng/mL independently associated with COVID-19 mortality. No association was found between vitamin D levels and the need for intubation. Vitamin D deficie.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Vanegas-Cedillo, medRxiv, doi:10.1101/2021.03.12.21253490 (Preprint) |
| Serum Vitamin D levels are associated with increased COVID-19 severity markers and mortality independent of visceral adiposity |
Retrospective 551 moderate to severe COVID-19 patients in Mexico showing vitamin D ≤12ng/mL independently associated with COVID-19 mortality. No association was found between vitamin D levels and the need for intubation. Vitamin D deficiency was more prevalent in women and patients with type 2 diabetes. 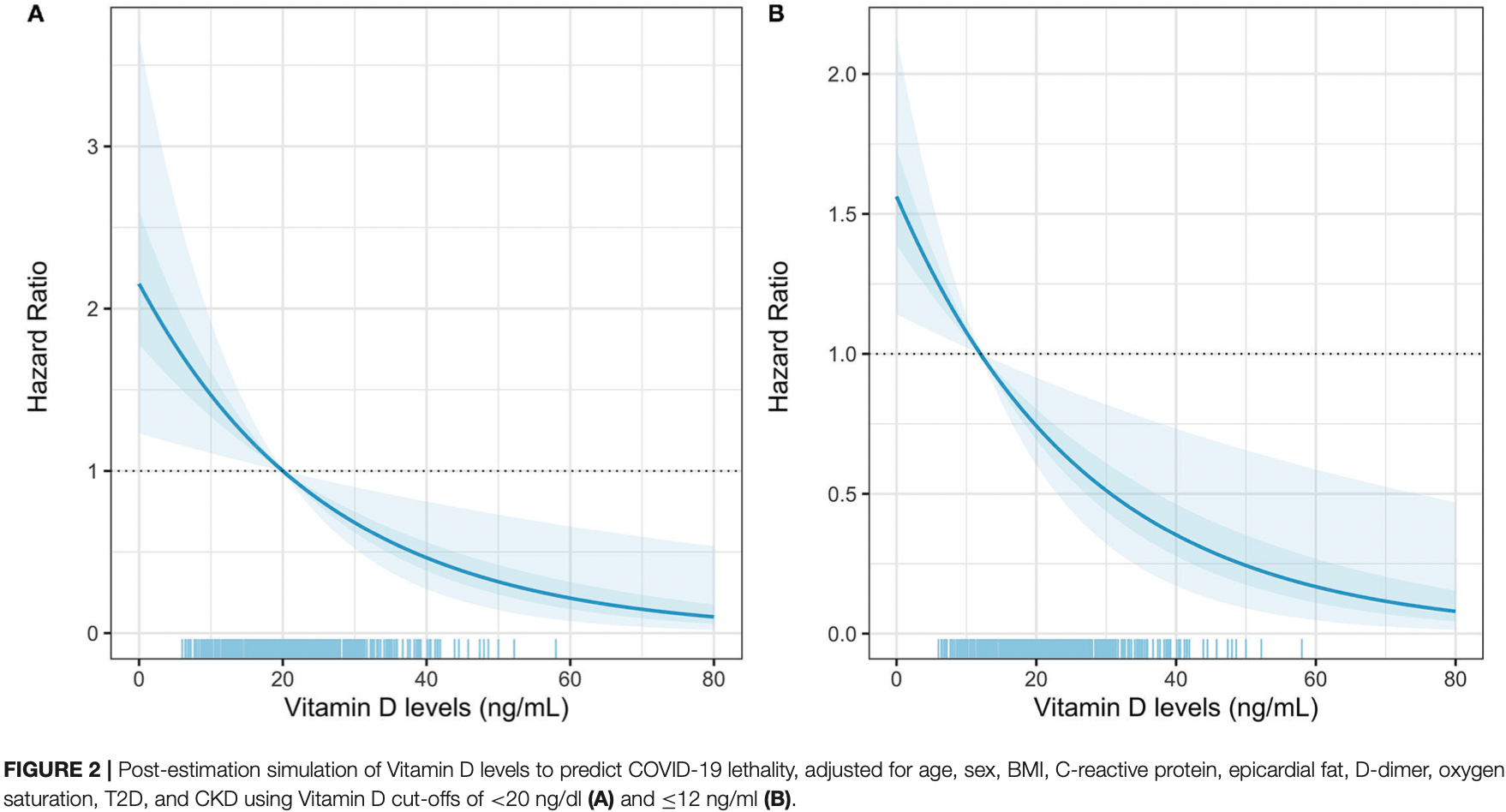 risk of death, 52.6% lower, RR 0.47, p = 0.006, high D levels 95 of 494 (19.2%), low D levels 21 of 57 (36.8%), adjusted, >12ng/mL. Vanegas-Cedillo et al., 3/14/2021, retrospective, Mexico, North America, preprint, 15 authors. |
| Submit Corrections or Comments |
| Levels | Jayawardena et al., Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2021.03.006 (Peer Reviewed) | Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries |
| Details Analysis of Asian countries finding that prevalence of vitamin D deficiency and lower vitamin D levels were associated with COVID-19 infection and mortality. Positive correlations were observed for prevalence of vitamin D deficiency with.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Jayawardena et al., Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2021.03.006 (Peer Reviewed) |
| Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries |
Analysis of Asian countries finding that prevalence of vitamin D deficiency and lower vitamin D levels were associated with COVID-19 infection and mortality.Positive correlations were observed for prevalence of vitamin D deficiency with COVID-19 infection (r = 0.76, p = 0.002) and mortality (r = 0.65, p = 0.03), after predicting with confounding factors. Mean vitamin D level had a significant negative correlation with COVID-19 infection (r = 0.77; p = 0.04) and mortality (r = 0.80, p = 0.03) when combining with confounders. 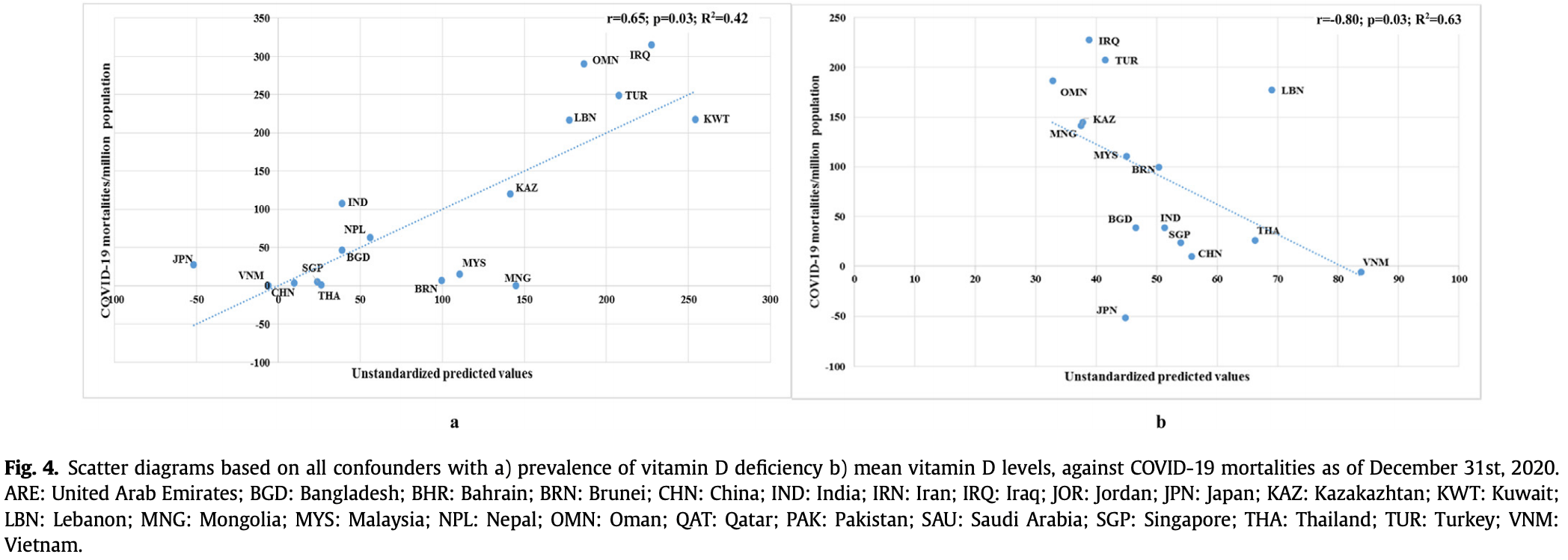 Jayawardena et al., 3/13/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Ahmad et al., medRxiv, doi:10.1101/2021.03.11.21253361 (Preprint) | death, ↓53.6%, p=0.03 | Mean Vitamin D levels in 19 European Countries & COVID-19 Mortality over 10 months |
| Details Retrospective 19 European countries showing countries with mean vitamin D levels > 50nmol/L have a 2.2 times lower risk of mortality (p = 0.032) compared to those with mean levels < 50 nmol/L. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ahmad et al., medRxiv, doi:10.1101/2021.03.11.21253361 (Preprint) |
| Mean Vitamin D levels in 19 European Countries & COVID-19 Mortality over 10 months |
Retrospective 19 European countries showing countries with mean vitamin D levels > 50nmol/L have a 2.2 times lower risk of mortality (p = 0.032) compared to those with mean levels < 50 nmol/L. 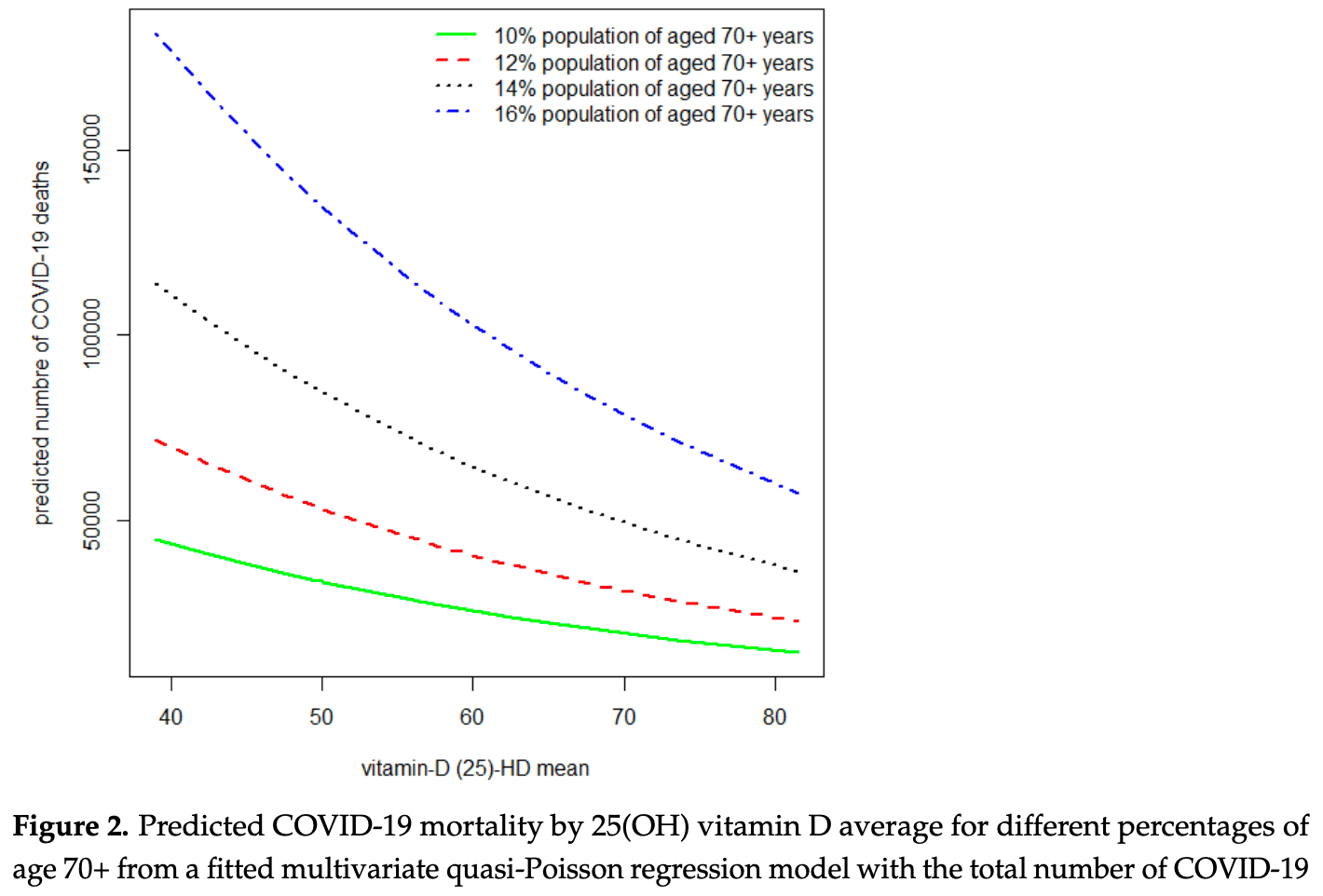 risk of death, 53.6% lower, RR 0.46, p = 0.03, >50nmol/L. Ahmad et al., 3/12/2021, preprint, 4 authors. |
| Submit Corrections or Comments |
| Levels | Charoenngam et al., Endocrine Practice, doi:10.1016/j.eprac.2021.02.013 (Peer Reviewed) | death, ↓34.1%, p=0.26 | Association of vitamin D status with hospital morbidity and mortality in adult hospitalized COVID-19 patients |
| Details Retrospective 287 hospitalized patients in the USA showing significantly lower mortality with vitamin D sufficiency in elderly patients and patients without obesity; and lower mortality for all patients but not reaching statistical signif.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Charoenngam et al., Endocrine Practice, doi:10.1016/j.eprac.2021.02.013 (Peer Reviewed) |
| Association of vitamin D status with hospital morbidity and mortality in adult hospitalized COVID-19 patients |
Retrospective 287 hospitalized patients in the USA showing significantly lower mortality with vitamin D sufficiency in elderly patients and patients without obesity; and lower mortality for all patients but not reaching statistical signifance. risk of death, 34.1% lower, RR 0.66, p = 0.26, high D levels 12 of 100 (12.0%), low D levels 29 of 187 (15.5%), adjusted, OR converted to RR, >=30ng/mL. risk of mechanical ventilation, 37.2% lower, RR 0.63, p = 0.17, high D levels 14 of 100 (14.0%), low D levels 34 of 187 (18.2%), adjusted, OR converted to RR, >=30ng/mL. risk of ICU admission, 23.1% lower, RR 0.77, p = 0.28, high D levels 25 of 100 (25.0%), low D levels 56 of 187 (29.9%), adjusted, OR converted to RR, >=30ng/mL. risk of death, 58.1% lower, RR 0.42, p = 0.05, high D levels 7 of 57 (12.3%), low D levels 25 of 79 (31.6%), adjusted, OR converted to RR, >65 years old, >=30ng/mL. Charoenngam et al., 3/8/2021, retrospective, USA, North America, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Late | Notz et al., Clinical Nutrition, doi:10.1016/j.clnu.2021.03.001 (Peer Reviewed) | Vitamin D deficiency in critically ill COVID-19 ARDS patients |
| Details Retrospective 26 ICU patients showing that the majority of patients had vitamin D deficiency. There was no statistically significant association of 25-hydroxyvitamin D status and clinical course, however low levels of 1,25-dihydroxyvitami.. |
| Details Source PDF Late treatment study Late treatment study |
| Notz et al., Clinical Nutrition, doi:10.1016/j.clnu.2021.03.001 (Peer Reviewed) |
| Vitamin D deficiency in critically ill COVID-19 ARDS patients |
Retrospective 26 ICU patients showing that the majority of patients had vitamin D deficiency. There was no statistically significant association of 25-hydroxyvitamin D status and clinical course, however low levels of 1,25-dihydroxyvitamin D were associated with prolonged mechanical ventilation and a worse APACHE II score. Clinical outcomes based on baseline vitamin D status are not provided. 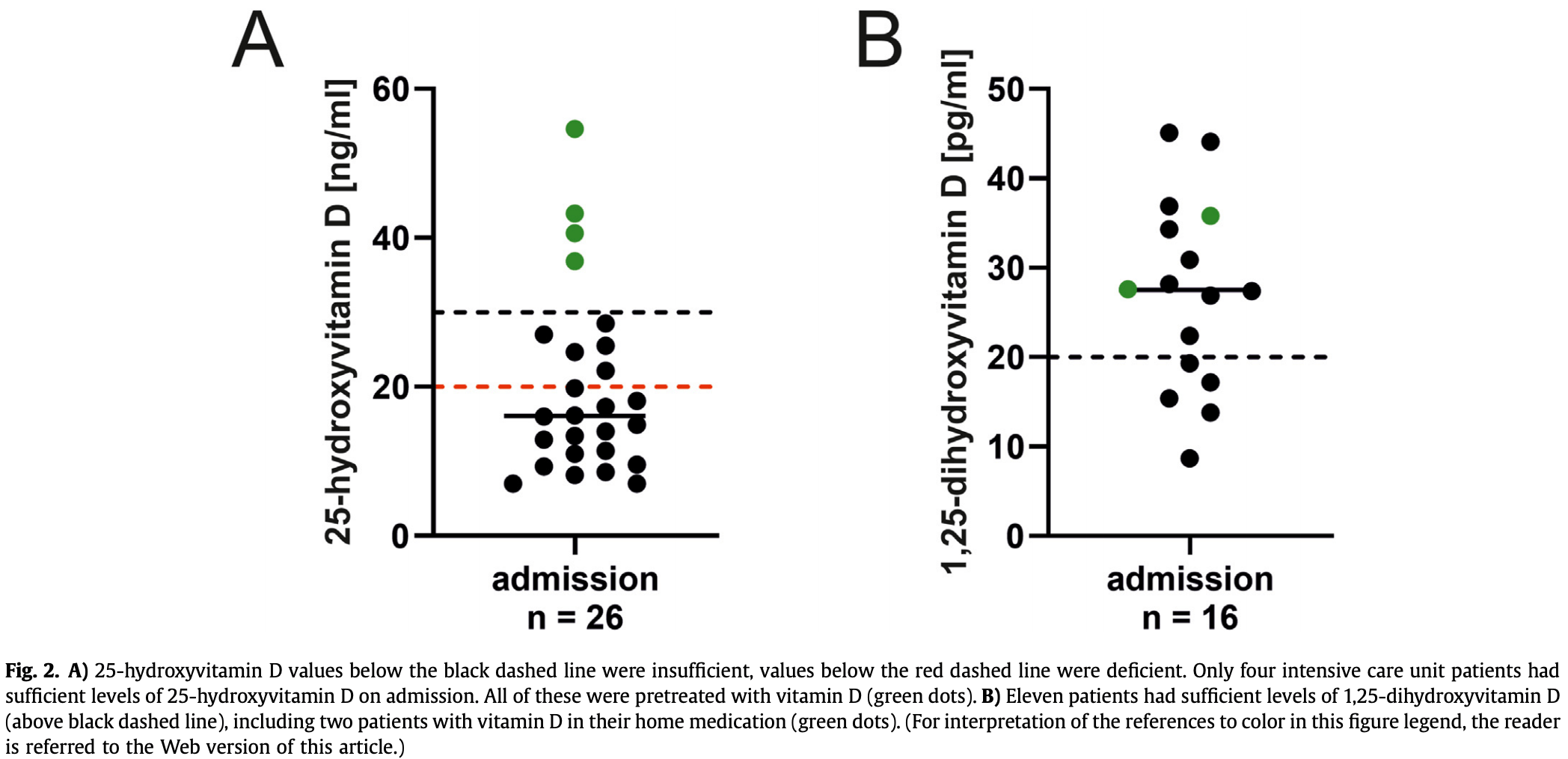 Notz et al., 3/7/2021, peer-reviewed, 12 authors. |
| Submit Corrections or Comments |
| Levels | Kralj et al., Critical Case Reports, doi:10.1002/ccr3.4010 (Peer Reviewed) | Vitamin D and COVID‐19 in an immunocompromised patient with multiple comorbidities—A Case Report |
| Details Case report of a high-risk immunocompromised patient with multiple comorbidities that had a mild case of COVID-19. The patient had UVB phototherapy three months earlier and had normal vitamin D levels (92.2 nmol/L, normal range 50-125). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Kralj et al., Critical Case Reports, doi:10.1002/ccr3.4010 (Peer Reviewed) |
| Vitamin D and COVID‐19 in an immunocompromised patient with multiple comorbidities—A Case Report |
Case report of a high-risk immunocompromised patient with multiple comorbidities that had a mild case of COVID-19. The patient had UVB phototherapy three months earlier and had normal vitamin D levels (92.2 nmol/L, normal range 50-125). 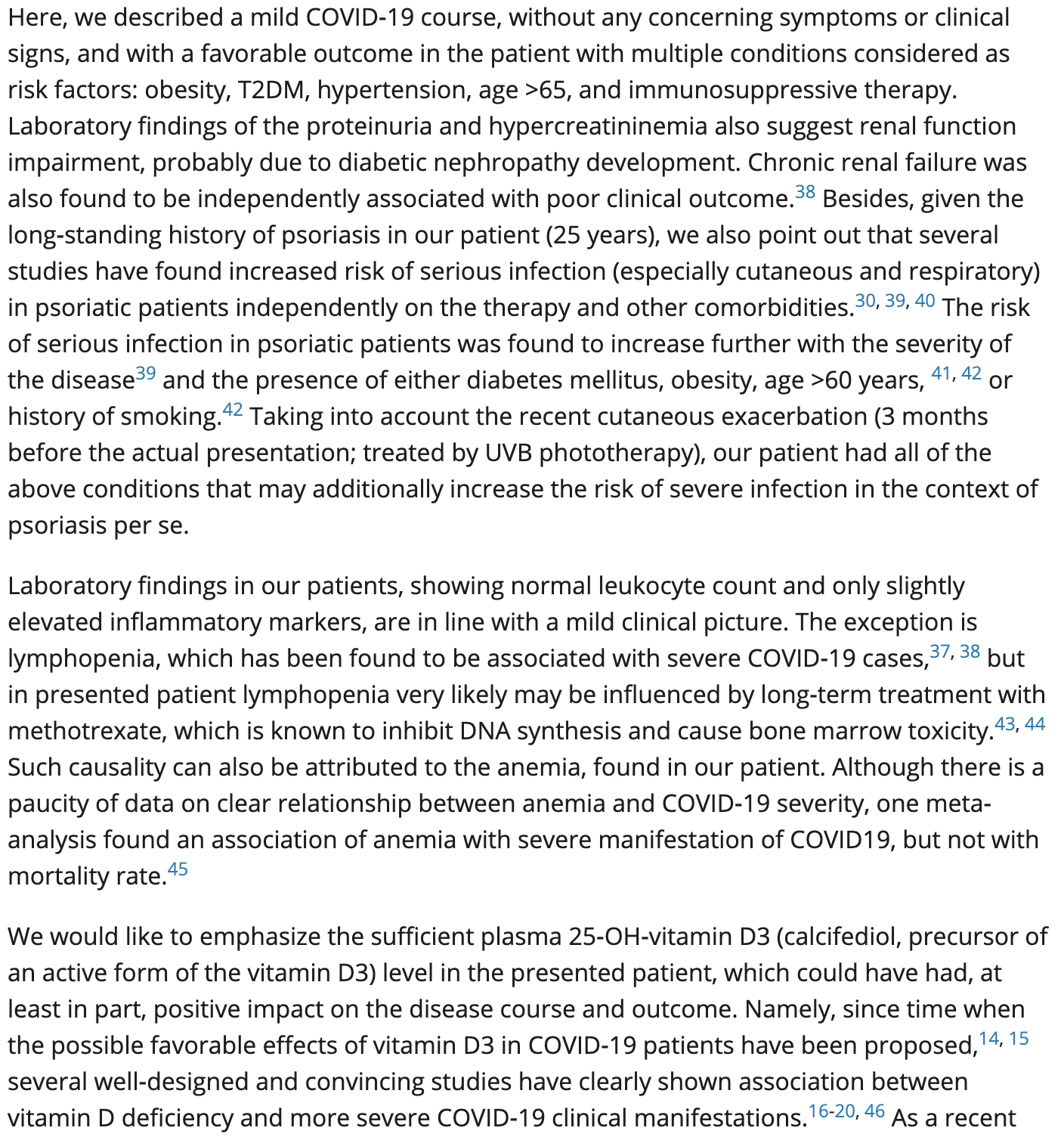 Kralj et al., 3/5/2021, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Mazziotti et al., J Endocrinol. Invest., doi:10.1007/s40618-021-01535-2 (Peer Reviewed) | death, ↓19.0%, p=0.49 | Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19 |
| Details - |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Mazziotti et al., J Endocrinol. Invest., doi:10.1007/s40618-021-01535-2 (Peer Reviewed) |
| Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19 |
- risk of death, 19.0% lower, RR 0.81, p = 0.49, treatment 116, control 232, RR approximated with OR. risk of mechanical ventilation, 67.0% higher, RR 1.67, p = 0.08, treatment 116, control 232, RR approximated with OR. Mazziotti et al., 3/5/2021, retrospective, Italy, Europe, peer-reviewed, 11 authors, dosage varies. |
| Submit Corrections or Comments |
| Levels | Mazziotti et al., J Endocrinol. Invest., doi:10.1007/s40618-021-01535-2 (Peer Reviewed) | death, ↓2.4%, p=0.91 | Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19 |
| Details Retrospective 348 hospitalized patients in Italy showing vitamin D deficiency associated with acute hypoxemic respiratory failure. Vitamin D supplementation during hospitalization was not significantly associated with mortality or ventila.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Mazziotti et al., J Endocrinol. Invest., doi:10.1007/s40618-021-01535-2 (Peer Reviewed) |
| Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19 |
Retrospective 348 hospitalized patients in Italy showing vitamin D deficiency associated with acute hypoxemic respiratory failure. Vitamin D supplementation during hospitalization was not significantly associated with mortality or ventilation. risk of acute hypoxemic respiratory failure, 2.4% lower, RR 0.98, p = 0.91, high D levels 187, low D levels 161, OR converted to RR, >12ng/mL, control prevalance approximated with overall prevalence. risk of acute hypoxemic respiratory failure, 37.0% lower, RR 0.63, p = 0.006, high D levels 72 of 187 (38.5%), low D levels 97 of 161 (60.2%), OR converted to RR, >12ng/mL. Mazziotti et al., 3/5/2021, retrospective, Italy, Europe, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Lohia et al., American Journal of Physiology-Endocrinology and Metabolism, doi:10.1152/ajpendo.00517.2020 (Peer Reviewed) | death, ↓14.7%, p=0.56 | Exploring the link between vitamin D and clinical outcomes in COVID-19 |
| Details Retrospective 270 patients with vitamin D levels measured in the last year, showing no significant difference in outcomes based on vitamin D levels or vitamin D supplementation. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Lohia et al., American Journal of Physiology-Endocrinology and Metabolism, doi:10.1152/ajpendo.00517.2020 (Peer Reviewed) |
| Exploring the link between vitamin D and clinical outcomes in COVID-19 |
Retrospective 270 patients with vitamin D levels measured in the last year, showing no significant difference in outcomes based on vitamin D levels or vitamin D supplementation. 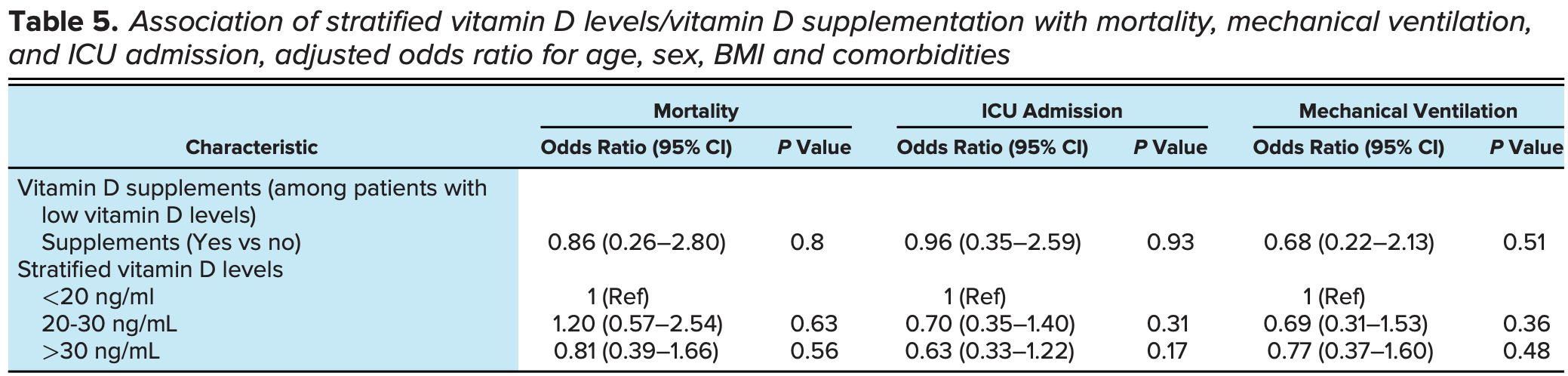 risk of death, 14.7% lower, RR 0.85, p = 0.56, high D levels 88, low D levels 95, OR converted to RR, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated. risk of mechanical ventilation, 18.9% lower, RR 0.81, p = 0.48, high D levels 88, low D levels 95, OR converted to RR, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated. risk of ICU admission, 28.5% lower, RR 0.72, p = 0.17, high D levels 88, low D levels 95, OR converted to RR, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated. Lohia et al., 3/4/2021, retrospective, USA, North America, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Ricci et al., Respiratory Research, doi:10.1186/s12931-021-01666-3 (Peer Reviewed) | death, ↓87.6%, p=0.07 | Circulating Vitamin D levels status and clinical prognostic indices in COVID-19 patients |
| Details Retrospective 52 hospitalized COVID-19 patients showing that vitamin D deficiency is associated with compromised inflammatory responses and higher pulmonary involvement. Vitamin D deficient patients also showed higher mortality, although .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ricci et al., Respiratory Research, doi:10.1186/s12931-021-01666-3 (Peer Reviewed) |
| Circulating Vitamin D levels status and clinical prognostic indices in COVID-19 patients |
Retrospective 52 hospitalized COVID-19 patients showing that vitamin D deficiency is associated with compromised inflammatory responses and higher pulmonary involvement. Vitamin D deficient patients also showed higher mortality, although not quite reaching statistical significance with the small sample size. 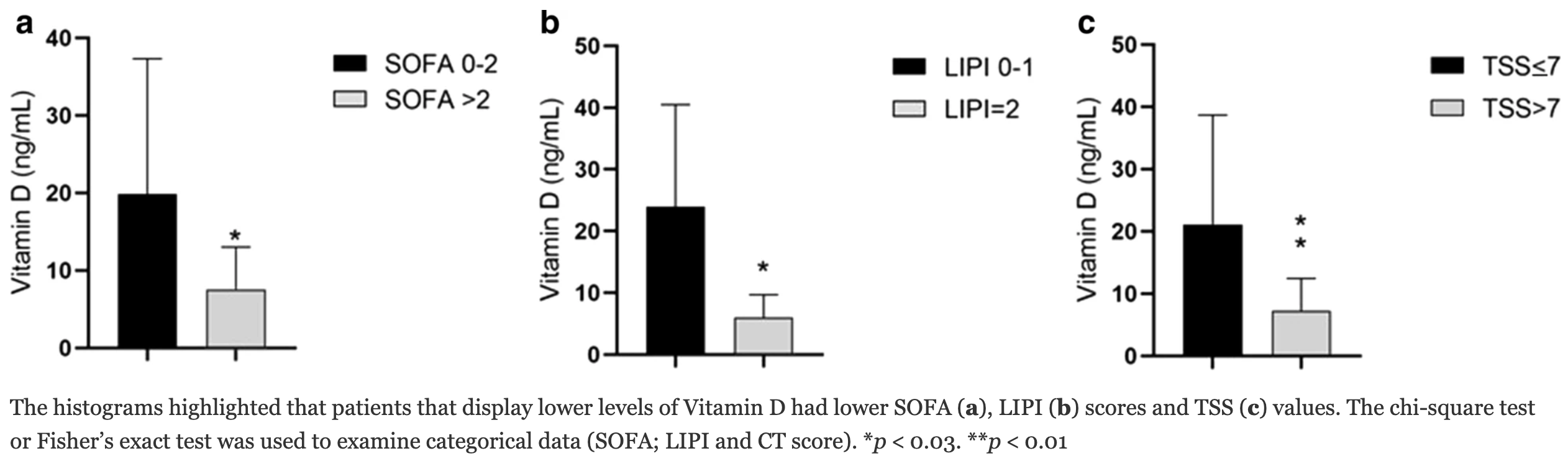 risk of death, 87.6% lower, RR 0.12, p = 0.07, high D levels 0 of 30 (0.0%), low D levels 3 of 22 (13.6%), relative risk is not 0 because of continuity correction due to zero events, >10 ng/mL. Ricci et al., 3/3/2021, retrospective, Italy, Europe, peer-reviewed, 15 authors. |
| Submit Corrections or Comments |
| Late | Karen et al., International Journal of Progressive Science and Technologies, doi:10.52155/ijpsat.v27.2.3269 (Peer Reviewed) | Vitamin D Associated Peculiarities in Women with Mild Covid-19 and Effect of Calcifediol on the Level of Vitamin D and Possibly, on Disease Outcome - Prospective Pilot Study |
| Details Prospective study of 30 female COVID-19 patients, all treated with calcifediol on admission, showing significantly increased vitamin D levels with treatment. There was no mortality. |
| Details Source PDF Late treatment study Late treatment study |
| Karen et al., International Journal of Progressive Science and Technologies, doi:10.52155/ijpsat.v27.2.3269 (Peer Reviewed) |
| Vitamin D Associated Peculiarities in Women with Mild Covid-19 and Effect of Calcifediol on the Level of Vitamin D and Possibly, on Disease Outcome - Prospective Pilot Study |
Prospective study of 30 female COVID-19 patients, all treated with calcifediol on admission, showing significantly increased vitamin D levels with treatment. There was no mortality. 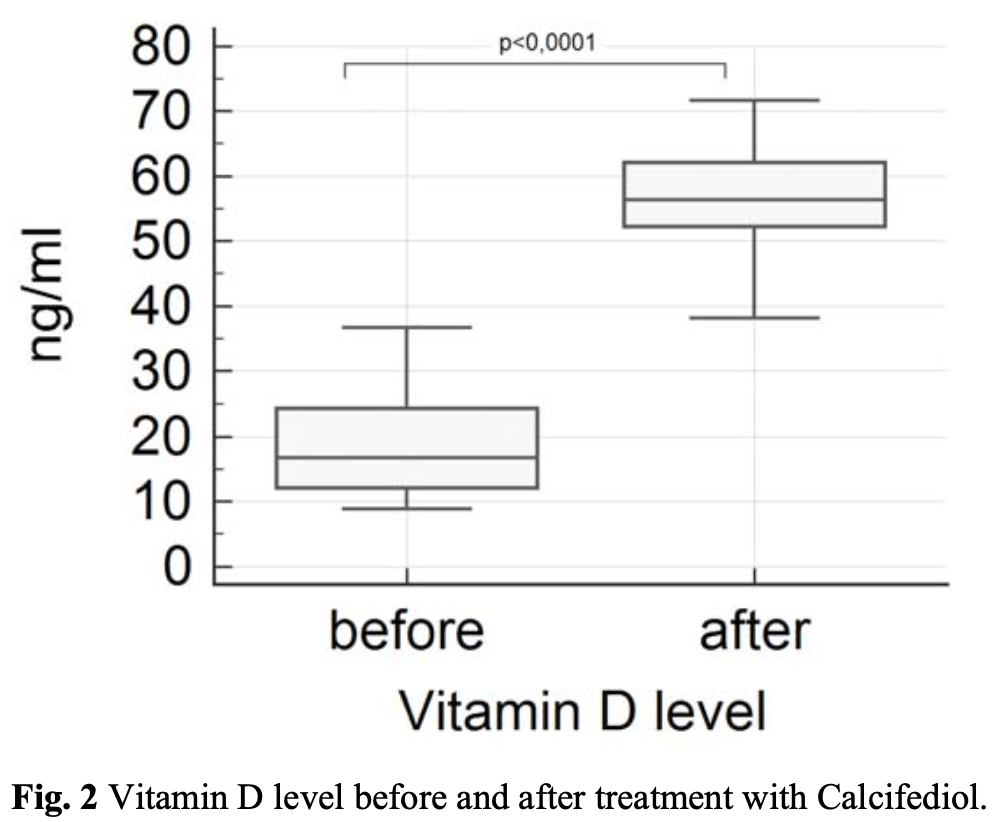 Karen et al., 2/28/2021, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Sulli et al., Nutrients, doi:10.3390/nu13030717 (Peer Reviewed) | cases, ↓75.6%, p=0.0002 | Vitamin D and Lung Outcomes in Elderly COVID-19 Patients |
| Details Retrospective 65 elderly COVID-19 patients and 65 matched controls, showing lower vitamin D levels associated with more severe lung involvement, longer disease duration, and higher mortality. Vitamin D supplementation was less common in t.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Sulli et al., Nutrients, doi:10.3390/nu13030717 (Peer Reviewed) |
| Vitamin D and Lung Outcomes in Elderly COVID-19 Patients |
Retrospective 65 elderly COVID-19 patients and 65 matched controls, showing lower vitamin D levels associated with more severe lung involvement, longer disease duration, and higher mortality. Vitamin D supplementation was less common in the COVID-19 group compared to the control group. 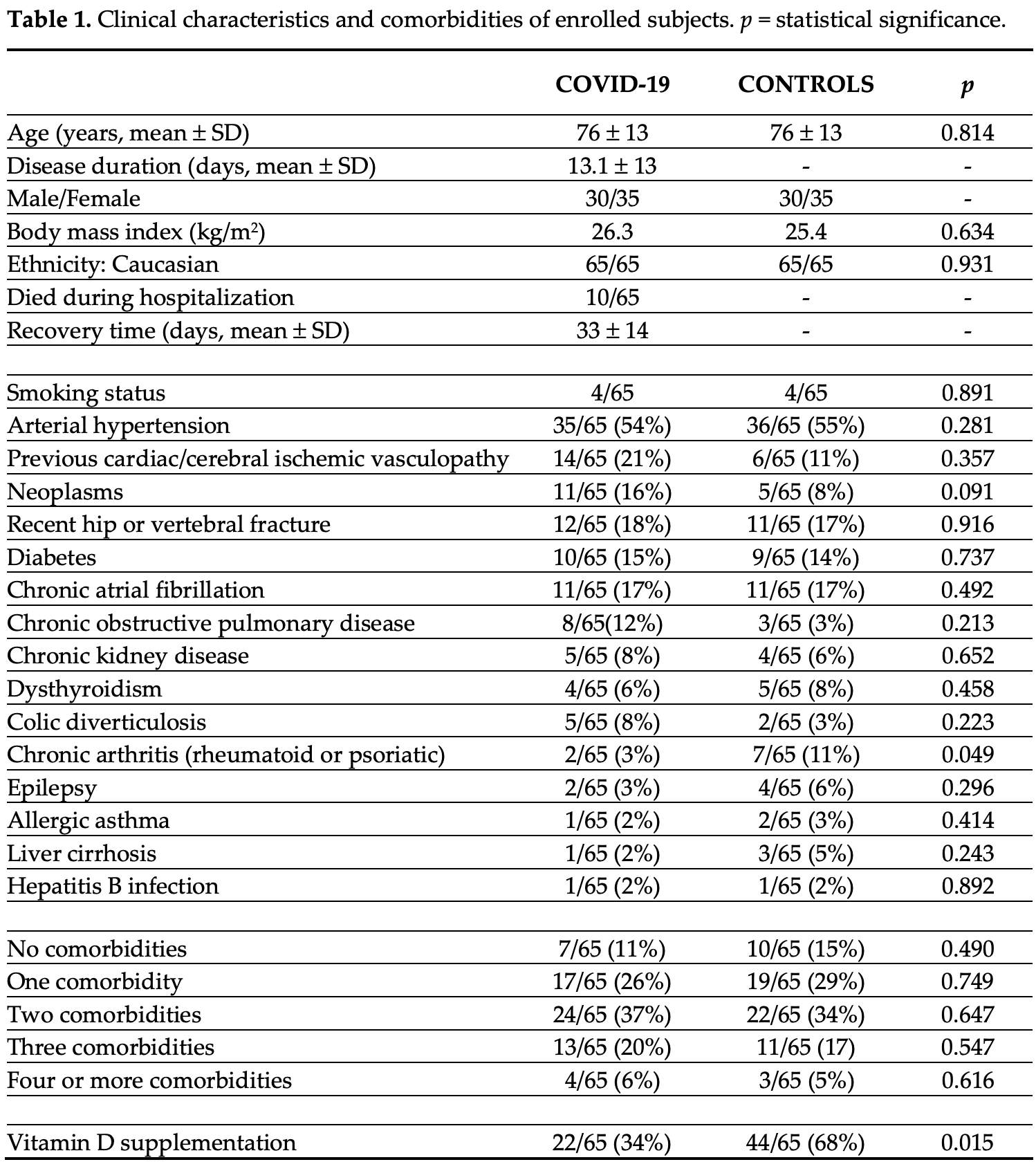 risk of case, 75.6% lower, RR 0.24, p < 0.001, treatment 22 of 65 (33.8%) cases, 44 of 65 (67.7%) controls, case control OR, vitamin D supplementation. Sulli et al., 2/24/2021, retrospective, Italy, Europe, peer-reviewed, 10 authors, dosage not specified. |
| Submit Corrections or Comments |
| Late | Lakkireddy et al., Scientific Reports, doi:10.1038/s41598-021-90189-4 (preprint 2/23/21) (Peer Reviewed) | death, ↓60.9%, p=0.27 | Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease |
| Details RCT 44 treatment and 43 control patients with vitamin D levels <30ng/ml, showing significant reduction in inflammatory markers with treatment of 60,000IU vitamin D per day for 8 days (10 days for BMI >25). Death and ICU admission was lowe.. |
| Details Source PDF Late treatment study Late treatment study |
| Lakkireddy et al., Scientific Reports, doi:10.1038/s41598-021-90189-4 (preprint 2/23/21) (Peer Reviewed) |
| Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease |
RCT 44 treatment and 43 control patients with vitamin D levels <30ng/ml, showing significant reduction in inflammatory markers with treatment of 60,000IU vitamin D per day for 8 days (10 days for BMI >25). Death and ICU admission was lower in the treatment group but not statistically significant. 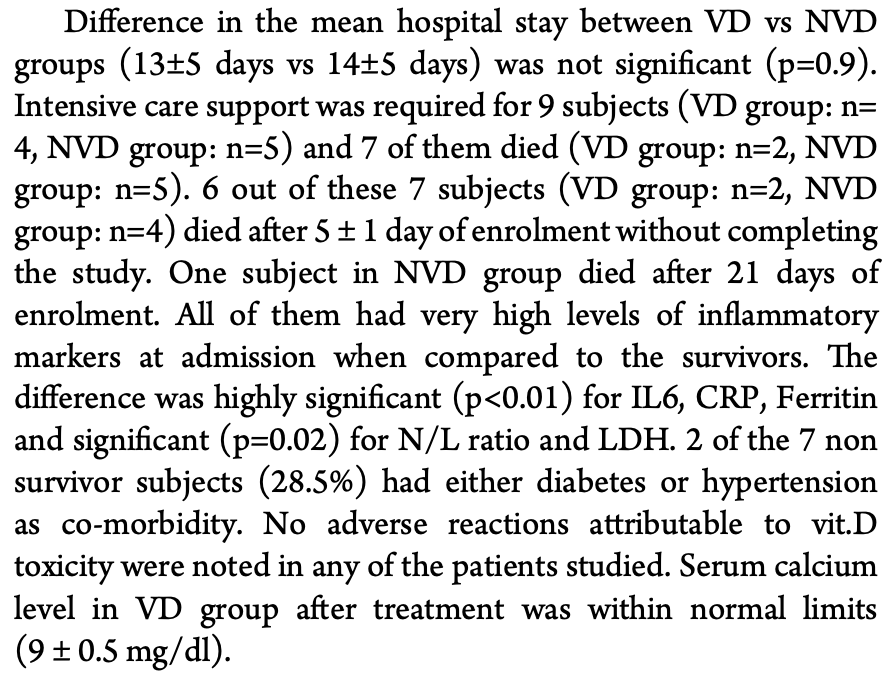 risk of death, 60.9% lower, RR 0.39, p = 0.27, treatment 2 of 44 (4.5%), control 5 of 43 (11.6%). risk of ICU admission, 21.8% lower, RR 0.78, p = 0.74, treatment 4 of 44 (9.1%), control 5 of 43 (11.6%). hospitalization time, 7.1% lower, relative time 0.93, p = 0.90, treatment 44, control 43. Lakkireddy et al., 2/23/2021, Randomized Controlled Trial, India, South Asia, peer-reviewed, mean age 45.5, 9 authors, dosage 60,000IU days 1-8, 8 or 10 days depending on BMI. |
| Submit Corrections or Comments |
| Levels | Gavioli et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1869626 (Peer Reviewed) | death, ↑4.7%, p=0.83 | An Evaluation of Serum 25-Hydroxy Vitamin D Levels in Patients with COVID-19 in New York City |
| Details Retrospective 437 mostly serious condition (85% hospitalized) patients in New York, showing vitamin D deficiency associated with increased likelihood of oxygen support, but no association with mortality and hospitalization. Multivariate a.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Gavioli et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1869626 (Peer Reviewed) |
| An Evaluation of Serum 25-Hydroxy Vitamin D Levels in Patients with COVID-19 in New York City |
Retrospective 437 mostly serious condition (85% hospitalized) patients in New York, showing vitamin D deficiency associated with increased likelihood of oxygen support, but no association with mortality and hospitalization. Multivariate analysis excluded variables with p > 0.2 in univariate analysis. Adjustment for factors correlated with vitamin D may obscure the effect of vitamin D levels. 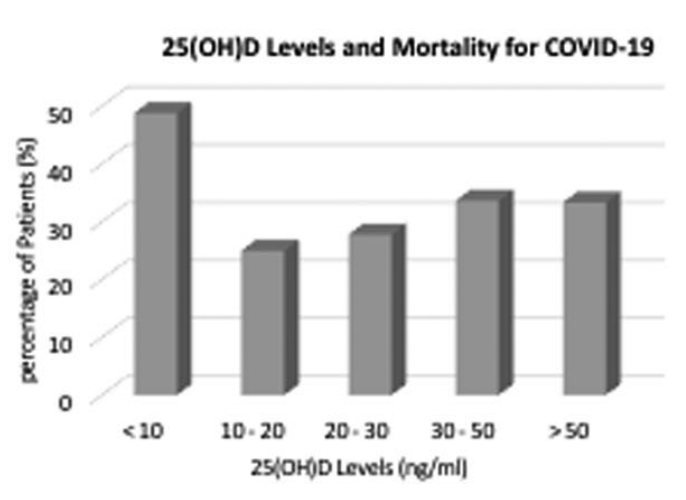 risk of death, 4.7% higher, RR 1.05, p = 0.83, high D levels 80 of 260 (30.8%), low D levels 52 of 177 (29.4%), >20ng/ml. risk of death, 44.8% lower, RR 0.55, p < 0.001, high D levels 102 of 376 (27.1%), low D levels 30 of 61 (49.2%), >10ng/ml. risk of oxygen therapy, 55.2% lower, RR 0.45, p < 0.001, high D levels 127 of 260 (48.8%), low D levels 116 of 177 (65.5%), adjusted, >20ng/ml, multivariate. risk of hospitalization, 3.6% lower, RR 0.96, p = 0.41, high D levels 218 of 260 (83.8%), low D levels 154 of 177 (87.0%), >20ng/ml. Gavioli et al., 2/19/2021, retrospective, USA, North America, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Infante et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2021.1877580 (Peer Reviewed) | death, ↓54.8%, p=0.05 | Low Vitamin D Status at Admission as a Risk Factor for Poor Survival in Hospitalized Patients With COVID-19: An Italian Retrospective Study |
| Details Retrospective 137 hospitalized patients in Italy. All patients had low vitamin D levels, and lower levels were associated with higher mortality. In multivariate logistic regression, vitamin D levels were significantly inversely associate.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Infante et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2021.1877580 (Peer Reviewed) |
| Low Vitamin D Status at Admission as a Risk Factor for Poor Survival in Hospitalized Patients With COVID-19: An Italian Retrospective Study |
Retrospective 137 hospitalized patients in Italy. All patients had low vitamin D levels, and lower levels were associated with higher mortality.In multivariate logistic regression, vitamin D levels were significantly inversely associated with mortality (OR 0.91 [0.85-0.98] p=0.01). 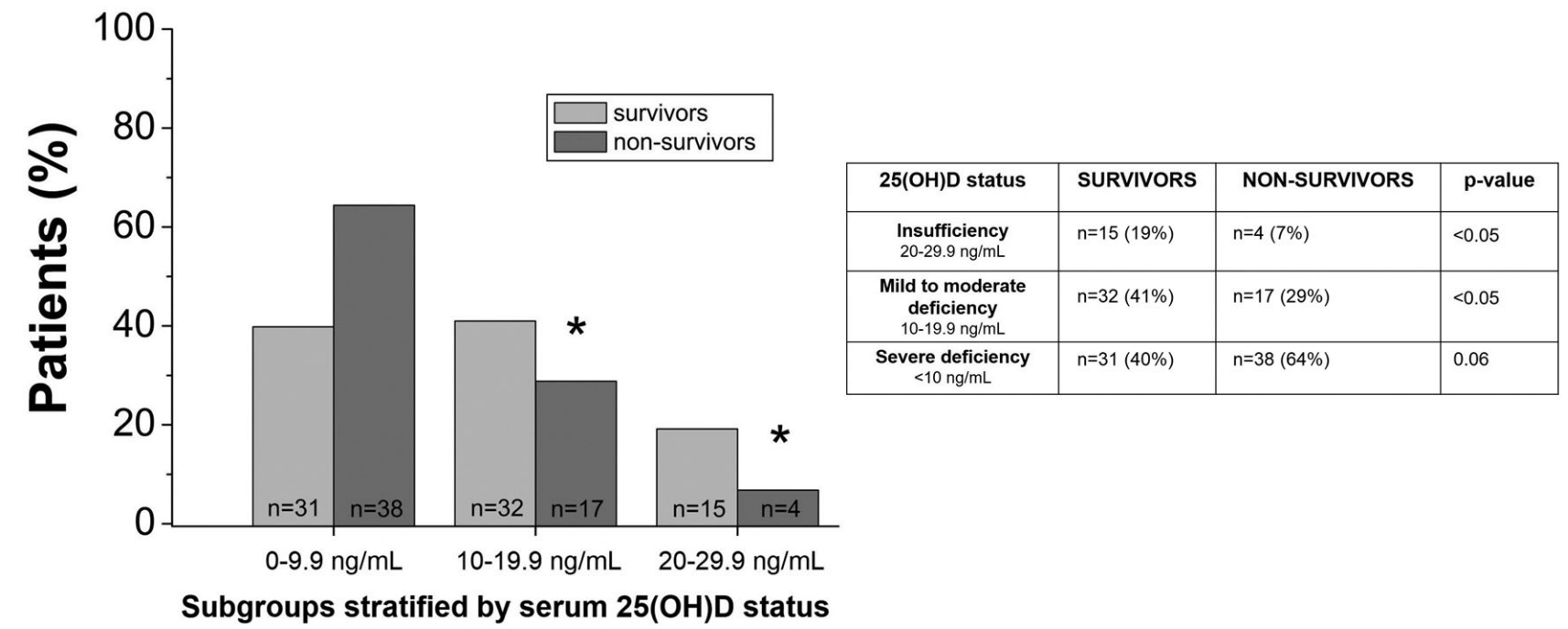 risk of death, 54.8% lower, RR 0.45, p = 0.05, high D levels 4 of 19 (21.1%), low D levels 55 of 118 (46.6%), >20ng/mL. Infante et al., 2/18/2021, retrospective, Italy, Europe, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Early | Burahee et al., SICOT-J, doi:10.1051/sicotj/2021001 (Peer Reviewed) | death, ↓93.3%, p=0.01 | Older patients with proximal femur fractures and SARS-CoV-2 infection – An observational study |
| Details Small retrospective study of 29 hip fracture patients in the UK, 14 with COVID-19. All COVID-19 patients were treated with vitamin D except for 2 where testing and supplementation was missed due to a clerical error. The two COVID-19 patie.. |
| Details Source PDF Early treatment study Early treatment study |
| Burahee et al., SICOT-J, doi:10.1051/sicotj/2021001 (Peer Reviewed) |
| Older patients with proximal femur fractures and SARS-CoV-2 infection – An observational study |
Small retrospective study of 29 hip fracture patients in the UK, 14 with COVID-19. All COVID-19 patients were treated with vitamin D except for 2 where testing and supplementation was missed due to a clerical error. The two COVID-19 patients that died were the two that did not receive vitamin D supplementation.
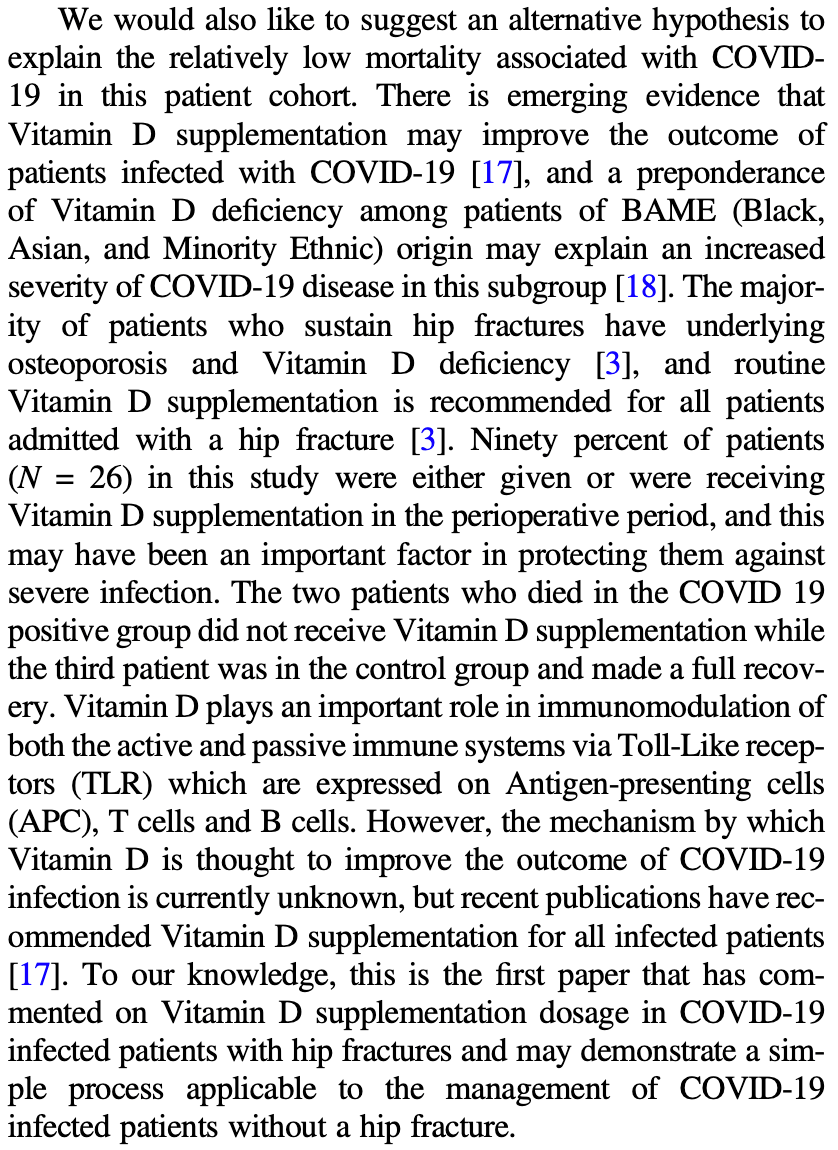 risk of death, 93.3% lower, RR 0.07, p = 0.01, treatment 0 of 12 (0.0%), control 2 of 2 (100.0%), relative risk is not 0 because of continuity correction due to zero events. Burahee et al., 2/17/2021, retrospective, United Kingdom, Europe, peer-reviewed, 4 authors, dosage 100,000IU days 1-4, additional 200000IU over four weeks if serum level insufficient. |
| Submit Corrections or Comments |
| Levels | Basaran et al., Bratislava Medical Journal, doi:10.4149/bll_2021_034 (Peer Reviewed) | severe case, ↓68.6%, p=0.005 | The relationship between vitamin D and the severity of COVID-19 |
| Details Prospective study of 204 patients with COVID-19-like pneumonia in Turkey, 42 outpatients (mild cases), and 162 inpatients (serious cases), showing significantly higher risk of severe cases with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Basaran et al., Bratislava Medical Journal, doi:10.4149/bll_2021_034 (Peer Reviewed) |
| The relationship between vitamin D and the severity of COVID-19 |
Prospective study of 204 patients with COVID-19-like pneumonia in Turkey, 42 outpatients (mild cases), and 162 inpatients (serious cases), showing significantly higher risk of severe cases with vitamin D deficiency. 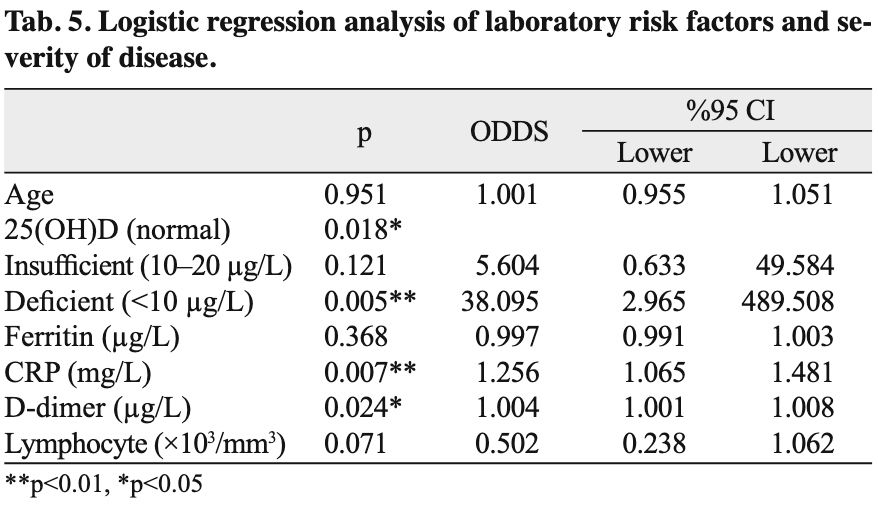 risk of severe case, 68.6% lower, RR 0.31, p = 0.005, high D levels 82 of 119 (68.9%), low D levels 80 of 85 (94.1%), OR converted to RR, >10μg/L, per standard deviation increase in levels. Basaran et al., 2/12/2021, retrospective, Turkey, Europe, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Susianti et al., Journal of Medical Biochemistry, doi:10.5937/jomb0-30228 (Peer Reviewed) | death, ↓91.5%, p=0.32 | Low levels of vitamin D were associated with coagulopathy among hospitalized coronavirus disease-19 (COVID-19) patients: A single-centered study in Indonesia |
| Details Retrospective 50 hospitalized PCR+ patients in Indonesia showing ICU admission, mortality, ISTH DIC (Disseminated Intravascular Coagulation) score>=5, and increased D-dimer significantly associated with lower vitamin D levels. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Susianti et al., Journal of Medical Biochemistry, doi:10.5937/jomb0-30228 (Peer Reviewed) |
| Low levels of vitamin D were associated with coagulopathy among hospitalized coronavirus disease-19 (COVID-19) patients: A single-centered study in Indonesia |
Retrospective 50 hospitalized PCR+ patients in Indonesia showing ICU admission, mortality, ISTH DIC (Disseminated Intravascular Coagulation) score>=5, and increased D-dimer significantly associated with lower vitamin D levels. 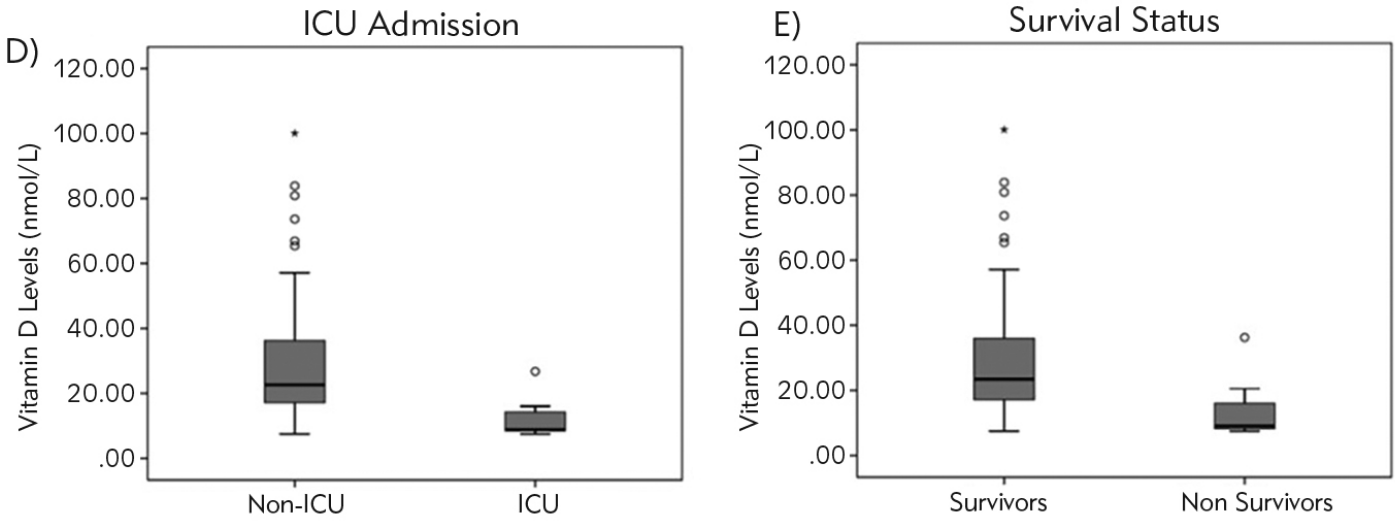 risk of death, 91.5% lower, RR 0.09, p = 0.32, high D levels 0 of 8 (0.0%), low D levels 9 of 42 (21.4%), relative risk is not 0 because of continuity correction due to zero events, >49.92 nmol/L. risk of ICU admission, 90.5% lower, RR 0.10, p = 0.32, high D levels 0 of 8 (0.0%), low D levels 8 of 42 (19.0%), relative risk is not 0 because of continuity correction due to zero events, >49.92 nmol/L. risk of disease progression, 81.5% lower, RR 0.19, p = 0.04, high D levels 8, low D levels 42, ISTH DIC>=5, >49.92 nmol/L, bivariate, RR approximated with OR. risk of disease progression, 44.4% lower, RR 0.56, p = 0.03, high D levels 8, low D levels 42, increased D-dimer >2 mg/L, >49.92 nmol/L, multivariate, RR approximated with OR. Susianti et al., 2/12/2021, retrospective, Indonesia, South Asia, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Hancock et al., SSRN, doi:10.2139/ssrn.3779211 (Preprint) | Case Cluster of RT-PCR COVID-19 Positive Patients with an Unexpected Benign Clinical Course With Vitamin D, Melatonin, Vitamin C, and Viscum Album |
| Details Case series of 24 COVID-19 patients (12 confirmed PCR+) treated with vitamin D, vitamin C, and melatonin, showing positive outcomes with no patient having worse than a mild case, including 7 high risk patients. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Hancock et al., SSRN, doi:10.2139/ssrn.3779211 (Preprint) |
| Case Cluster of RT-PCR COVID-19 Positive Patients with an Unexpected Benign Clinical Course With Vitamin D, Melatonin, Vitamin C, and Viscum Album |
Case series of 24 COVID-19 patients (12 confirmed PCR+) treated with vitamin D, vitamin C, and melatonin, showing positive outcomes with no patient having worse than a mild case, including 7 high risk patients. 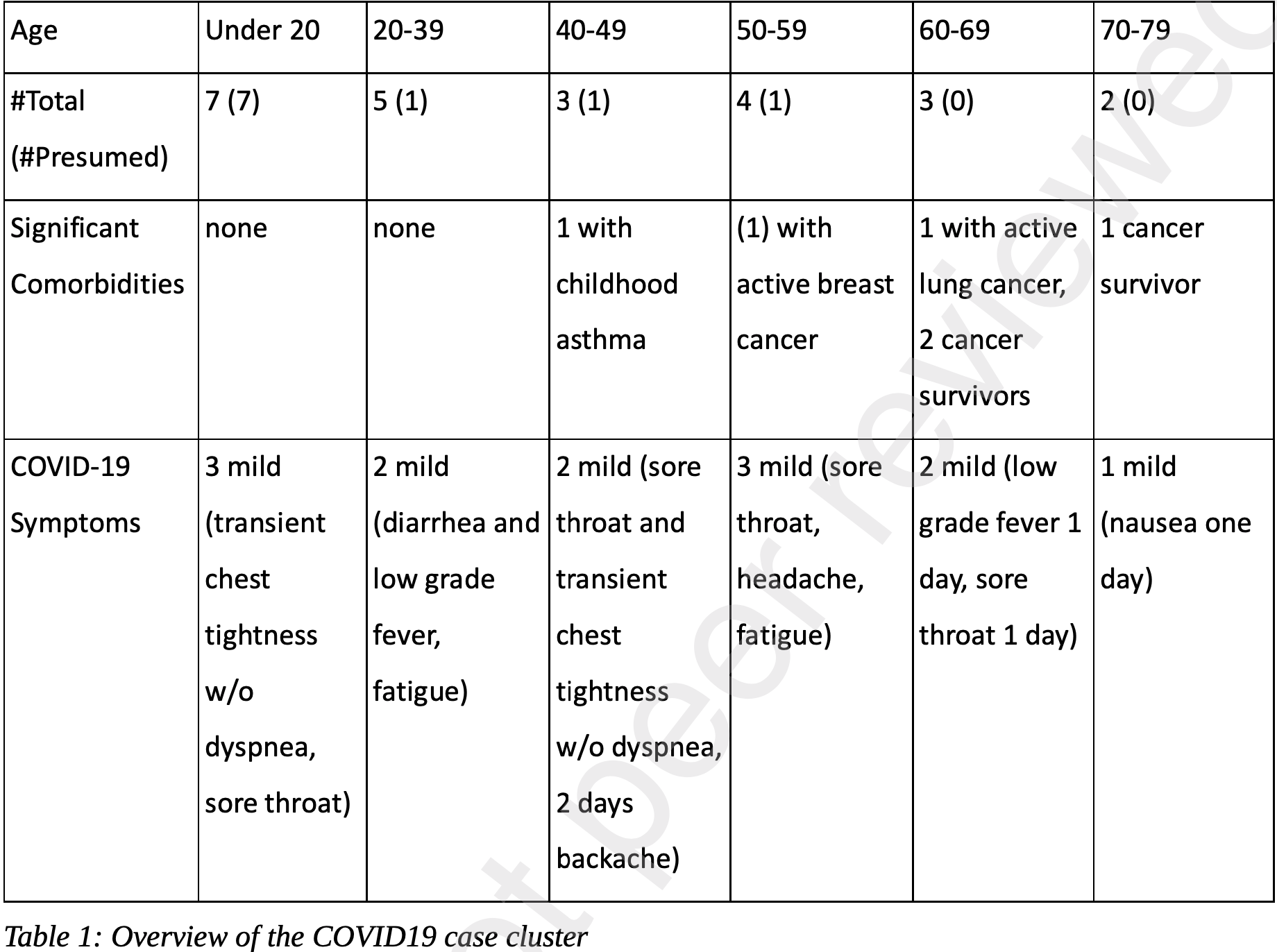 Hancock et al., 2/9/2021, preprint, 4 authors. |
| Submit Corrections or Comments |
| Levels | Yadav et al., Indian Journal of Clinical Biochemistry, doi:10.1007/s12291-020-00950-1 (Peer Reviewed) | Association of Vitamin D Status with COVID-19 Infection and Mortality in the Asia Pacific region: A Cross-Sectional Study |
| Details Analysis of vitamin D levels and COVID-19 in 37 Asia Pacific countries, finding a significant association with the number of cases/million (r = −0.394, p = 0.016) and a weak association with the number of deaths/ million (r = −0.280, p .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Yadav et al., Indian Journal of Clinical Biochemistry, doi:10.1007/s12291-020-00950-1 (Peer Reviewed) |
| Association of Vitamin D Status with COVID-19 Infection and Mortality in the Asia Pacific region: A Cross-Sectional Study |
Analysis of vitamin D levels and COVID-19 in 37 Asia Pacific countries, finding a significant association with the number of cases/million (r = −0.394, p = 0.016) and a weak association with the number of deaths/ million (r = −0.280, p = 0.093). 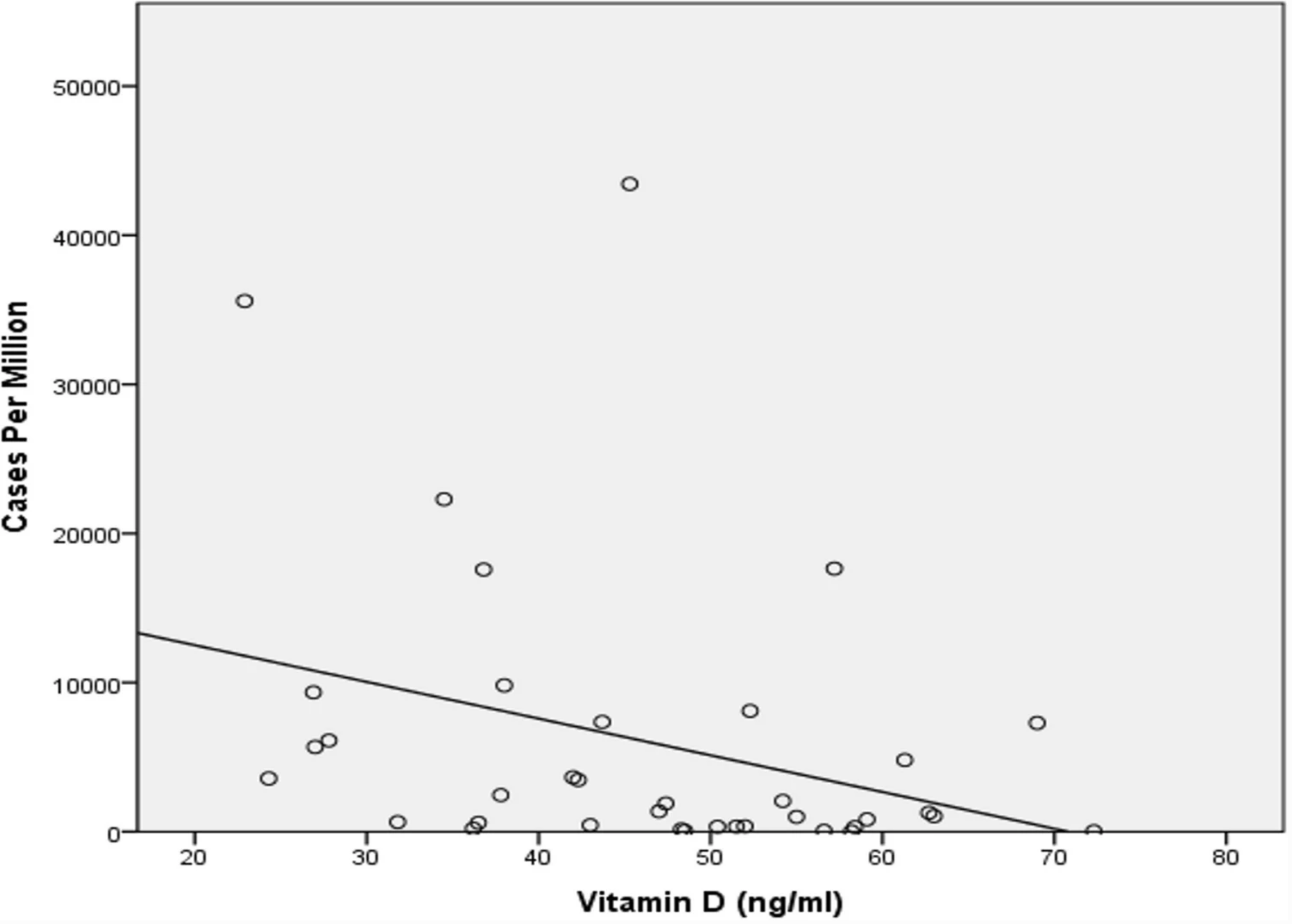 Yadav et al., 2/3/2021, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Söbü et al., The Journal of Current Pediatrics, doi:10.4274/jcp.2021.0002 (Peer Reviewed) | Vitamin D Levels of COVID-19 Positive Sypmtomatic Pediatric Cases |
| Details Retrospective 30 hospitalized pediatric COVID-19 patients and 82 healthy controls, showing significantly lower vitamin D levels in COVID-19 patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Söbü et al., The Journal of Current Pediatrics, doi:10.4274/jcp.2021.0002 (Peer Reviewed) |
| Vitamin D Levels of COVID-19 Positive Sypmtomatic Pediatric Cases |
Retrospective 30 hospitalized pediatric COVID-19 patients and 82 healthy controls, showing significantly lower vitamin D levels in COVID-19 patients. 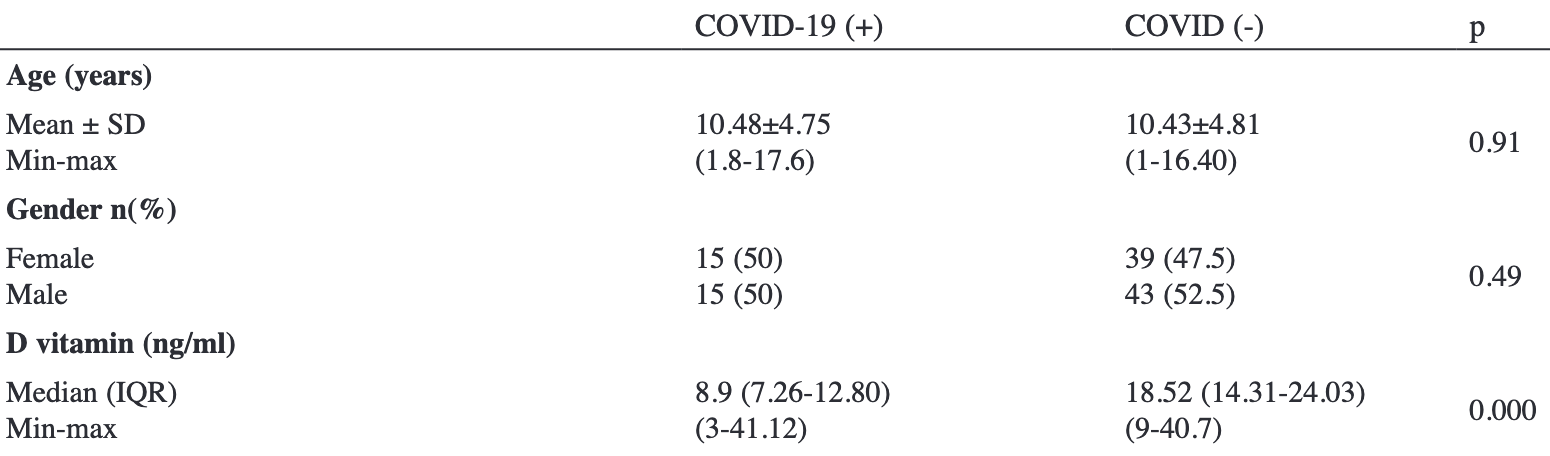 Söbü et al., 2/2/2021, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Patchen et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000255 (Peer Reviewed) | severe case, ↓2.0%, p=0.11 | Genetically predicted serum vitamin D and COVID-19: a Mendelian randomization study |
| Details UK Biobank Mendelian randomization study not finding significant differences in COVID-19 risk. The number of people predicted to have vitamin D deficiency does not appear to be provided. For some background on Mendelian randomization stu.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Patchen et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000255 (Peer Reviewed) |
| Genetically predicted serum vitamin D and COVID-19: a Mendelian randomization study |
UK Biobank Mendelian randomization study not finding significant differences in COVID-19 risk. The number of people predicted to have vitamin D deficiency does not appear to be provided.For some background on Mendelian randomization studies and their limitations see [1].For reasons why Mendelian randomization may fail in this case, see [2]. Authors suggest that it may come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response. For most other purposes, it may not matter much that unbound (free) 25-OHD is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25-OHD and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all. 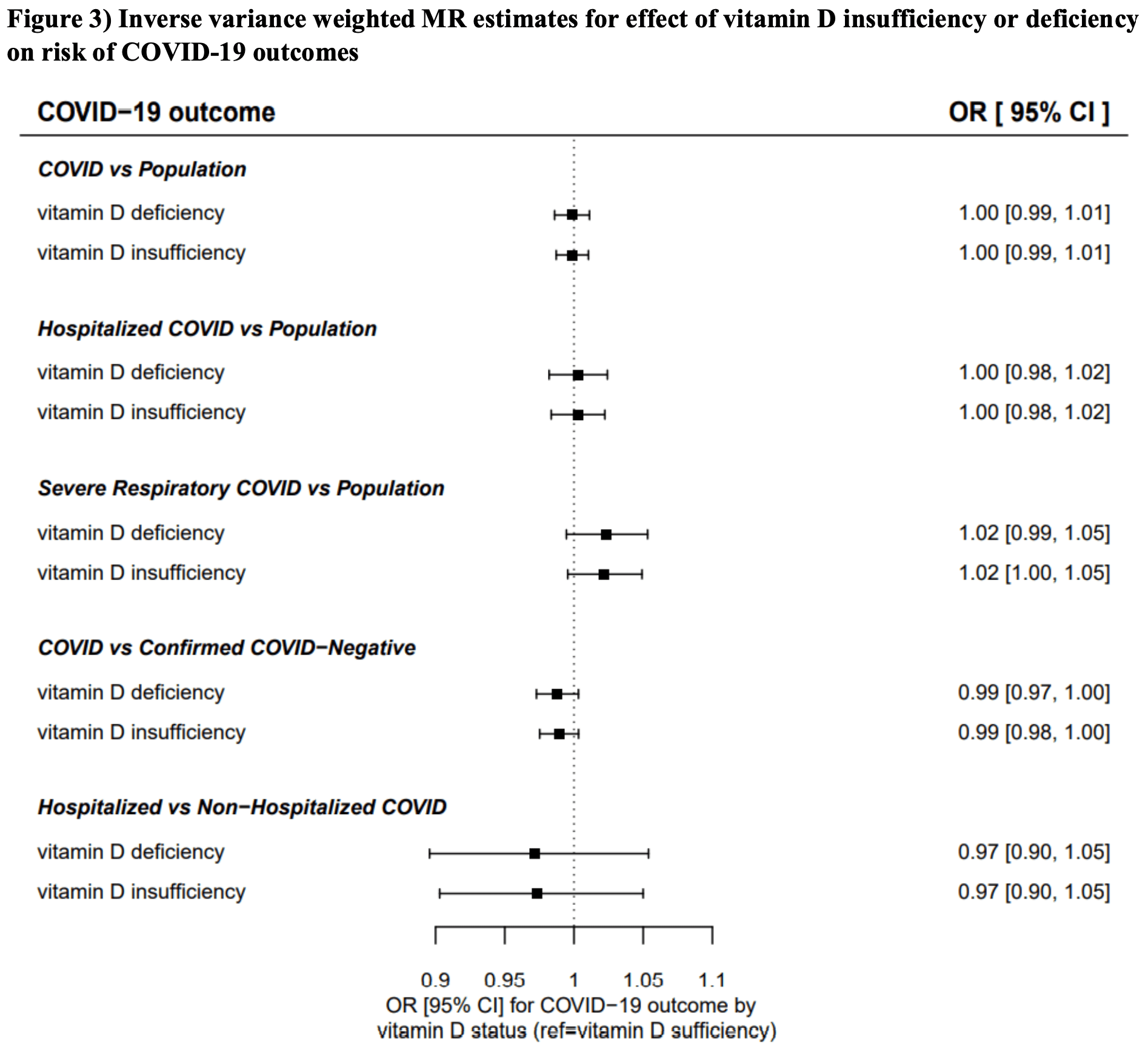 risk of severe case, 2.0% lower, RR 0.98, p = 0.11, OR converted to RR, >50nmol/L, baseline risk approximated with overall risk. risk of hospitalization, no change, RR 1.00, p = 1.00, OR converted to RR, >50nmol/L, baseline risk approximated with overall risk. risk of case, no change, RR 1.00, p = 1.00, OR converted to RR, >50nmol/L, baseline risk approximated with overall risk. Patchen et al., 2/1/2021, retrospective, United Kingdom, Europe, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Nadiger et al., Critical Care Medicine, doi:10.1097/01.ccm.0000726440.30551.47 (Peer Reviewed) | Vitamin D Levels in Children With COVID-19 Admitted to the PICU |
| Details Retrospective 14 pediatric COVID-19 ICU patients showing that the majority were vitamin D deficient. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Nadiger et al., Critical Care Medicine, doi:10.1097/01.ccm.0000726440.30551.47 (Peer Reviewed) |
| Vitamin D Levels in Children With COVID-19 Admitted to the PICU |
Retrospective 14 pediatric COVID-19 ICU patients showing that the majority were vitamin D deficient. 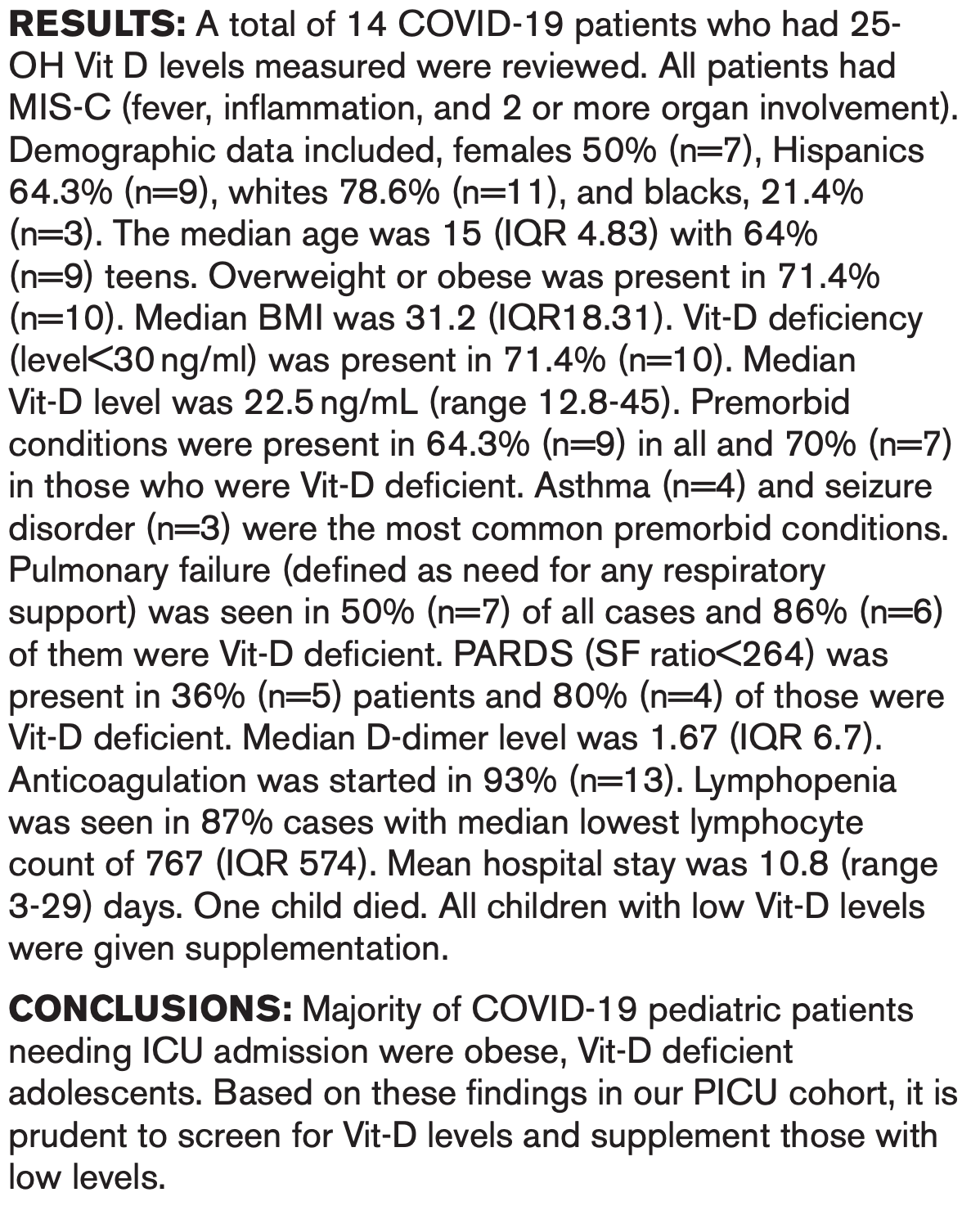 Nadiger et al., 1/31/2021, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Demir et al., Journal of Medical Virology, doi:10.1002/jmv.26832 (Peer Reviewed) | severe case, ↓89.3%, p<0.001 | Vitamin D deficiency is associated with COVID‐19 positivity and the severity of the disease |
| Details Retrospective cohort study of 487 patients finding that lower vitamin D levels is associated with more severe cases as measured by affected lung segments and increased hospitalization time for COVID-19 positive patients, and that lower vi.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Demir et al., Journal of Medical Virology, doi:10.1002/jmv.26832 (Peer Reviewed) |
| Vitamin D deficiency is associated with COVID‐19 positivity and the severity of the disease |
Retrospective cohort study of 487 patients finding that lower vitamin D levels is associated with more severe cases as measured by affected lung segments and increased hospitalization time for COVID-19 positive patients, and that lower vitamin D levels increases COVID-19 PCR+ cases. 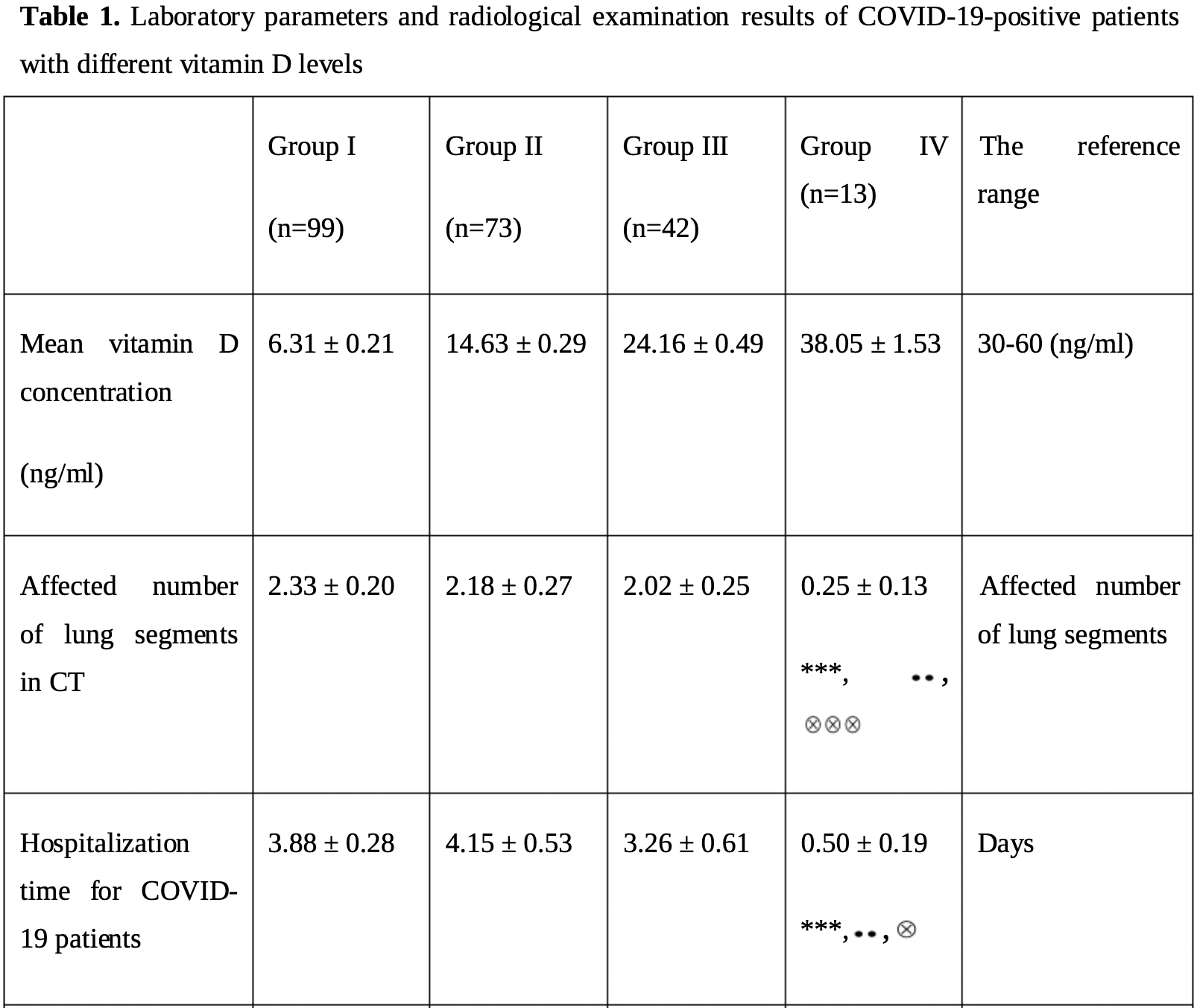 risk of severe case, 89.3% lower, RR 0.11, p < 0.001, high D levels 13, low D levels 99, ratio of the mean number of affected lung segments, >30ng/ml vs. <=10ng/mL. hospitalization time, 87.1% lower, relative time 0.13, p < 0.001, high D levels 13, low D levels 99, >30ng/ml vs. <=10ng/mL. risk of case, 24.2% lower, RR 0.76, p = 0.18, high D levels 13 of 31 (41.9%), low D levels 99 of 179 (55.3%), >30ng/ml vs. <=10ng/mL. Demir et al., 1/29/2021, retrospective, Turkey, Europe, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Ma et al., The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqaa381 (Peer Reviewed) | cases, ↓30.0%, p=0.03 | Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank |
| Details Retrospective 8,297 adults from the UK Biobank showing the habitual use of vitamin D supplements significantly associated with lower risk of COVID-19 cases. Note that the information on vitamin D supplement use was collected a median of 1.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Ma et al., The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqaa381 (Peer Reviewed) |
| Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank |
Retrospective 8,297 adults from the UK Biobank showing the habitual use of vitamin D supplements significantly associated with lower risk of COVID-19 cases. Note that the information on vitamin D supplement use was collected a median of 10 years before the COVID-19 tests, so usage may have changed significantly. 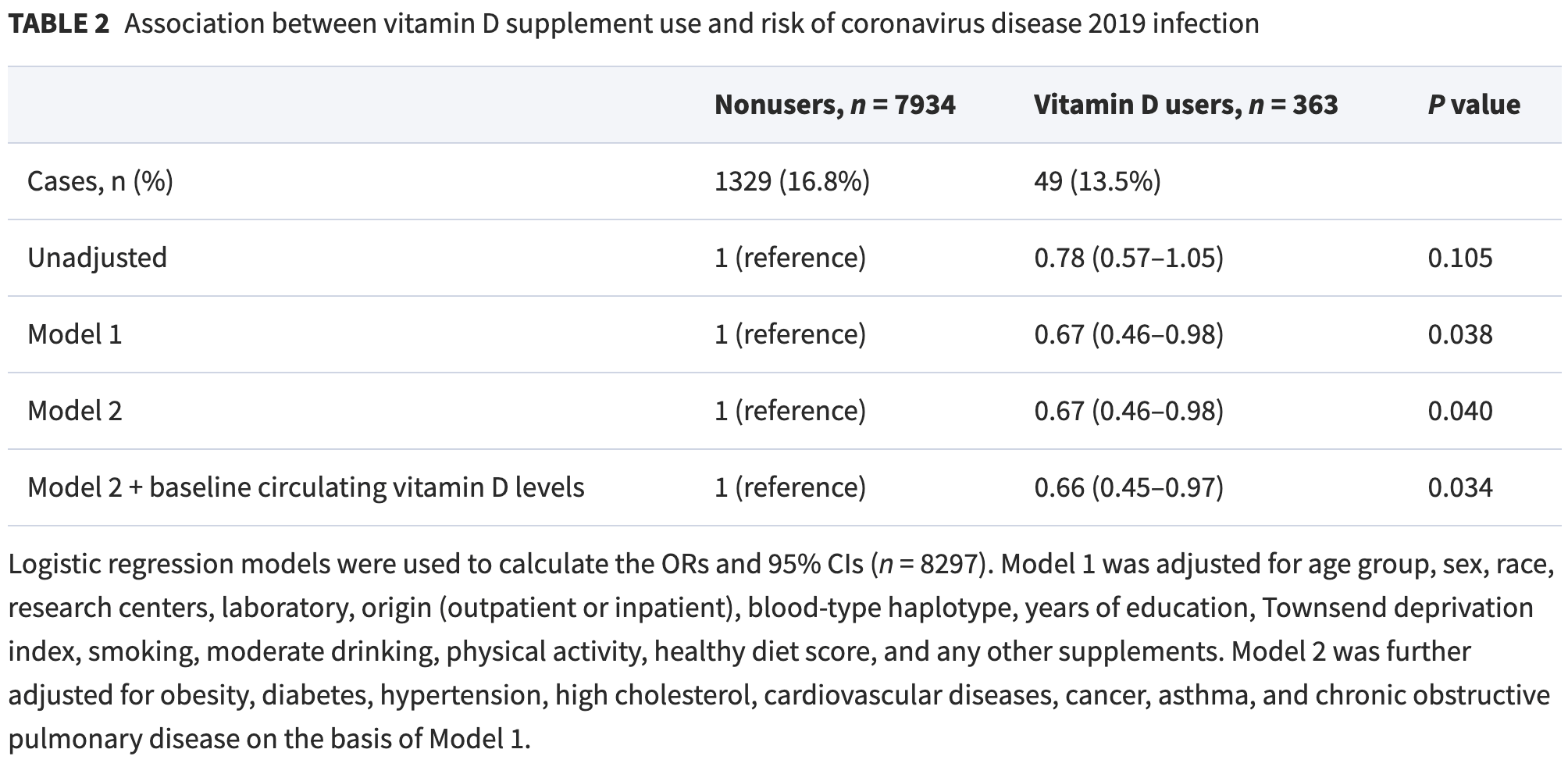 risk of case, 30.0% lower, RR 0.70, p = 0.03, treatment 49 of 363 (13.5%), control 1,329 of 7,934 (16.8%), adjusted, OR converted to RR. Ma et al., 1/29/2021, retrospective, United Kingdom, Europe, peer-reviewed, 4 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Rafailia et al., medRxiv, doi:10.1101/2021.01.28.21250673 (Preprint) | Is vitamin D deficiency associated with the COVID-19 epidemic in Europe |
| Details Analysis of vitamin D deficiency and COVID-19 cases and mortality in European countries showing significant correlations with infections (r=0.82, p<0.001) and mortality (r=0.53, p=0.05). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Rafailia et al., medRxiv, doi:10.1101/2021.01.28.21250673 (Preprint) |
| Is vitamin D deficiency associated with the COVID-19 epidemic in Europe |
Analysis of vitamin D deficiency and COVID-19 cases and mortality in European countries showing significant correlations with infections (r=0.82, p<0.001) and mortality (r=0.53, p=0.05).  Rafailia et al., 1/29/2021, retrospective, multiple countries, multiple regions, preprint, 2 authors. |
| Submit Corrections or Comments |
| Review | Brenner, H., Nutrients, doi:10.3390/nu13020411 (Review) (Peer Reviewed) | review | Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths—Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action |
| Details Summary of epidemiological and intervention studies for vitamin D supplementation. Author concludes that despite limitations, evidence strongly supports widespread supplementation, in particular for high-risk populations, as well as high-.. |
| Details Source PDF Review Review |
| Brenner, H., Nutrients, doi:10.3390/nu13020411 (Review) (Peer Reviewed) |
| Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths—Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action |
Summary of epidemiological and intervention studies for vitamin D supplementation. Author concludes that despite limitations, evidence strongly supports widespread supplementation, in particular for high-risk populations, as well as high-dose supplementation for those infected. 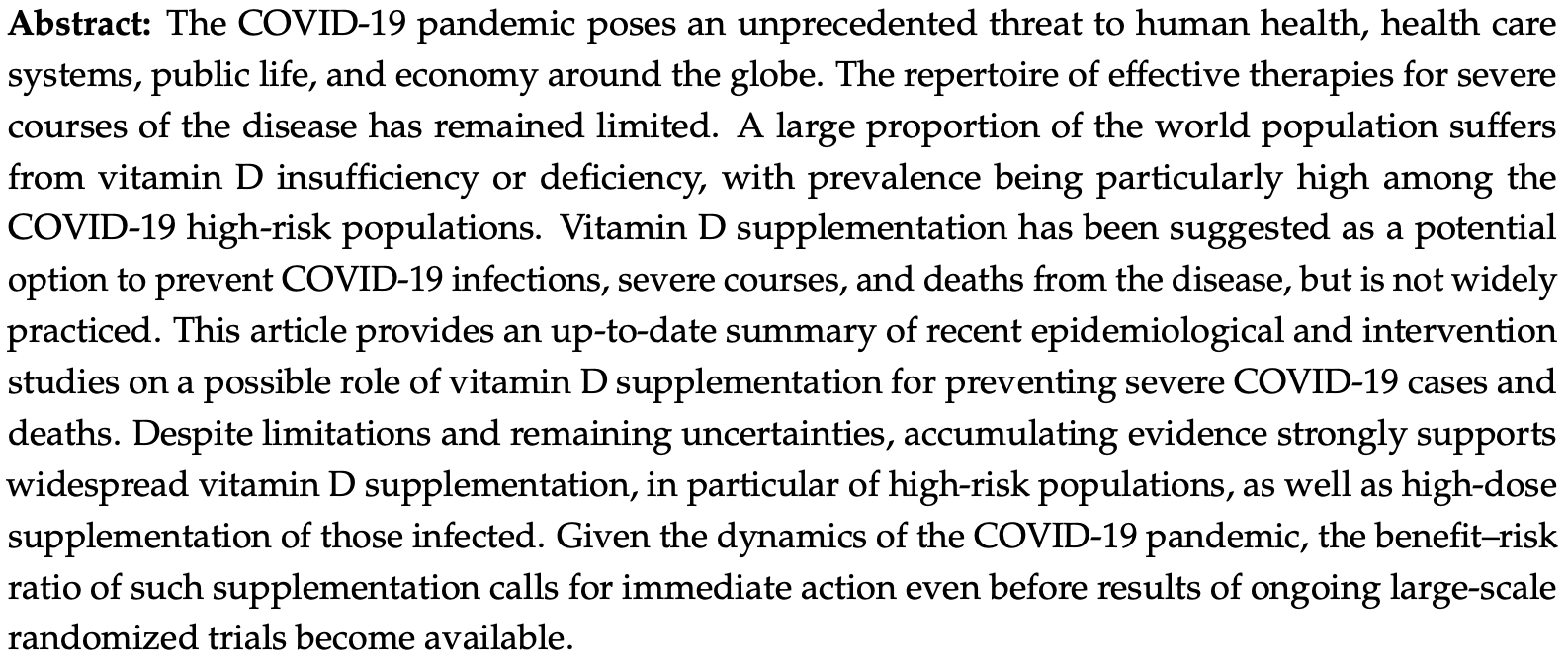 Brenner et al., 1/28/2021, peer-reviewed, 1 author. |
| Submit Corrections or Comments |
| Levels | Tehrani et al., Clinical Nutrition, doi:10.1016/j.clnesp.2021.01.014 (Peer Reviewed) | death, ↓47.5%, p=0.07 | Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and mortality |
| Details Retrospective 205 patients in Iran, showing higher mortality with vitamin D deficiency, not quite reaching statistical significance. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Tehrani et al., Clinical Nutrition, doi:10.1016/j.clnesp.2021.01.014 (Peer Reviewed) |
| Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and mortality |
Retrospective 205 patients in Iran, showing higher mortality with vitamin D deficiency, not quite reaching statistical significance. 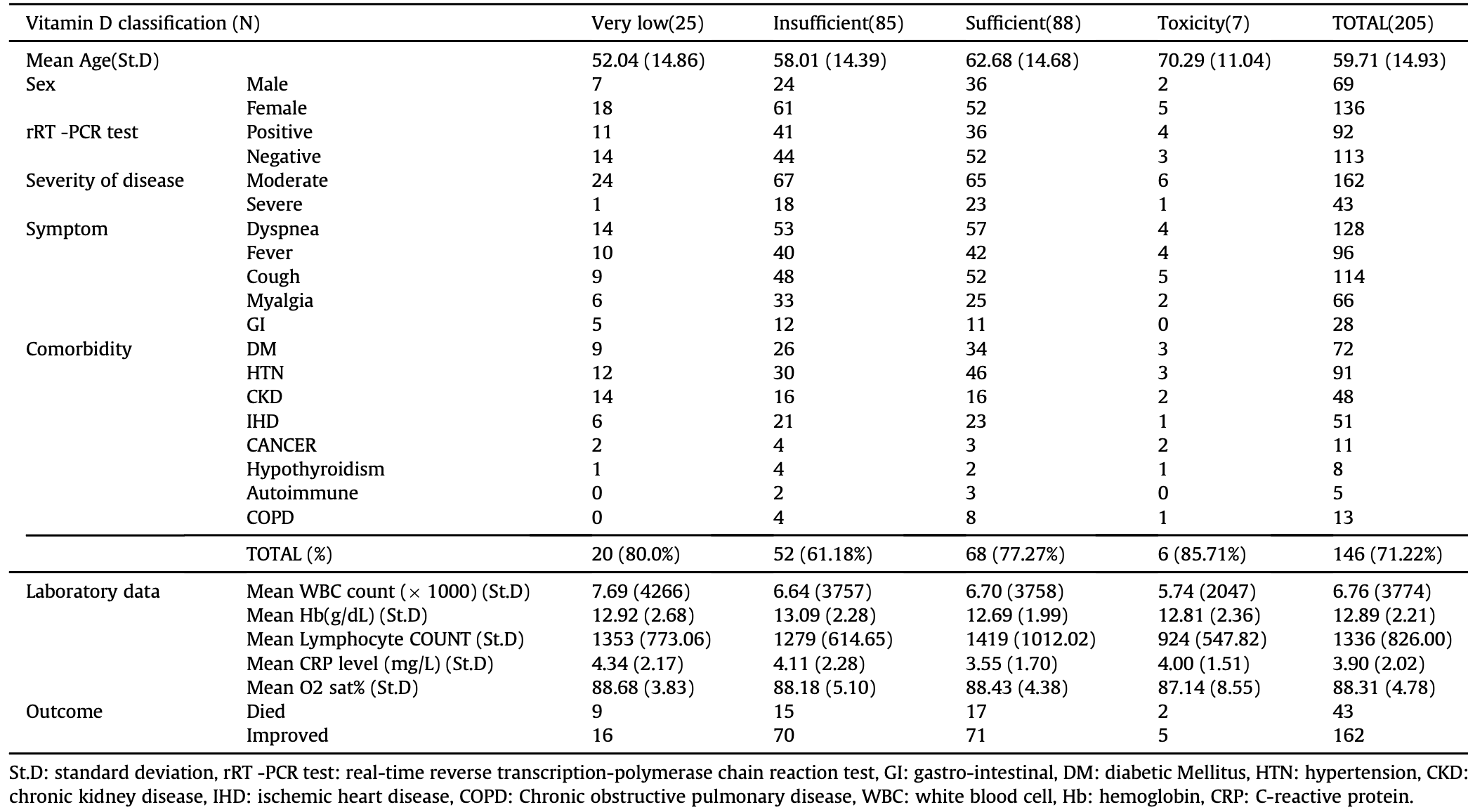 risk of death, 47.5% lower, RR 0.52, p = 0.07, high D levels 34 of 180 (18.9%), low D levels 9 of 25 (36.0%), >10ng/ml. Tehrani et al., 1/25/2021, retrospective, Iran, Middle East, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Barassi et al., Panminerva Med., doi:10.23736/S0031-0808.21.04277-4 (Peer Reviewed) | death, ↓64.9%, p=0.44 | Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support |
| Details Retrospective 118 consecutive hospitalized PCR+ patients in Italy showing higher ventilation and mortality with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Barassi et al., Panminerva Med., doi:10.23736/S0031-0808.21.04277-4 (Peer Reviewed) |
| Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support |
Retrospective 118 consecutive hospitalized PCR+ patients in Italy showing higher ventilation and mortality with vitamin D deficiency. 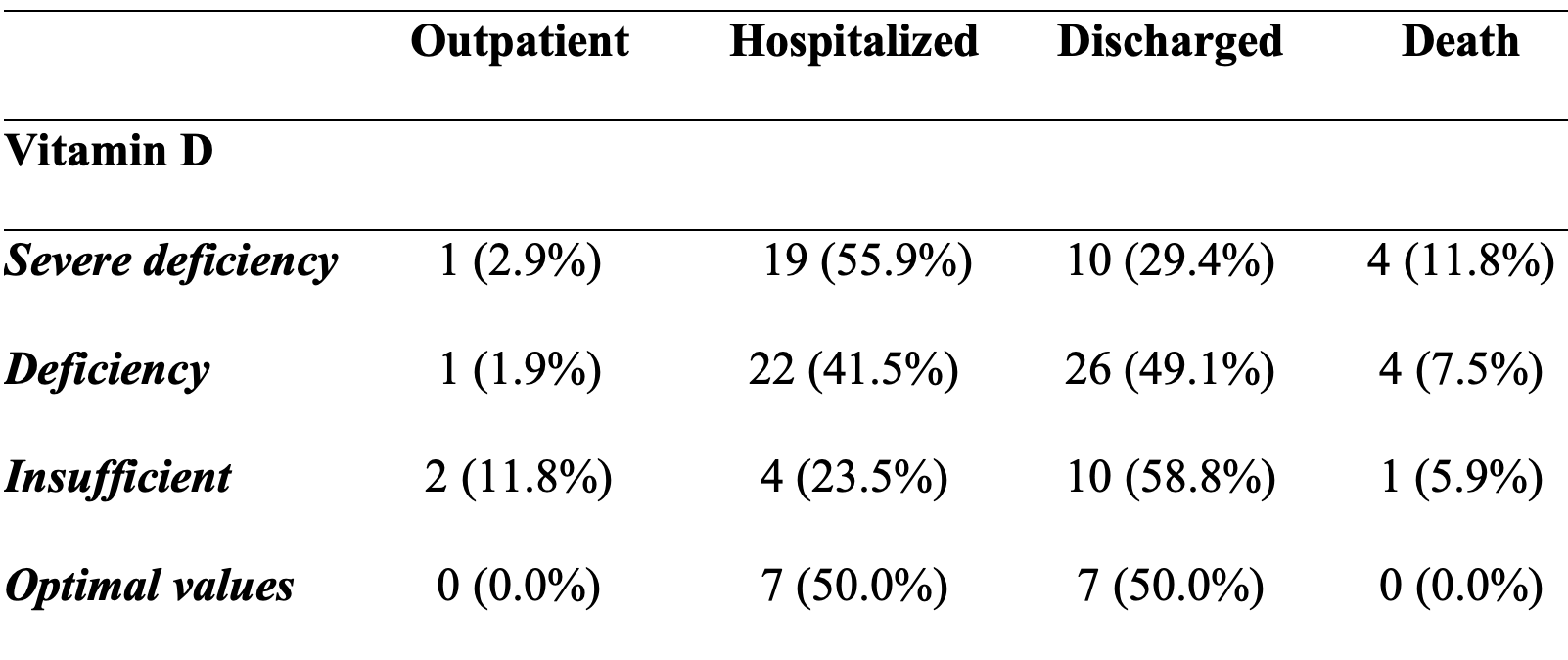 risk of death, 64.9% lower, RR 0.35, p = 0.44, high D levels 1 of 31 (3.2%), low D levels 8 of 87 (9.2%), >20ng/mL. risk of mechanical ventilation, 64.9% lower, RR 0.35, p = 0.15, high D levels 2 of 31 (6.5%), low D levels 16 of 87 (18.4%), >20ng/mL. Barassi et al., 1/25/2021, retrospective, Italy, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Late | Nogués et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab405 (Peer Reviewed) | death, ↓79.0%, p=0.001 | Calcifediol Treatment and COVID-19-Related Outcomes |
| Details Quasi-randomized trial with 930 hospitalized patients, 447 treated with calcifediol, showing significantly lower ICU admission and death with treatment. Note that the randomization in this trial is by ward. Authors report that patients we.. |
| Details Source PDF Late treatment study Late treatment study |
| Nogués et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab405 (Peer Reviewed) |
| Calcifediol Treatment and COVID-19-Related Outcomes |
Quasi-randomized trial with 930 hospitalized patients, 447 treated with calcifediol, showing significantly lower ICU admission and death with treatment. Note that the randomization in this trial is by ward. Authors report that patients were allocated to empty beds available at admission time regardless of patient conditions, and that staff in all wards followed the same protocol.The earlier preprint for this article was censored by the Lancet. The Lancet reportedly requested a review from a Twitter user that posted negative comments [1]. The review provides useful feedback for the authors to improve the reporting of the cluster nature of the RCT, and to explain the delay in registration, however it is highly unusual to censor a preprint in this way. Authors responded to the issues raised here: [2] 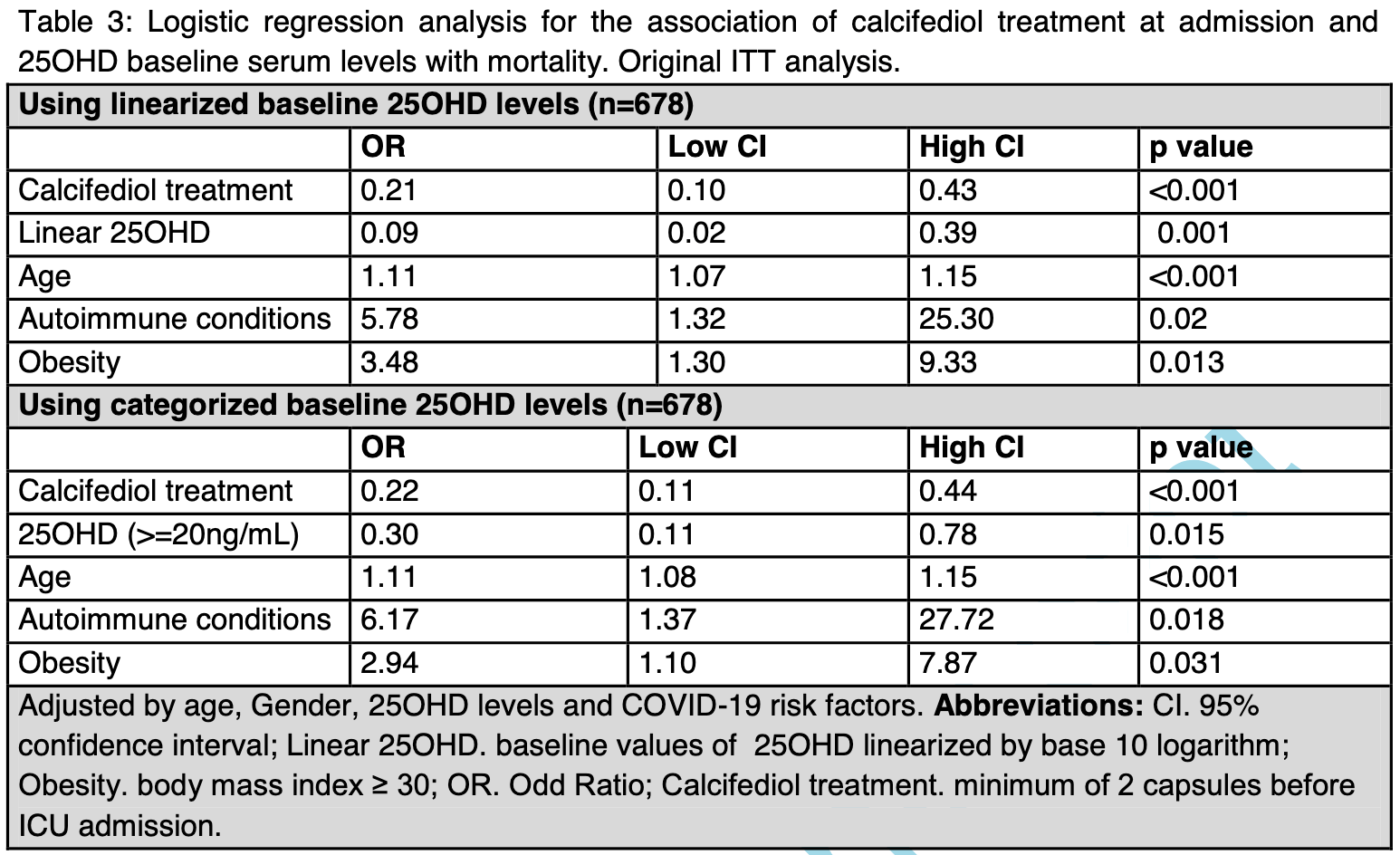 risk of death, 79.0% lower, RR 0.21, p = 0.001, treatment 21 of 447 (4.7%), control 62 of 391 (15.9%), adjusted, ITT. risk of death, 48.0% lower, RR 0.52, p = 0.001, treatment 500, control 338, adjusted, including patients treated later. risk of ICU admission, 87.0% lower, RR 0.13, p < 0.001, treatment 20 of 447 (4.5%), control 82 of 391 (21.0%), adjusted, ITT. Nogués et al., 1/22/2021, prospective quasi-randomized (ward), Spain, Europe, peer-reviewed, 16 authors, dosage calcifediol 0.5mg day 1, 0.27mg day 3, 0.27mg day 7, 0.27mg day 15, 0.27mg day 30. |
| Submit Corrections or Comments |
| Levels | Walrand, S., Nature, doi:10.1038/s41598-021-81419-w (Peer Reviewed) | Autumn COVID-19 surge dates in Europe correlated to latitudes, not to temperature-humidity, pointing to vitamin D as contributing factor |
| Details Analysis of the increase in COVID-19 cases in European countries, showing no correlation with temperature, but a significant correlation with country latitude. Since UV radiation decreases earlier for higher latitudes, this supports the t.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Walrand, S., Nature, doi:10.1038/s41598-021-81419-w (Peer Reviewed) |
| Autumn COVID-19 surge dates in Europe correlated to latitudes, not to temperature-humidity, pointing to vitamin D as contributing factor |
Analysis of the increase in COVID-19 cases in European countries, showing no correlation with temperature, but a significant correlation with country latitude. Since UV radiation decreases earlier for higher latitudes, this supports the theory that low vitamin D levels increases COVID-19 risk.Author recommends that vitamin D supplementation be considered to reduce pandemic severity during the winter, noting that UV levels in Europe and Northern USA will not return to a level above that of October until the end of March. 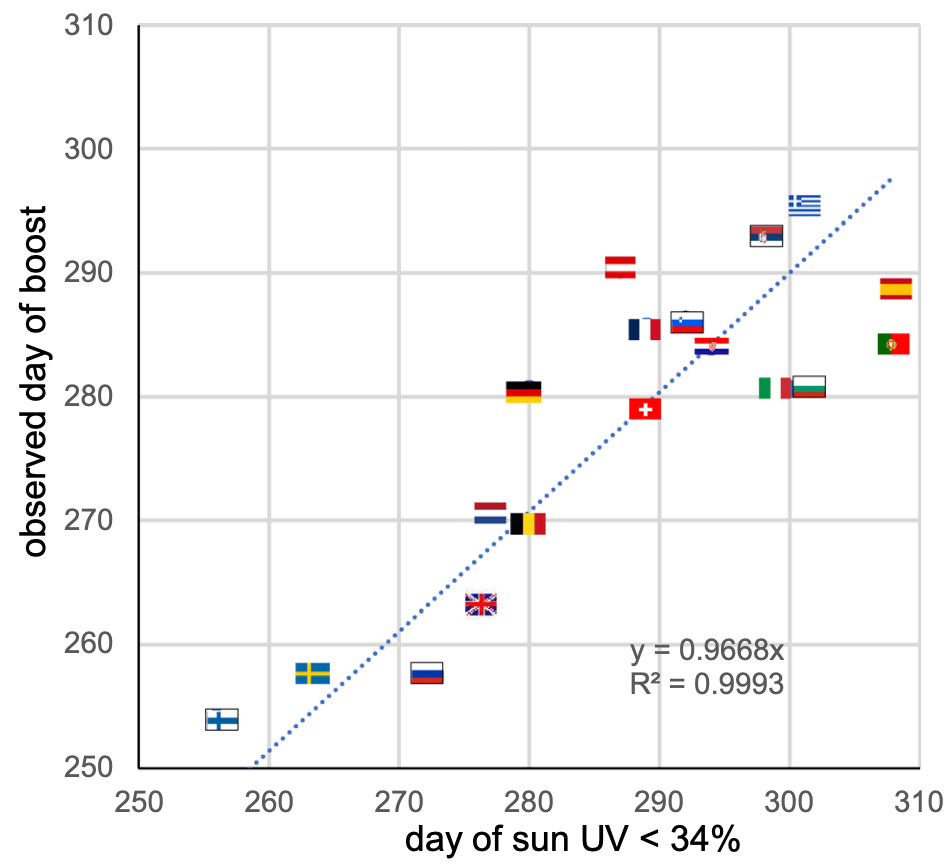 Walrand et al., 1/21/2021, peer-reviewed, 1 author. |
| Submit Corrections or Comments |
| Levels | Orchard et al., Clin Chem Lab Med, doi:10.1515/cclm-2020-1567 (Peer Reviewed) | ICU, ↓58.8%, p=0.001 | Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients |
| Details Retrospective 165 hospitalized patients with known vitamin D levels, showing an associated between vitamin D deficiency and ICU admission. There was no statistically significant difference in clinical outcomes for ICU patients. It's uncle.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Orchard et al., Clin Chem Lab Med, doi:10.1515/cclm-2020-1567 (Peer Reviewed) |
| Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients |
Retrospective 165 hospitalized patients with known vitamin D levels, showing an associated between vitamin D deficiency and ICU admission. There was no statistically significant difference in clinical outcomes for ICU patients. It's unclear why authors do not provide clinical outcomes for all patients rather than ICU only. 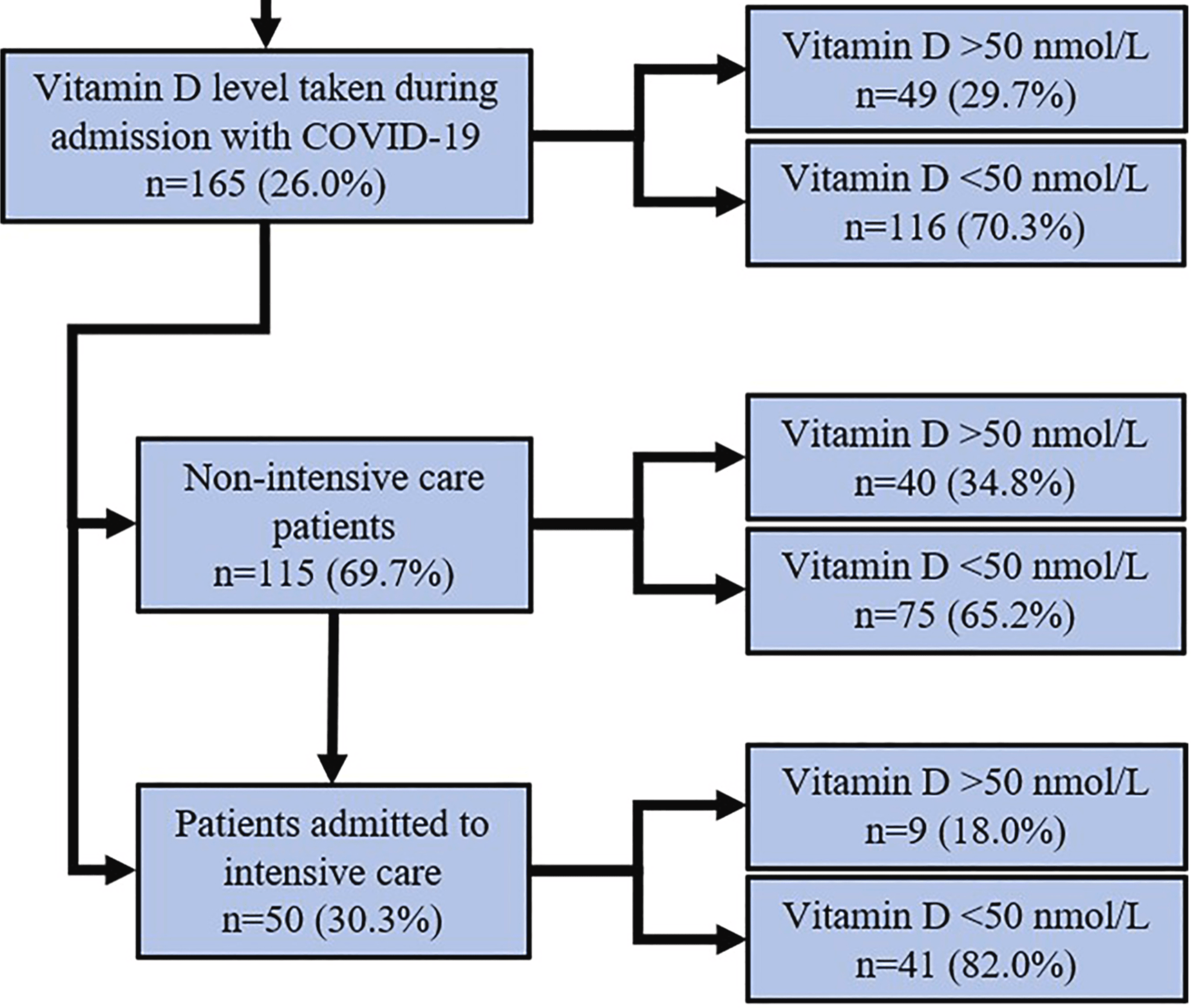 risk of ICU admission, 58.8% lower, RR 0.41, p = 0.001, high D levels 9 of 40 (22.5%), low D levels 41 of 75 (54.7%), all hospitalized patients, >50 nmol/L. risk of death, 24.1% lower, RR 0.76, p = 1.00, high D levels 1 of 9 (11.1%), low D levels 6 of 41 (14.6%), ICU patients only, >50 nmol/L. risk of mechanical ventilation, 8.9% lower, RR 0.91, p = 0.70, high D levels 6 of 9 (66.7%), low D levels 30 of 41 (73.2%), ICU patients only, >50 nmol/L. Orchard et al., 1/19/2021, retrospective, United Kingdom, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Vasheghani et al., Scientific Reports, doi:10.1038/s41598-021-97017-9 (preprint 1/18/2021) (Preprint) | death, ↓30.4%, p=0.45 | The relationship between serum 25-hydroxyvitamin D levels and the severity of COVID-19 disease and its mortality |
| Details Retrospective 508 hospitalized COVID-19 patients in Iran showing lower mortality with vitamin D supplementation (not reaching statistical significance), and an association between lower vitamin D levels and disease severity, ICU admission.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Vasheghani et al., Scientific Reports, doi:10.1038/s41598-021-97017-9 (preprint 1/18/2021) (Preprint) |
| The relationship between serum 25-hydroxyvitamin D levels and the severity of COVID-19 disease and its mortality |
Retrospective 508 hospitalized COVID-19 patients in Iran showing lower mortality with vitamin D supplementation (not reaching statistical significance), and an association between lower vitamin D levels and disease severity, ICU admission, and increased mortality. Details of supplementation are not provided. The multivariate result for vitamin D deficiency is in the preprint, the journal version only contains the multivariate result for serum level. 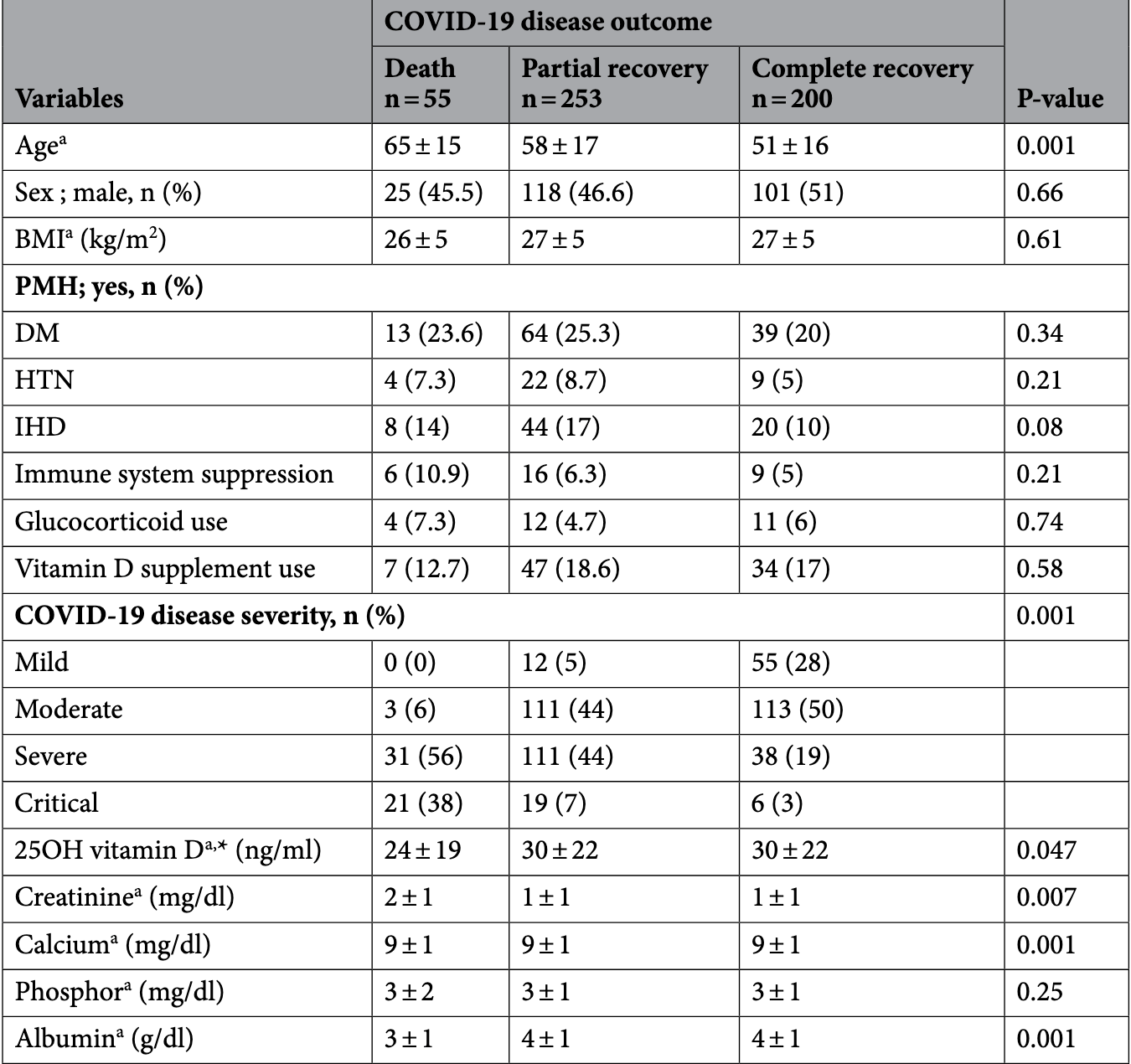 risk of death, 30.4% lower, RR 0.70, p = 0.45, treatment 7 of 88 (8.0%), control 48 of 420 (11.4%), vitamin D supplementation. risk of ICU admission, 63.8% lower, RR 0.36, p = 0.009, treatment 13 of 185 (7.0%), control 53 of 323 (16.4%), adjusted, vitamin D levels >30ng/mL. Vasheghani et al., 1/18/2021, retrospective, Iran, Middle East, preprint, 6 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | Hutchings et al., Endocrine, doi:/10.1007/s12020-020-02597-7 (Peer Reviewed) | Patients hospitalized with COVID-19 have low levels of 25-hydroxyvitamin D |
| Details Retrospective 330 hospitalized COVID-19 patients in Armenia, showing significantly higher prevalence of vitamin D deficiency (<12ng/mL) compared to health controls (45% vs. 13%). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Hutchings et al., Endocrine, doi:/10.1007/s12020-020-02597-7 (Peer Reviewed) |
| Patients hospitalized with COVID-19 have low levels of 25-hydroxyvitamin D |
Retrospective 330 hospitalized COVID-19 patients in Armenia, showing significantly higher prevalence of vitamin D deficiency (<12ng/mL) compared to health controls (45% vs. 13%). 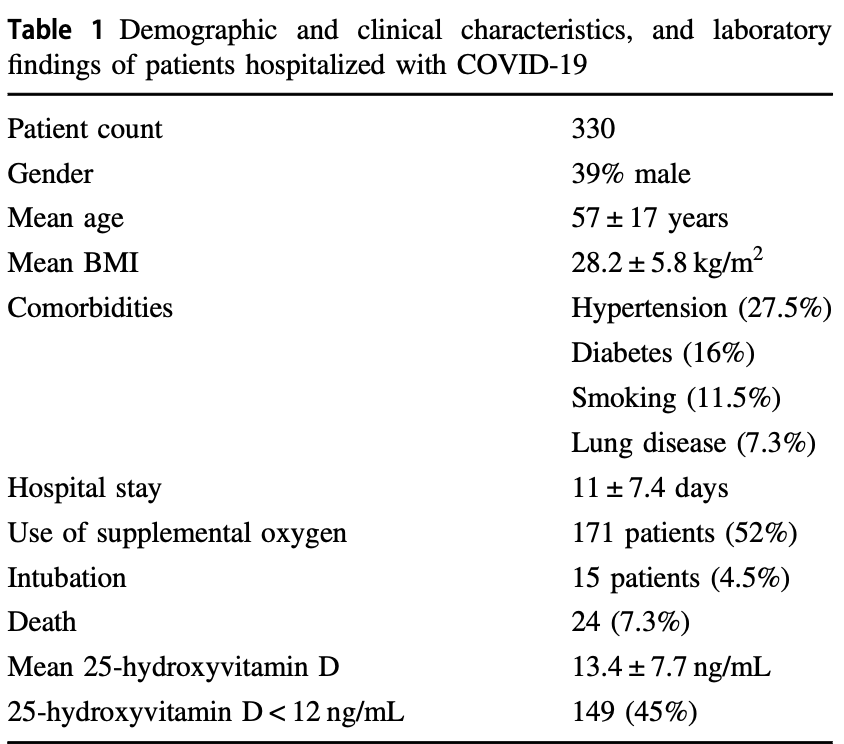 Hutchings et al., 1/16/2021, retrospective, Armenia, Asia, peer-reviewed, 12 authors. |
| Submit Corrections or Comments |
| Late | Giannini et al., Nutrients, doi:10.3390/nu13010219 (Peer Reviewed) | death/ICU, ↓36.6%, p=0.13 | Effectiveness of In-Hospital Cholecalciferol Use on Clinical Outcomes in Comorbid COVID-19 Patients: A Hypothesis-Generating Study |
| Details Retrospective 91 hospitalized patients, 36 treated with high-dose cholecalciferol, showing lower combined death/ICU admission with treatment. Authors also analyze the relationship with comorbidity burden, finding that the positive effect.. |
| Details Source PDF Late treatment study Late treatment study |
| Giannini et al., Nutrients, doi:10.3390/nu13010219 (Peer Reviewed) |
| Effectiveness of In-Hospital Cholecalciferol Use on Clinical Outcomes in Comorbid COVID-19 Patients: A Hypothesis-Generating Study |
Retrospective 91 hospitalized patients, 36 treated with high-dose cholecalciferol, showing lower combined death/ICU admission with treatment.Authors also analyze the relationship with comorbidity burden, finding that the positive effect of high-dose cholecalciferol on the combined endpoint was significantly amplified with increasing comorbidity burden. 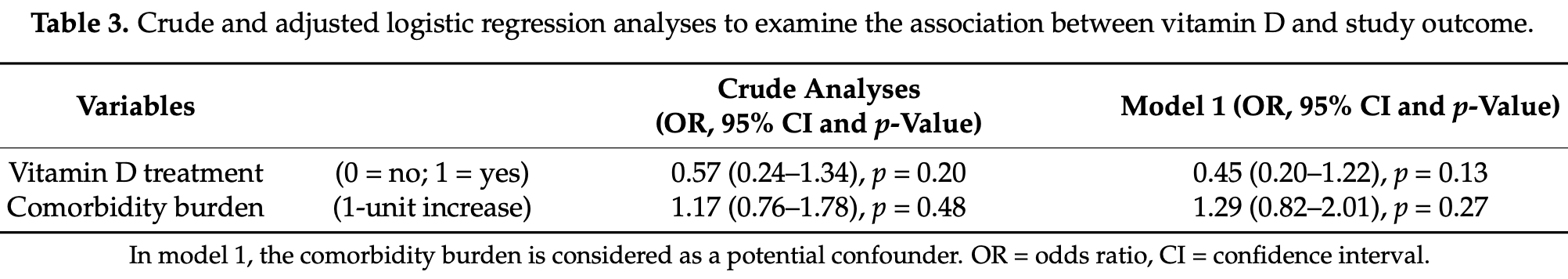 risk of death/ICU, 36.6% lower, RR 0.63, p = 0.13, treatment 14 of 36 (38.9%), control 29 of 55 (52.7%), OR converted to RR. Giannini et al., 1/14/2021, retrospective, Italy, Europe, peer-reviewed, 21 authors, dosage 200,000IU days 1-2. |
| Submit Corrections or Comments |
| Levels | Bennouar et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1856013 (Peer Reviewed) | death, ↓85.5%, p=0.002 | Vitamin D Deficiency and Low Serum Calcium as Predictors of Poor Prognosis in Patients with Severe COVID-19 |
| Details Prospective study of 120 severe cases of COVID-19 in Algeria finding low vitamin D and low calcium both associated with increased mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Bennouar et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1856013 (Peer Reviewed) |
| Vitamin D Deficiency and Low Serum Calcium as Predictors of Poor Prognosis in Patients with Severe COVID-19 |
Prospective study of 120 severe cases of COVID-19 in Algeria finding low vitamin D and low calcium both associated with increased mortality. 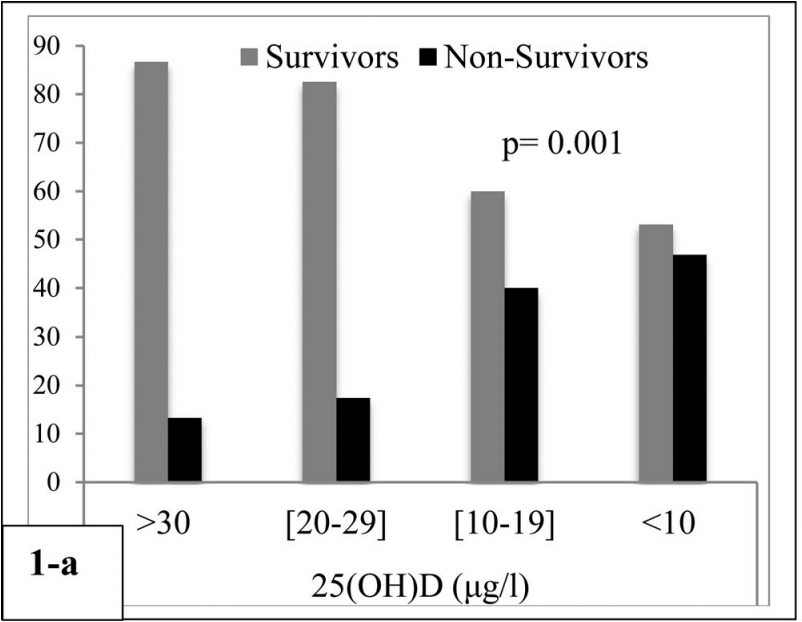 risk of death, 85.5% lower, RR 0.14, p = 0.002, high D levels 4 of 30 (13.3%), low D levels 15 of 32 (46.9%), adjusted, >30μg/l vs. <10μg/l, proportional Cox regression. risk of death, 63.0% lower, RR 0.37, p = 0.10, high D levels 4 of 30 (13.3%), low D levels 14 of 35 (40.0%), adjusted, >30μg/l vs. 10-19μg/l, proportional Cox regression. risk of death, 23.1% lower, RR 0.77, p = 0.73, high D levels 4 of 30 (13.3%), low D levels 4 of 23 (17.4%), adjusted, >30μg/l vs. 20-29μg/l, proportional Cox regression. Bennouar et al., 1/12/2021, prospective, Algeria, Africa, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Li et al., Aging and Disease, doi:10.14336/AD.2020.1108 (Peer Reviewed) | severe case, ↓36.2%, p<0.0001 | Metabolic Healthy Obesity, Vitamin D Status, and Risk of COVID-19 |
| Details UK Biobank retrospective 353,299 patients showing that vitamin D insufficiency and deficiency are associated with increased COVID-19 risk. This study also analyzes metabolic/obesity phenotypes and the combination with vitamin D status. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Li et al., Aging and Disease, doi:10.14336/AD.2020.1108 (Peer Reviewed) |
| Metabolic Healthy Obesity, Vitamin D Status, and Risk of COVID-19 |
UK Biobank retrospective 353,299 patients showing that vitamin D insufficiency and deficiency are associated with increased COVID-19 risk. This study also analyzes metabolic/obesity phenotypes and the combination with vitamin D status. 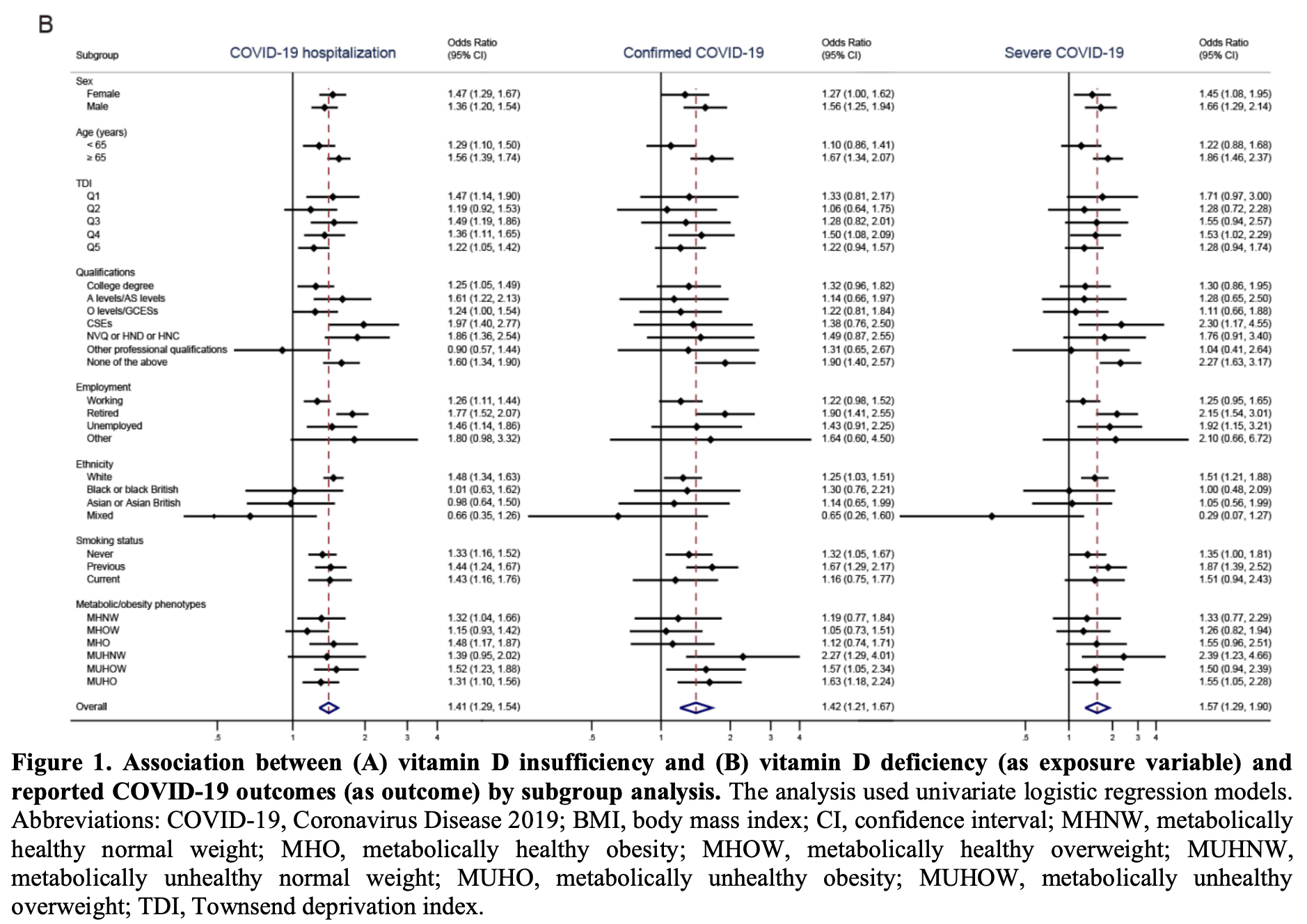 risk of severe case, 36.2% lower, RR 0.64, p < 0.001, OR converted to RR, >25nmol/L. risk of hospitalization, 28.8% lower, RR 0.71, p < 0.001, OR converted to RR, >25nmol/L. risk of case, 29.5% lower, RR 0.71, p < 0.001, OR converted to RR, >25nmol/L. Li et al., 1/11/2021, retrospective, population-based cohort, United Kingdom, Europe, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Angelidi et al., Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2021.01.001 (Peer Reviewed) | death, ↓88.0%, p=0.01 | Vitamin D Status is Associated With In-hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients |
| Details Retrospective 144 patients in the USA showing significantly lower mortality for vitamin D levels >=30ng/mL. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Angelidi et al., Mayo Clinic Proceedings, doi:10.1016/j.mayocp.2021.01.001 (Peer Reviewed) |
| Vitamin D Status is Associated With In-hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients |
Retrospective 144 patients in the USA showing significantly lower mortality for vitamin D levels >=30ng/mL. 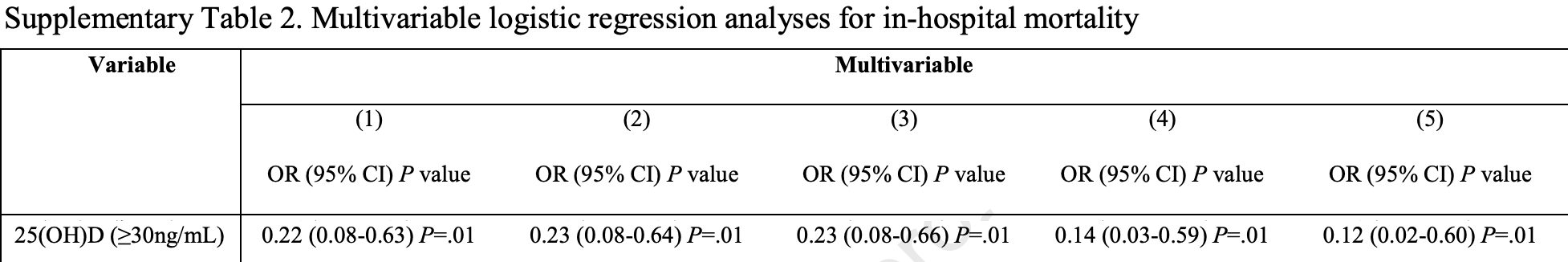 risk of death, 88.0% lower, RR 0.12, p = 0.01, high D levels 6 of 65 (9.2%), low D levels 20 of 79 (25.3%), adjusted, >30ng/mL, supplementary table 2, multivariable logistic regression model 5. Angelidi et al., 1/9/2021, retrospective, USA, North America, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Pal et al., Frontiers in Medicine, doi:10.3389/fmed.2020.590805 (Peer Reviewed) | High Prevalence of Hypocalcemia in Non-severe COVID-19 Patients: A Retrospective Case-Control Study |
| Details Retrospective 72 non-severe COVID-19 patients in India, showing very high levels of vitamin D deficiency (70 of 72 patients). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Pal et al., Frontiers in Medicine, doi:10.3389/fmed.2020.590805 (Peer Reviewed) |
| High Prevalence of Hypocalcemia in Non-severe COVID-19 Patients: A Retrospective Case-Control Study |
Retrospective 72 non-severe COVID-19 patients in India, showing very high levels of vitamin D deficiency (70 of 72 patients). 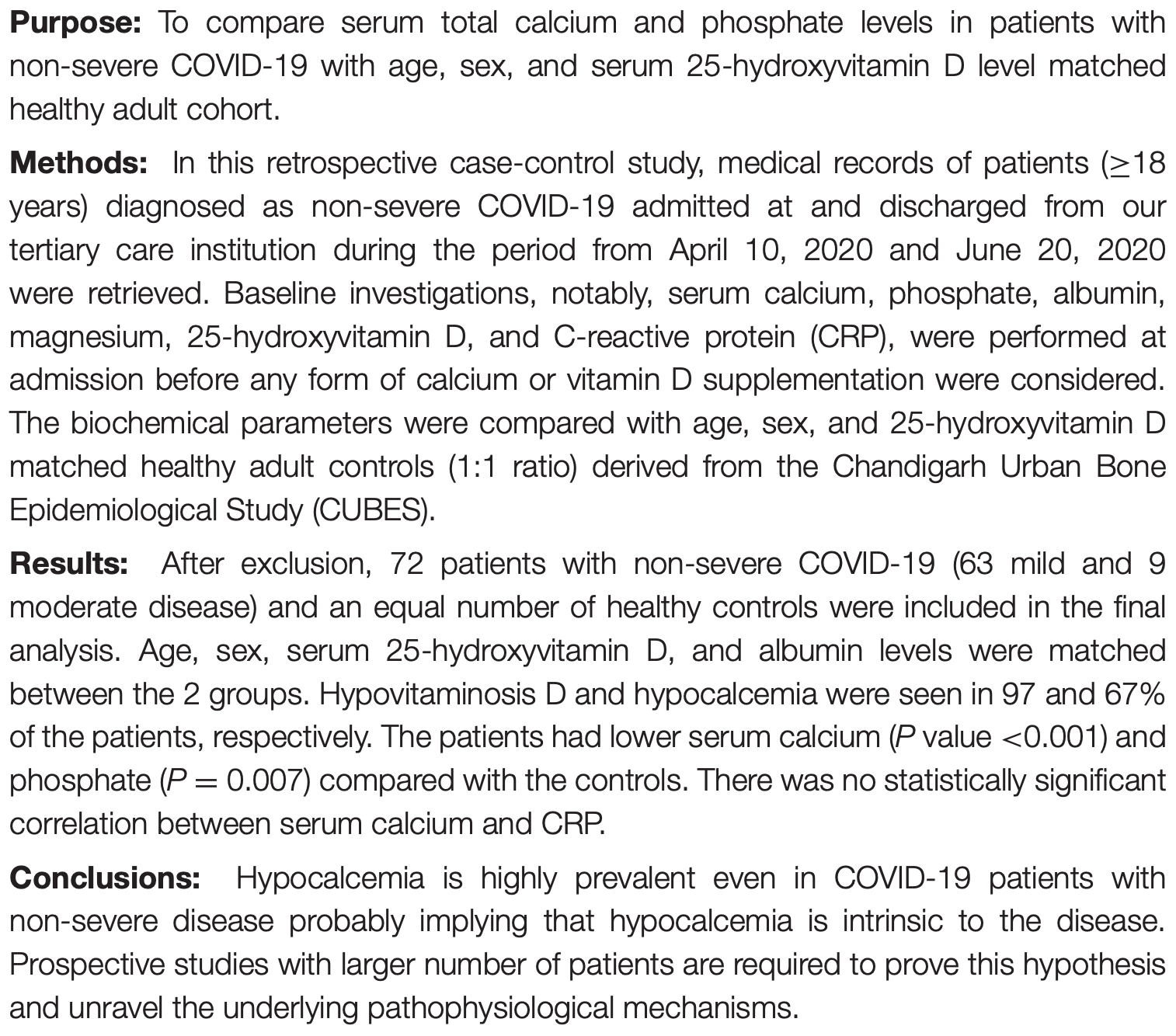 Pal et al., 1/7/2021, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Amin et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2020-000151 (Peer Reviewed) | progression, ↑32.3%, p=0.20 | No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data |
| Details Analysis of vitamin D levels and COVID-19 cases and severity based on genetic predisposition to higher vitamin D levels or lower vitamin D deficiency, finding no significant association. For some background on Mendelian randomization stu.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Amin et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2020-000151 (Peer Reviewed) |
| No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data |
Analysis of vitamin D levels and COVID-19 cases and severity based on genetic predisposition to higher vitamin D levels or lower vitamin D deficiency, finding no significant association.For some background on Mendelian randomization studies and their limitations see [1].For reasons why Mendelian randomization may fail in this case, see [2]. Authors suggest that it may come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response. For most other purposes, it may not matter much that unbound (free) 25-OHD is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25-OHD and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all. 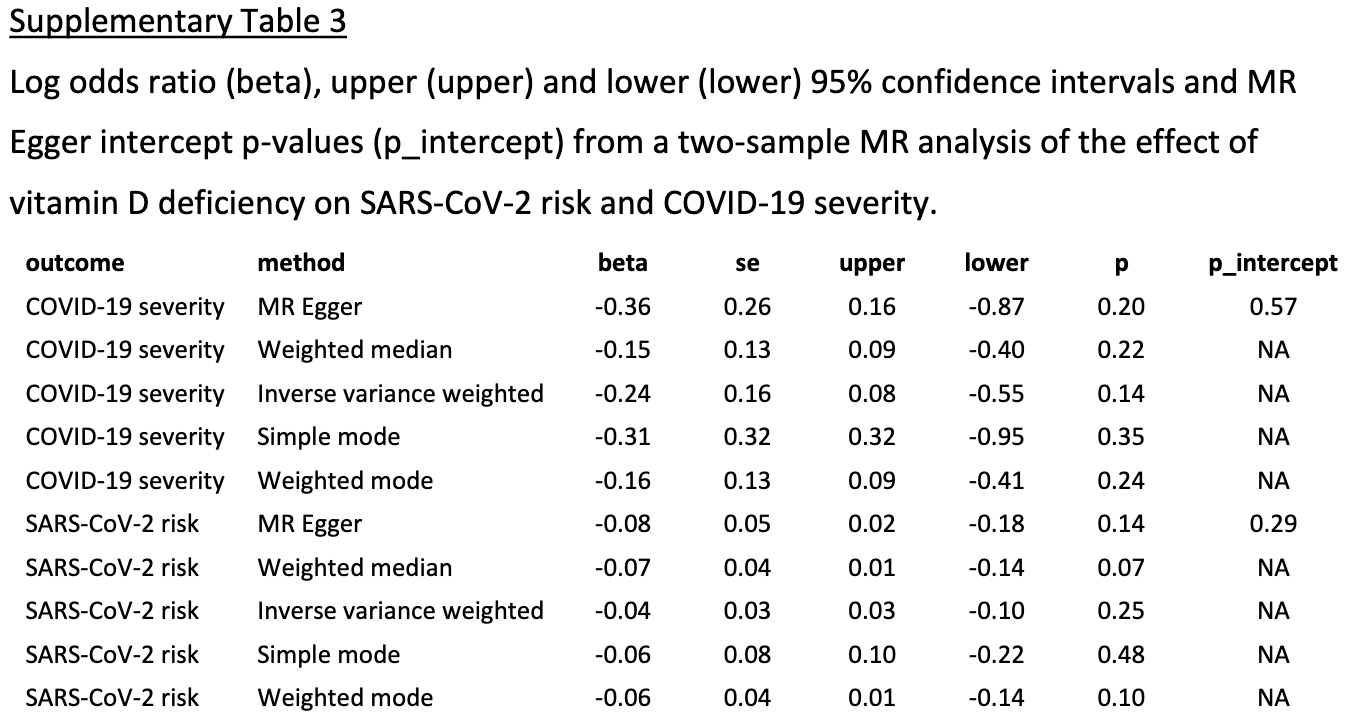 COVID-19 severity, 32.3% higher, RR 1.32, p = 0.20, OR converted to RR, >=50nmol/L vs. <25nmol/L, MR Egger, baseline risk approximated with overall risk. risk of case, 7.6% higher, RR 1.08, p = 0.14, OR converted to RR, >=50nmol/L vs. <25nmol/L, MR Egger, baseline risk approximated with overall risk. Amin et al., 1/7/2021, retrospective, population-based cohort, United Kingdom, Europe, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Nikniaz et al., medRxiv, doi:10.1101/2021.01.04.21249219 (Preprint) (meta analysis) | death, ↓67.5%, p=0.008 | The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis |
| Details Meta analysis of 4 supplementation studies, finding that vitamin D supplementation "seems to decrease the mortality rate, the severity of the disease, and serum levels of the inflammatory markers". Mortality odds ratio OR 0.264,.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Nikniaz et al., medRxiv, doi:10.1101/2021.01.04.21249219 (Preprint) (meta analysis) |
| The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis |
Meta analysis of 4 supplementation studies, finding that vitamin D supplementation "seems to decrease the mortality rate, the severity of the disease, and serum levels of the inflammatory markers". Mortality odds ratio OR 0.264, p = 0.008. 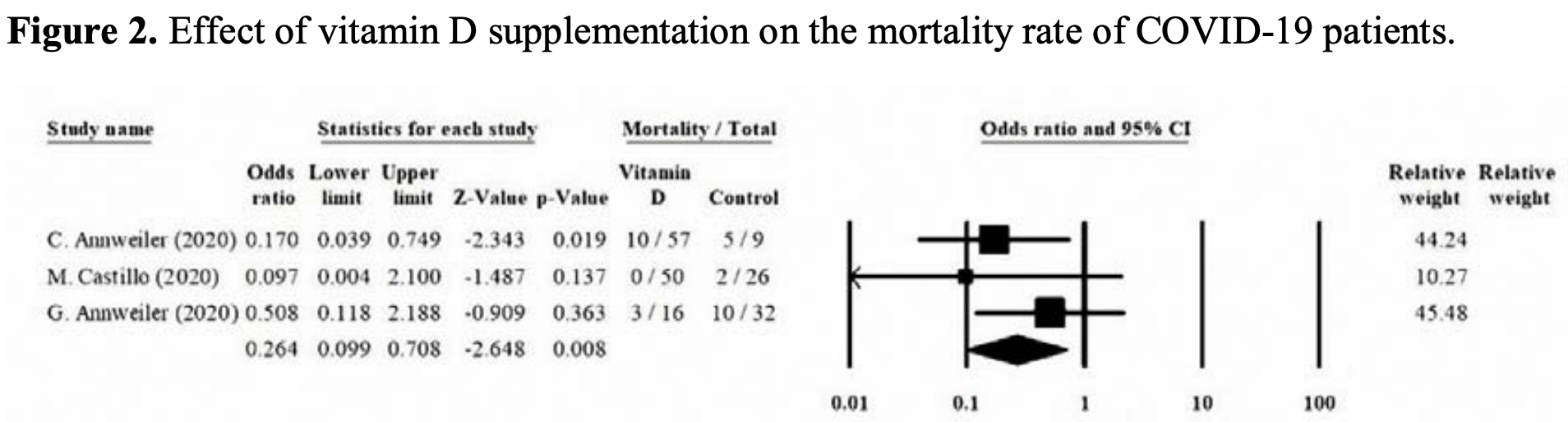 risk of death, 67.5% lower, RR 0.32, p = 0.008, treatment 13 of 123 (10.6%), control 17 of 67 (25.4%), OR converted to RR. Nikniaz et al., 1/5/2021, preprint, 4 authors. |
| Submit Corrections or Comments |
| Levels | Karonova et al., Infectology, doi:10.22625/2072-6732-2020-12-3-21-27 (Peer Reviewed) | death, ↓79.4%, p=0.11 | Serum 25(oH)D level in patients with CoVID-19 |
| Details Retrospective 80 COVID-19 patients showing low vitamin D levels associated with severity and mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Karonova et al., Infectology, doi:10.22625/2072-6732-2020-12-3-21-27 (Peer Reviewed) |
| Serum 25(oH)D level in patients with CoVID-19 |
Retrospective 80 COVID-19 patients showing low vitamin D levels associated with severity and mortality. 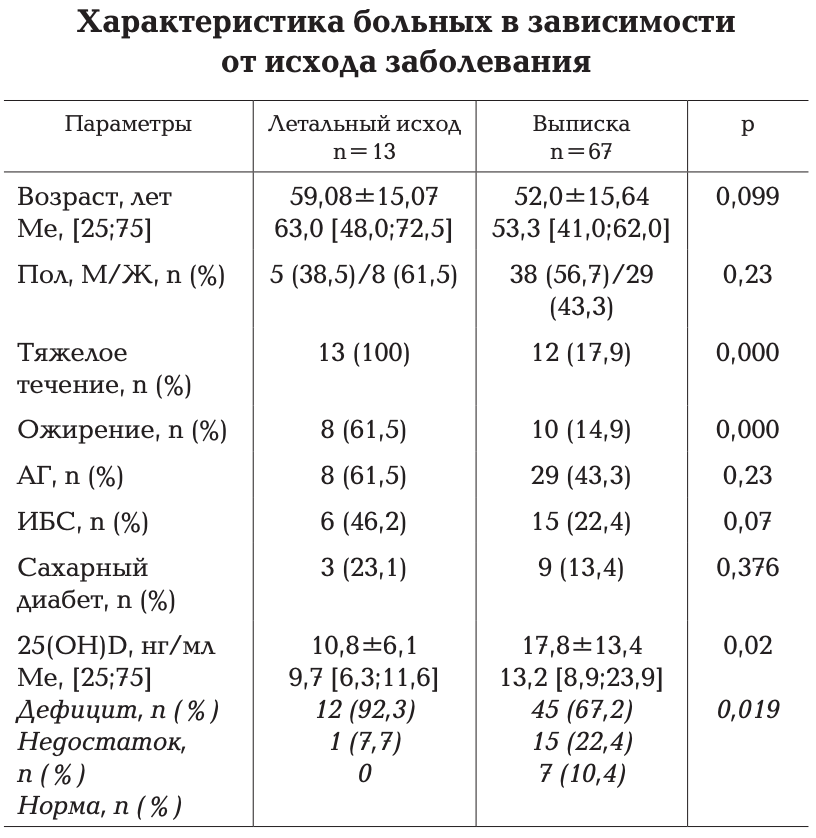 risk of death, 79.4% lower, RR 0.21, p = 0.11, high D levels 1 of 23 (4.3%), low D levels 12 of 57 (21.1%), OR converted to RR, >20ng/ml. risk of severe case, 71.1% lower, RR 0.29, p = 0.07, high D levels 3 of 23 (13.0%), low D levels 22 of 57 (38.6%), OR converted to RR, >20ng/ml. Karonova et al., 12/31/2020, retrospective, Russia, Europe, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Szeto et al., Endocrine Research, doi:10.1080/07435800.2020.1867162 (Peer Reviewed) | death, ↑5.6%, p=1.00 | Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients |
| Details Retrospective 93 hospitalized patients with vitamin D levels 1-365 days before admission, not showing significant differences with vitamin D deficiency or vitamin D levels. Vitamin D levels may vary significantly throughout the year creat.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Szeto et al., Endocrine Research, doi:10.1080/07435800.2020.1867162 (Peer Reviewed) |
| Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients |
Retrospective 93 hospitalized patients with vitamin D levels 1-365 days before admission, not showing significant differences with vitamin D deficiency or vitamin D levels. Vitamin D levels may vary significantly throughout the year creating a major cofounder that authors do not adjust for. 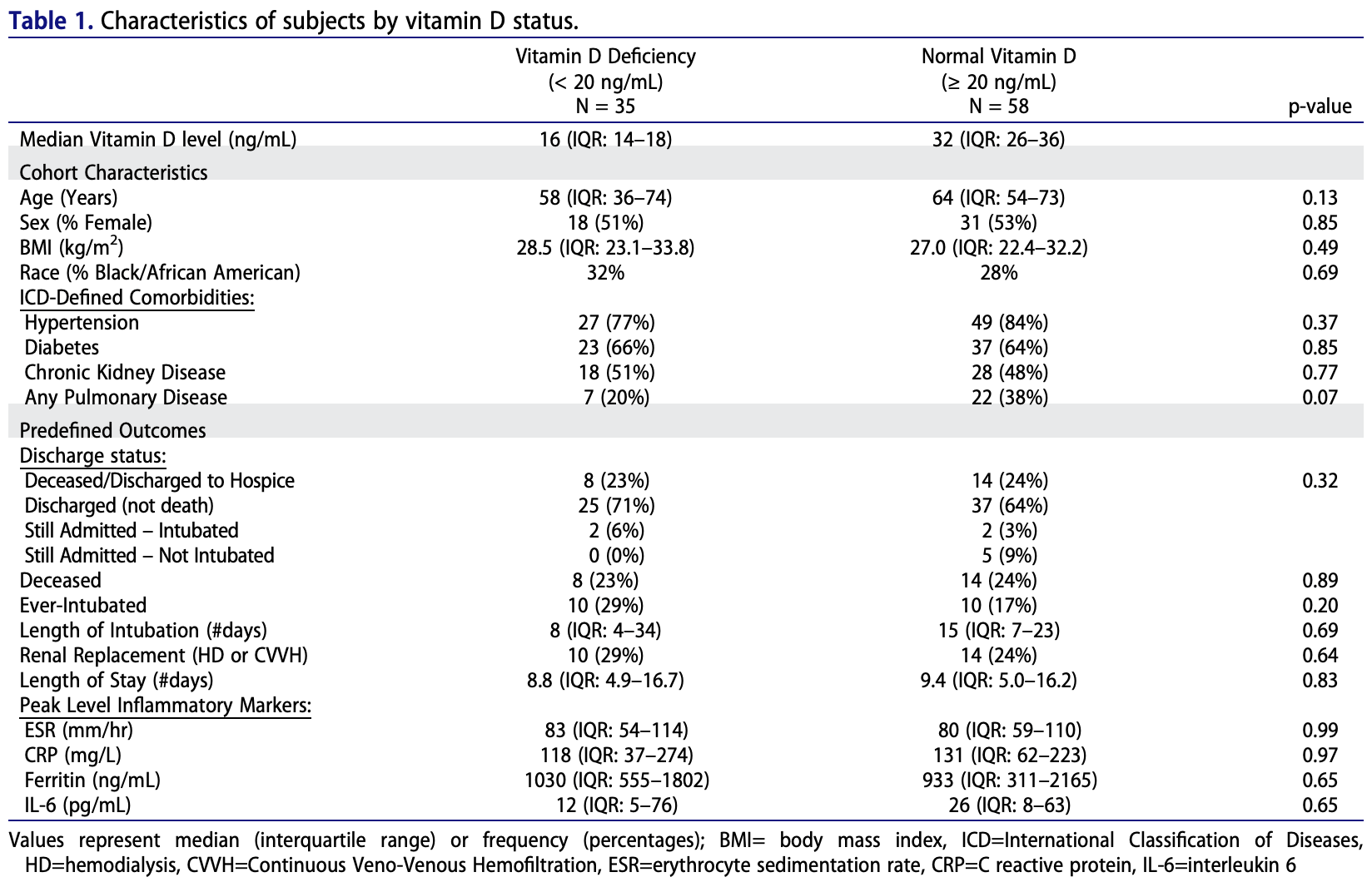 risk of death, 5.6% higher, RR 1.06, p = 1.00, high D levels 14 of 58 (24.1%), low D levels 8 of 35 (22.9%). risk of mechanical ventilation, 39.7% lower, RR 0.60, p = 0.21, high D levels 10 of 58 (17.2%), low D levels 10 of 35 (28.6%). risk of no hospital discharge, 26.7% higher, RR 1.27, p = 0.50, high D levels 21 of 58 (36.2%), low D levels 10 of 35 (28.6%). Szeto et al., 12/30/2020, retrospective, USA, North America, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Review | McCullough et al., Reviews in Cardiovascular Medicine, doi:10.31083/j.rcm.2020.04.264 (Review) (Peer Reviewed) | review | Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19) |
| Details Review urging early treatment of COVID-19 with sequential multidrug treatment that has been shown to be safe and effective. Proposed treatment includes zinc, vitamin D & C, quercetin, and depending on age, comorbidities, and symptoms may .. |
| Details Source PDF Review Review |
| McCullough et al., Reviews in Cardiovascular Medicine, doi:10.31083/j.rcm.2020.04.264 (Review) (Peer Reviewed) |
| Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19) |
| Review urging early treatment of COVID-19 with sequential multidrug treatment that has been shown to be safe and effective. Proposed treatment includes zinc, vitamin D & C, quercetin, and depending on age, comorbidities, and symptoms may include >=2 of HCQ, ivermectin, favipiravir; AZM/DOXY; corticosteroids; colchicine; bamlanivimab; aspirin; LMWH; and supplemental oxygen. McCullough et al., 12/30/2020, peer-reviewed, 58 authors. |
| Submit Corrections or Comments |
| Late | Jevalikar et al., Scientific Reports, doi:10.1038/s41598-021-85809-y (preprint 12/28) (Peer Reviewed) | death, ↓82.0%, p=0.12 | Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19 |
| Details Prospective study of 410 hospitalized patients in India showing lower mortality and ICU admission with cholecalciferol treatment, although not statistically significant with the small number of cases. The median total dose was 60000IU. N.. |
| Details Source PDF Late treatment study Late treatment study |
| Jevalikar et al., Scientific Reports, doi:10.1038/s41598-021-85809-y (preprint 12/28) (Peer Reviewed) |
| Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19 |
Prospective study of 410 hospitalized patients in India showing lower mortality and ICU admission with cholecalciferol treatment, although not statistically significant with the small number of cases. The median total dose was 60000IU.No significant difference was found for outcomes based on baseline vitamin D deficiency, however this analysis does not appear to account for the deficient patients that were treated with vitamin D. 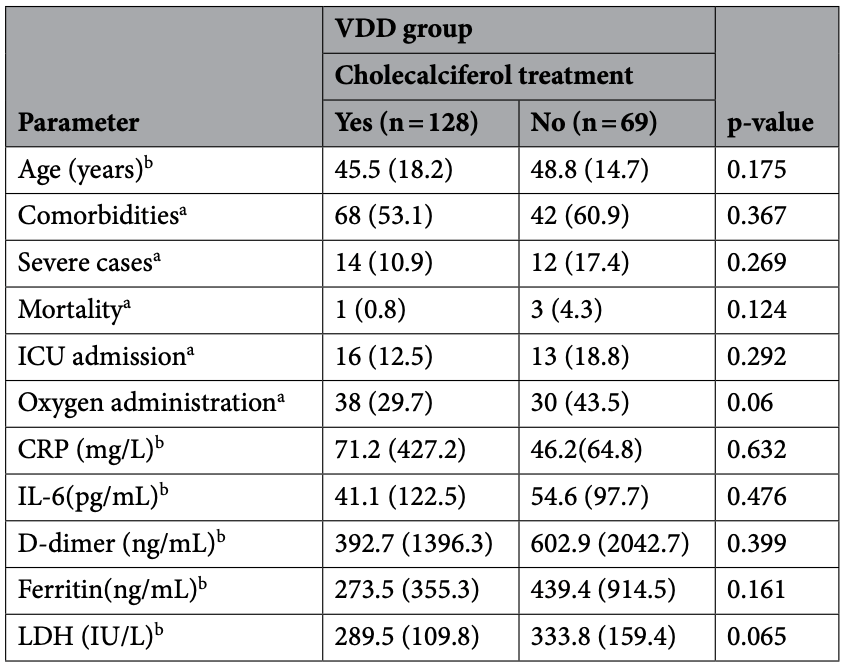 risk of death, 82.0% lower, RR 0.18, p = 0.12, treatment 1 of 128 (0.8%), control 3 of 69 (4.3%). risk of ICU admission, 33.7% lower, RR 0.66, p = 0.29, treatment 16 of 128 (12.5%), control 13 of 69 (18.8%). risk of oxygen therapy, 31.7% lower, RR 0.68, p = 0.06, treatment 38 of 128 (29.7%), control 30 of 69 (43.5%). Jevalikar et al., 12/28/2020, prospective, India, South Asia, peer-reviewed, 8 authors, dosage 60,000IU single dose, median total dose. |
| Submit Corrections or Comments |
| Late | Sistanizad et al., European Journal of Integrative Medicine, doi:10.1016/j.eujim.2020.101271 (Peer Reviewed) | death, ↓63.5%, p=0.004 | High dose vitamin D improves total serum antioxidant capacity and ICU outcome in critically ill patients - a randomized, double-blind clinical trial |
| Details RCT of 30 ventilated ICU patients showing lower mortality with vitamin D treatment, RR 0.36, p = 0.004. Authors do not indicate why the patients were hospitalized or if any of the patients were COVID-19 patients. 300,000 IU intramuscular .. |
| Details Source PDF Late treatment study Late treatment study |
| Sistanizad et al., European Journal of Integrative Medicine, doi:10.1016/j.eujim.2020.101271 (Peer Reviewed) |
| High dose vitamin D improves total serum antioxidant capacity and ICU outcome in critically ill patients - a randomized, double-blind clinical trial |
RCT of 30 ventilated ICU patients showing lower mortality with vitamin D treatment, RR 0.36, p = 0.004. Authors do not indicate why the patients were hospitalized or if any of the patients were COVID-19 patients. 300,000 IU intramuscular vitamin D was used. 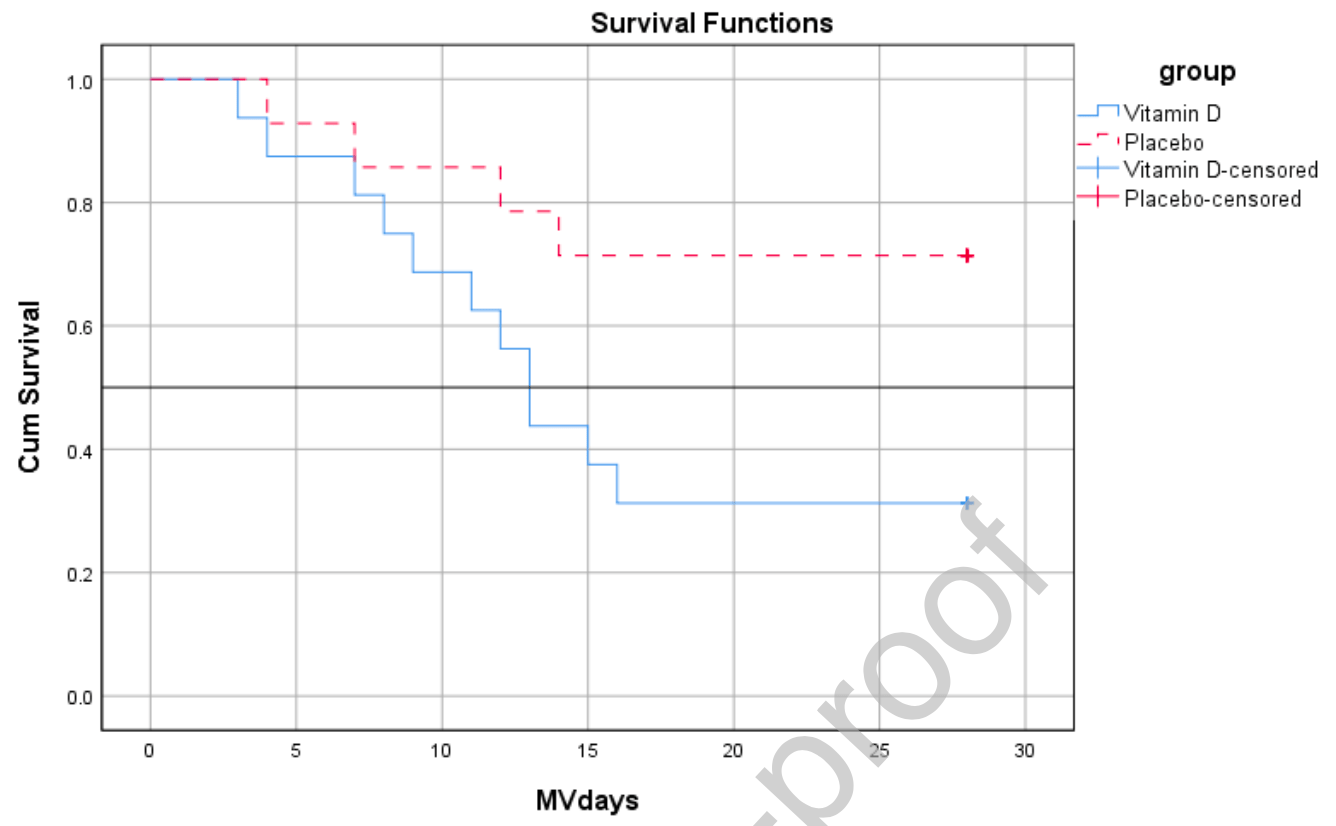 risk of death, 63.5% lower, RR 0.36, p = 0.004, treatment 5 of 16 (31.2%), control 12 of 14 (85.7%). Sistanizad et al., 12/26/2020, Randomized Controlled Trial, Iran, Middle East, peer-reviewed, 8 authors, dosage 300,000IU single dose, intramuscular. |
| Submit Corrections or Comments |
| PrEPPEP | Cangiano et al., Aging, doi:10.18632/aging.202307 (Peer Reviewed) | death, ↓70.0%, p=0.04 | Mortality in an Italian nursing home during COVID-19 pandemic: correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests |
| Details 70% lower mortality with vitamin D supplementation. Analysis of 98 PCR+ nursing home residents in Italy, mean age 90, vitamin D supplementation RR 0.30, p = 0.04. The paper provides the p value for regression but not the effect size. Trea.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Cangiano et al., Aging, doi:10.18632/aging.202307 (Peer Reviewed) |
| Mortality in an Italian nursing home during COVID-19 pandemic: correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests |
70% lower mortality with vitamin D supplementation. Analysis of 98 PCR+ nursing home residents in Italy, mean age 90, vitamin D supplementation RR 0.30, p = 0.04. The paper provides the p value for regression but not the effect size. Treatment was 2x per month 25000IU. 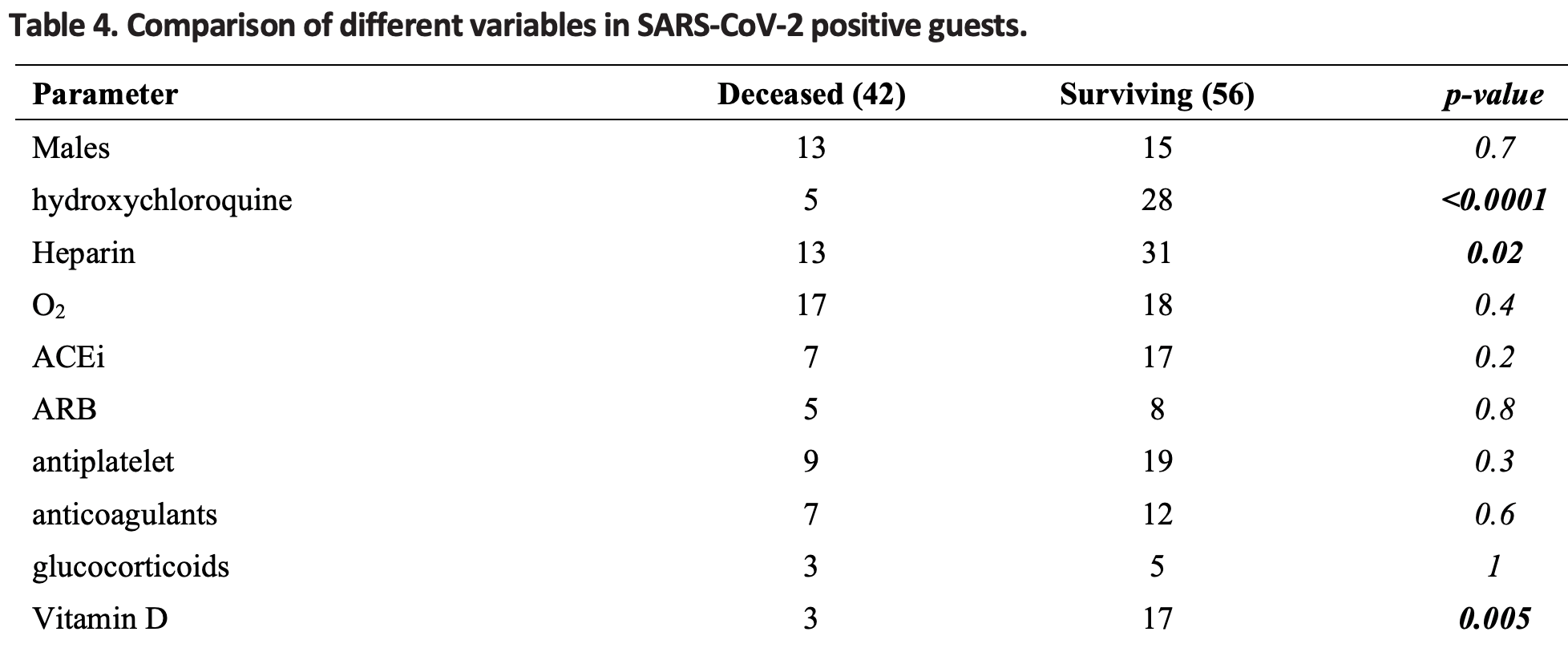 risk of death, 70.0% lower, RR 0.30, p = 0.04, treatment 3 of 20 (15.0%), control 39 of 78 (50.0%). Cangiano et al., 12/22/2020, retrospective, Italy, Europe, peer-reviewed, 14 authors, dosage 25,000IU 2x per month. |
| Submit Corrections or Comments |
| Levels | Abdollahi et al., Journal of Medical Virology, doi:10.1002/jmv.26726 (Peer Reviewed) | cases, ↓53.9%, p=0.001 | The Association Between the Level of Serum 25(OH) Vitamin D, Obesity, and underlying Diseases with the risk of Developing COVID‐19 Infection: A case‐control study of hospitalized patients in Tehran, Iran |
| Details Case control study with 201 patients and 201 matched controls in Iran showing vitamin D deficiency associated with COVID-19. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Abdollahi et al., Journal of Medical Virology, doi:10.1002/jmv.26726 (Peer Reviewed) |
| The Association Between the Level of Serum 25(OH) Vitamin D, Obesity, and underlying Diseases with the risk of Developing COVID‐19 Infection: A case‐control study of hospitalized patients in Tehran, Iran |
Case control study with 201 patients and 201 matched controls in Iran showing vitamin D deficiency associated with COVID-19. 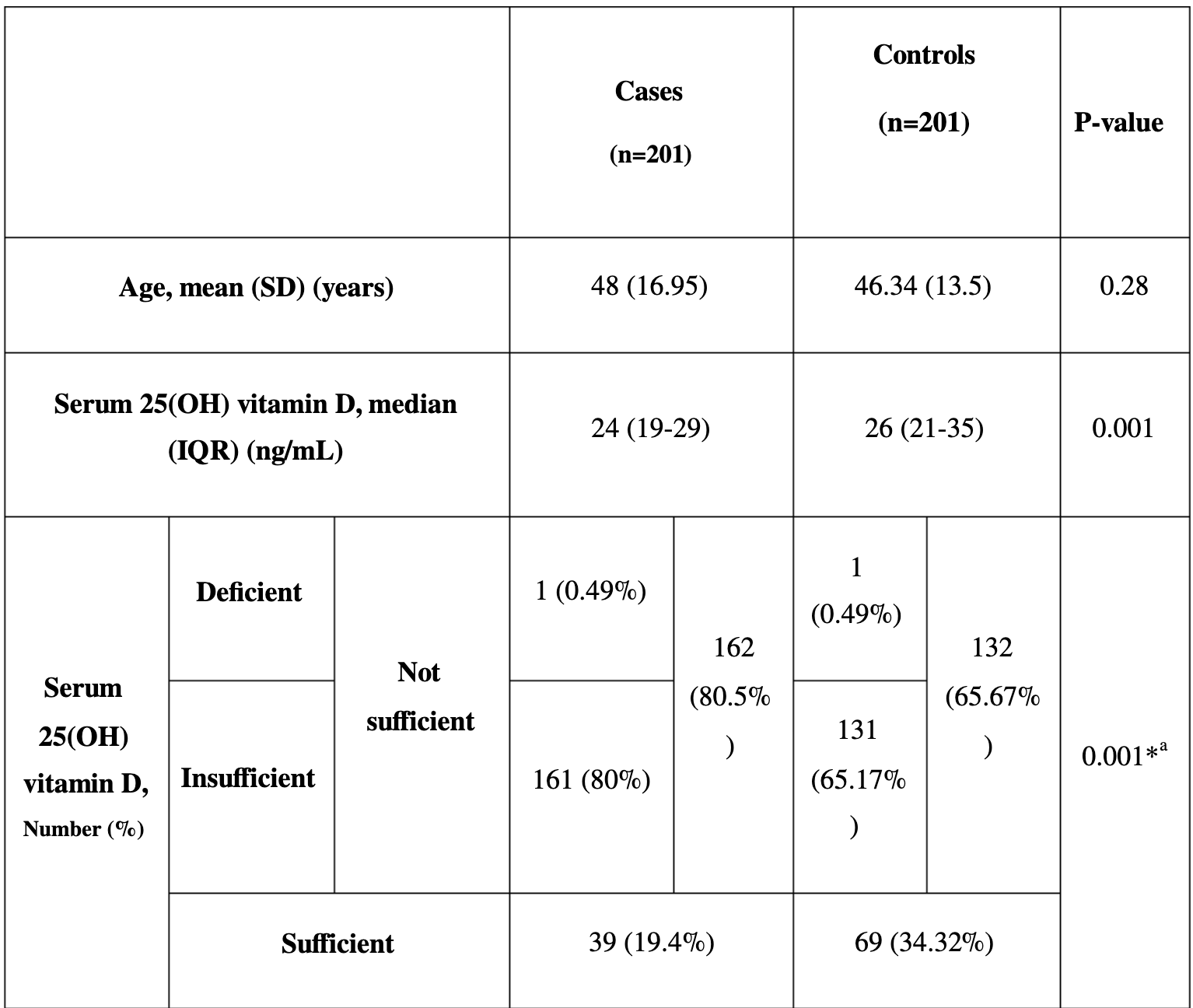 risk of case, 53.9% lower, RR 0.46, p = 0.001, high D levels 108, low D levels 294, >30ng/ml. Abdollahi et al., 12/12/2020, retrospective, Iran, Middle East, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Late | Ling et el., Nutrients, doi:10.3390/nu12123799 (Peer Reviewed) | death, ↓79.8%, p<0.001 | High-Dose Cholecalciferol Booster Therapy is Associated with a Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study |
| Details 80% lower mortality with cholecalciferol booster therapy. Retrospective 986 hospitalized patients in the UK finding that cholecalciferol booster therapy, regardless of baseline serum levels, was associated with a reduced risk of mortality.. |
| Details Source PDF Late treatment study Late treatment study |
| Ling et el., Nutrients, doi:10.3390/nu12123799 (Peer Reviewed) |
| High-Dose Cholecalciferol Booster Therapy is Associated with a Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study |
80% lower mortality with cholecalciferol booster therapy. Retrospective 986 hospitalized patients in the UK finding that cholecalciferol booster therapy, regardless of baseline serum levels, was associated with a reduced risk of mortality in acute COVID-19 inpatients.Primary cohort of 444 patients, adjusted mortality odds ratio aOR 0.13, p < 0.001.
Validation cohort of 541 patients, adjusted mortality odds ratio aOR 0.38, p = 0.018. 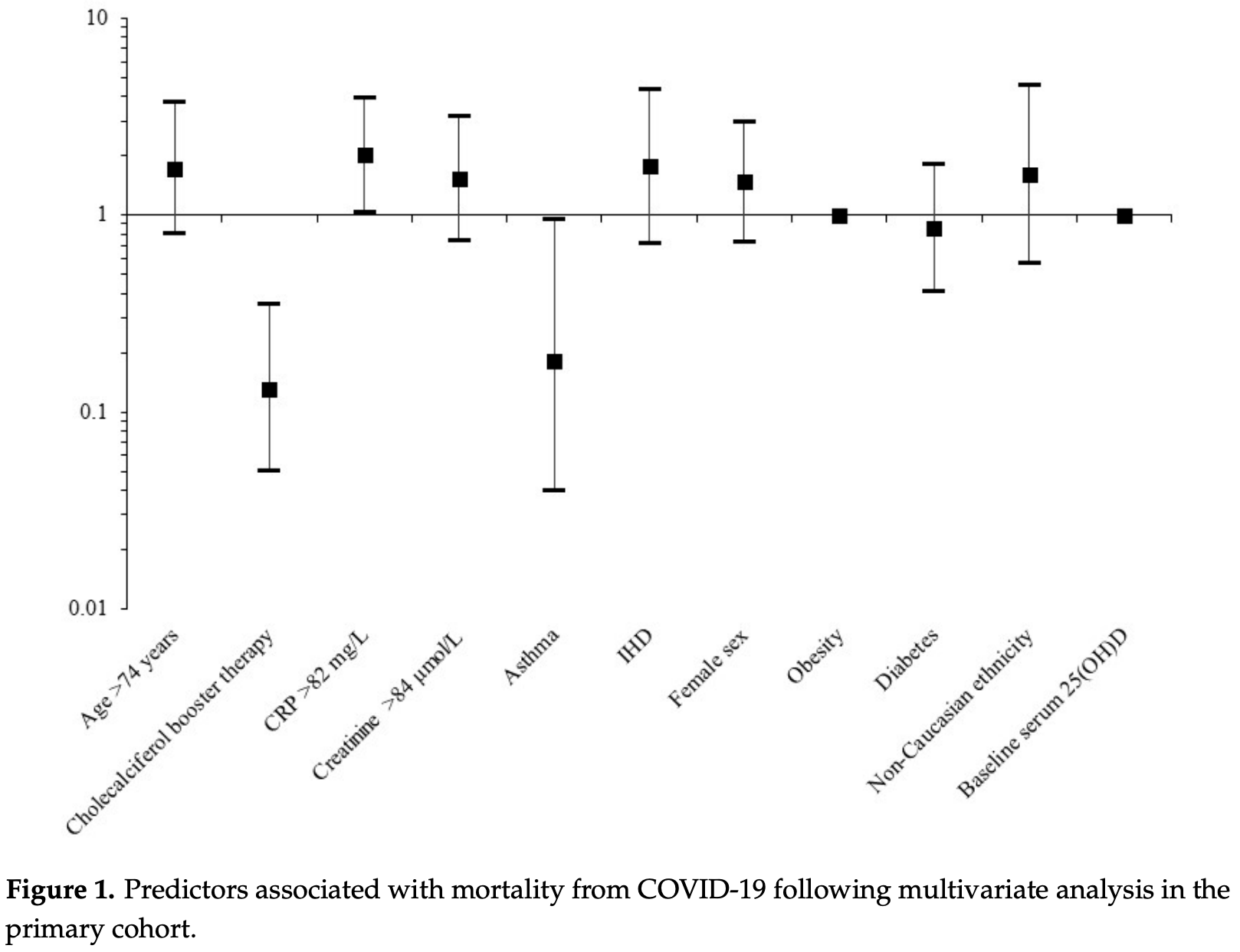 risk of death, 79.8% lower, RR 0.20, p < 0.001, treatment 73, control 253, OR converted to RR, primary cohort. risk of death, 55.5% lower, RR 0.44, p = 0.02, treatment 80, control 443, OR converted to RR, validation cohort. Ling et al., 12/11/2020, retrospective, United Kingdom, Europe, peer-reviewed, 7 authors, dosage 40,000IU weekly, regimen varied with 77% receiving a total of 40,000IU/week. |
| Submit Corrections or Comments |
| News | VitaminDForAll (News) | news | Over 100 Scientists, Doctors, & Leading Authorities Call For Increased Vitamin D Use To Combat COVID-19 |
| Details Over 100 scientists and doctors call for efforts to increase vitamin D levels. Recommendations include reaching 75 nmol/L serum levels, 2000-4000IU daily supplementation (in the absence of testing), and measurement and treatment in hospit.. |
| Details Source PDF News News |
| VitaminDForAll (News) |
| Over 100 Scientists, Doctors, & Leading Authorities Call For Increased Vitamin D Use To Combat COVID-19 |
Over 100 scientists and doctors call for efforts to increase vitamin D levels. Recommendations include reaching 75 nmol/L serum levels, 2000-4000IU daily supplementation (in the absence of testing), and measurement and treatment in hospitalized patients. 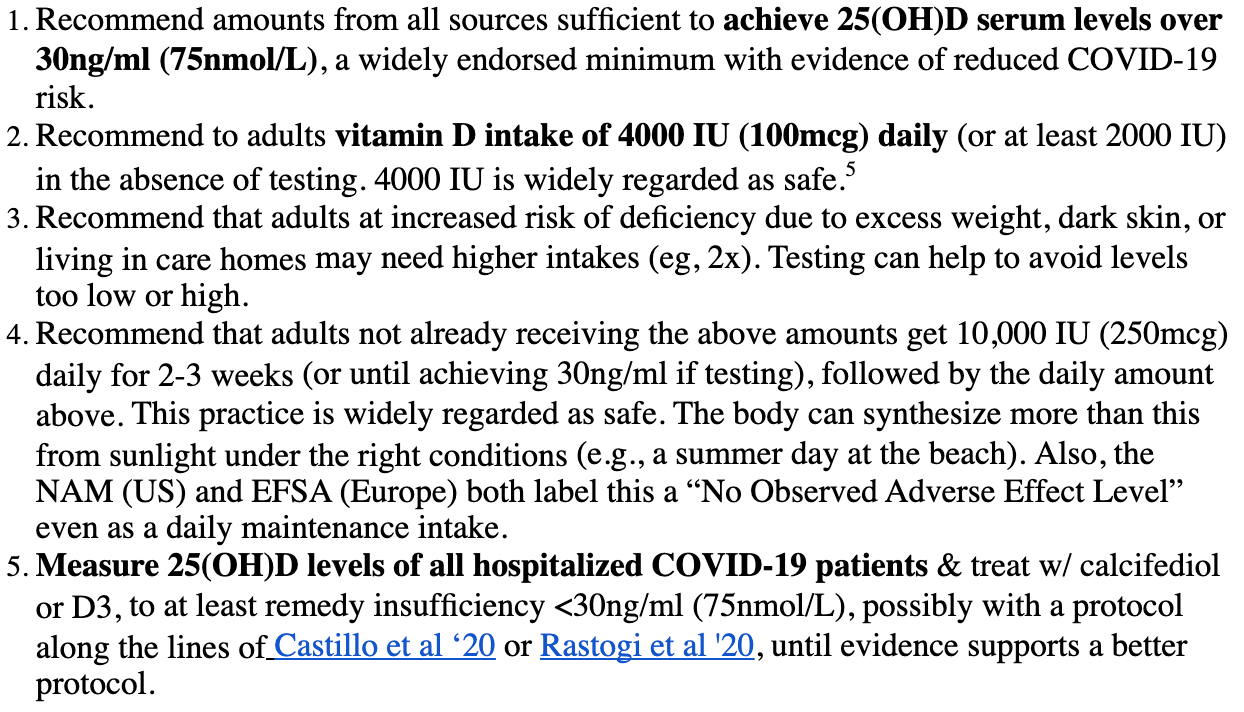 VitaminDForAll et al., 12/10/2020, preprint, 2 authors. |
| Submit Corrections or Comments |
| Levels | Vassiliou et al., Hellenic Journal of Cardiology, doi:10.1016/j.hjc.2020.11.011 (Peer Reviewed) | Vitamin D deficiency correlates with a reduced number of natural killer cells in intensive care unit (ICU) and non-ICU patients with COVID-19 pneumonia |
| Details Observational study of 29 ICU patients and 10 non-ICU patients showing vitamin D levels positively correlated with cytotoxic T cells, natural killer (NK) cells, NK-T cells, and regulatory T cells. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Vassiliou et al., Hellenic Journal of Cardiology, doi:10.1016/j.hjc.2020.11.011 (Peer Reviewed) |
| Vitamin D deficiency correlates with a reduced number of natural killer cells in intensive care unit (ICU) and non-ICU patients with COVID-19 pneumonia |
Observational study of 29 ICU patients and 10 non-ICU patients showing vitamin D levels positively correlated with cytotoxic T cells, natural killer (NK) cells, NK-T cells, and regulatory T cells. 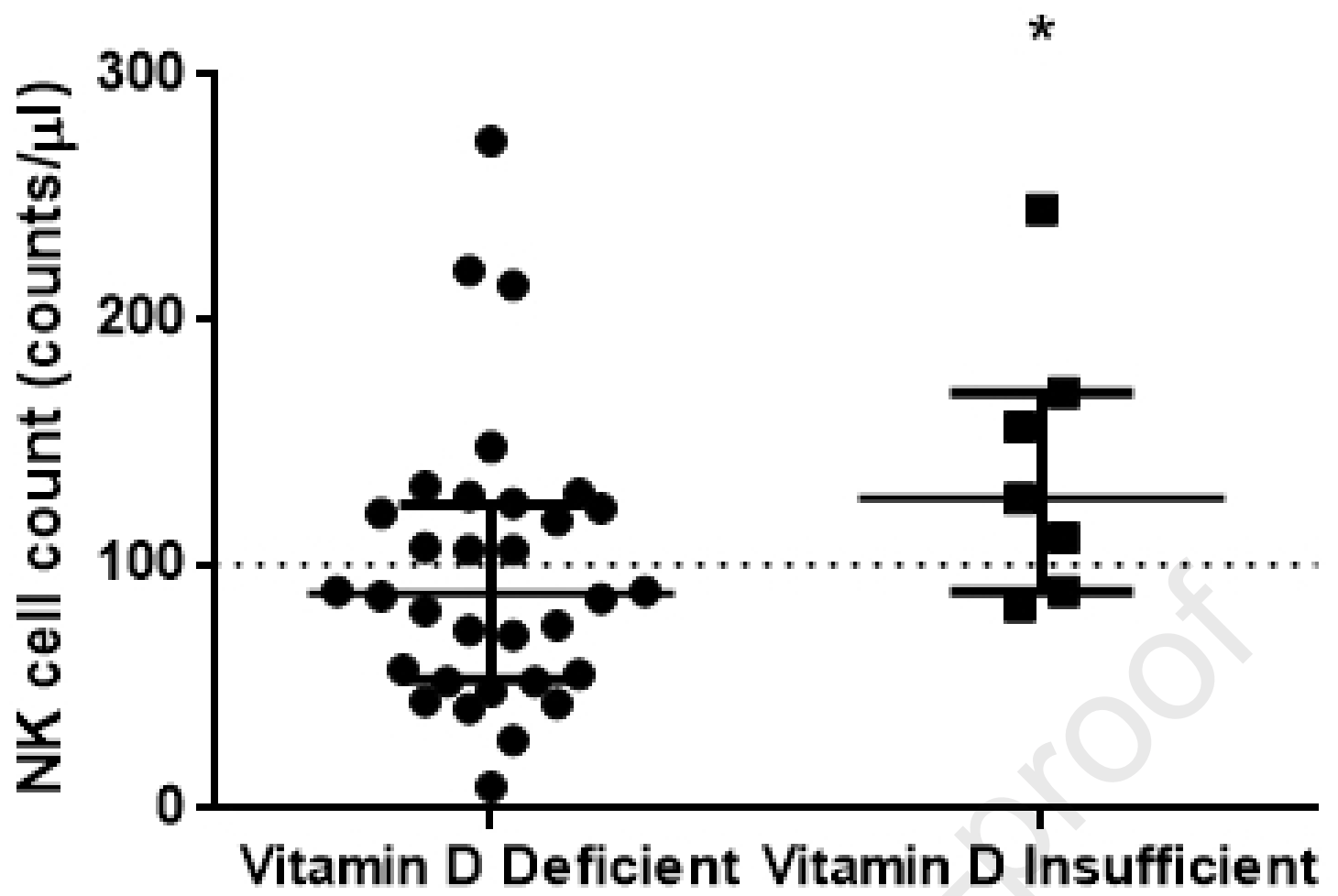 Vassiliou et al., 12/9/2020, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Vassiliou et al., Nutrients, doi:10.3390/nu12123773 (Peer Reviewed) | death, ↓90.9%, p=0.04 | Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort |
| Details Small prospective study of 30 ICU patients, showing higher mortality risk for low vitamin D levels. When divided into two groups at the median level, there was 5 of 15 deaths for the low vitamin D group compared to 0 of 15 in the high vit.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Vassiliou et al., Nutrients, doi:10.3390/nu12123773 (Peer Reviewed) |
| Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort |
Small prospective study of 30 ICU patients, showing higher mortality risk for low vitamin D levels. When divided into two groups at the median level, there was 5 of 15 deaths for the low vitamin D group compared to 0 of 15 in the high vitamin D group. 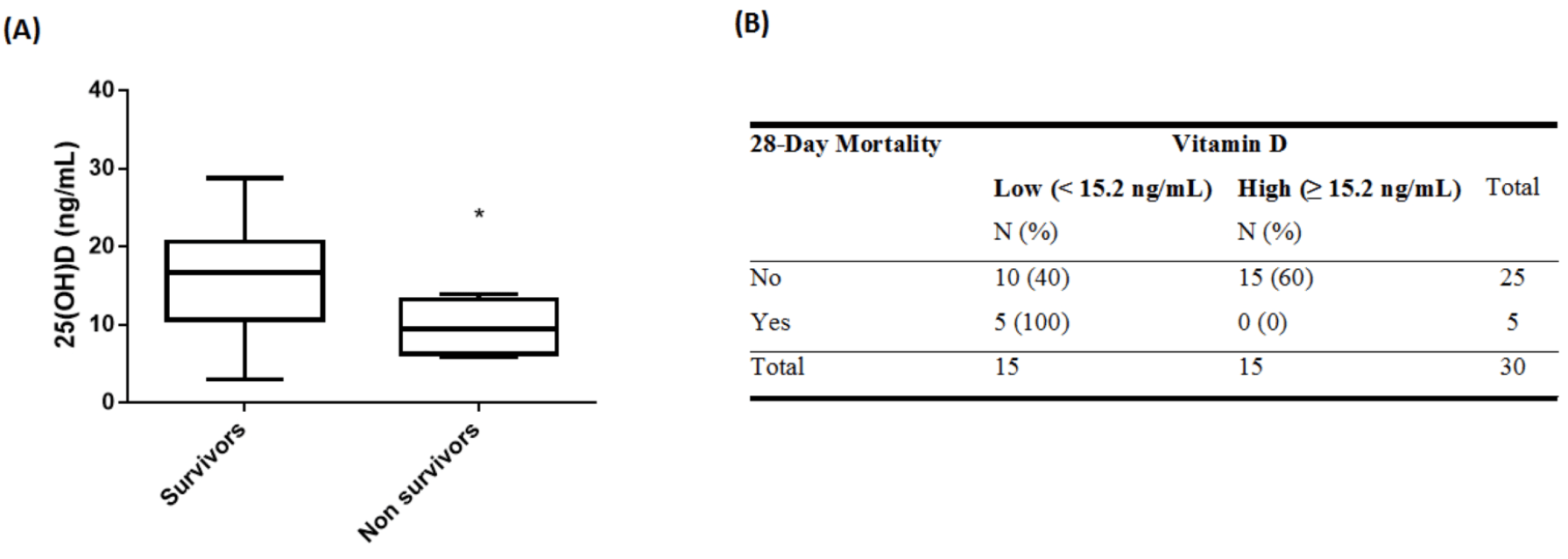 risk of death, 90.9% lower, RR 0.09, p = 0.04, high D levels 0 of 15 (0.0%), low D levels 5 of 15 (33.3%), relative risk is not 0 because of continuity correction due to zero events, >15.2ng/mL. Vassiliou et al., 12/9/2020, prospective, Greece, Europe, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Alguwaihes et al., Cardiovascular Diabetology, doi:10.1186/s12933-020-01184-4 (Peer Reviewed) | death, ↓85.7%, p=0.007 | Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study |
| Details Retrospective 439 diabetic hospitalized patients in Saudi Arabia showing lower mortality with vitamin D >12.5 nmol/L, adjusted hazard ratio aHR 0.14, p = 0.007. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Alguwaihes et al., Cardiovascular Diabetology, doi:10.1186/s12933-020-01184-4 (Peer Reviewed) |
| Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study |
Retrospective 439 diabetic hospitalized patients in Saudi Arabia showing lower mortality with vitamin D >12.5 nmol/L, adjusted hazard ratio aHR 0.14, p = 0.007. 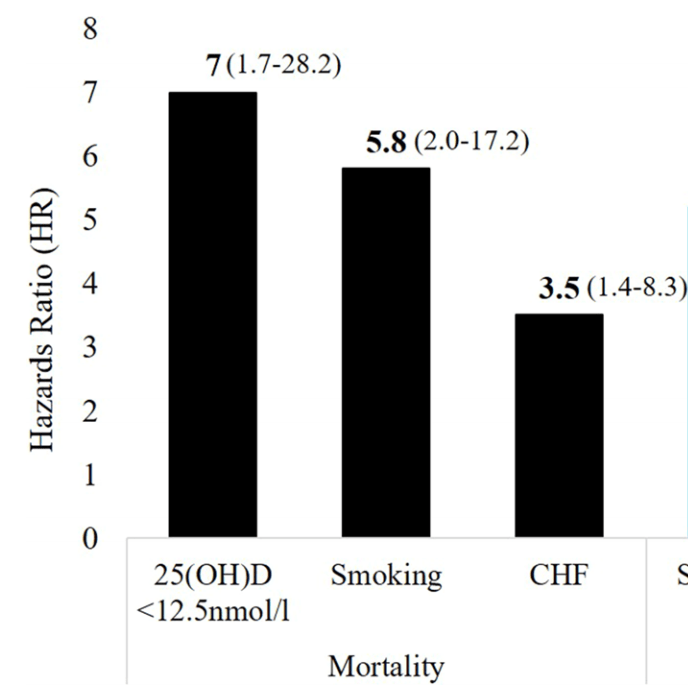 risk of death, 85.7% lower, RR 0.14, p = 0.007, high D levels 111, low D levels 328, >12.5 nmol/L. Alguwaihes et al., 12/5/2020, retrospective, Saudi Arabia, Middle East, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Levels | Katz el al., Nutrition, doi:10.1016/j.nut.2020.111106 (Peer Reviewed) | cases, ↓78.4%, p<0.001 | Increased risk for Covid-19 in patients with Vitamin D deficiency |
| Details Retrospective database analysis showing patients with vitamin D deficiency were 4.6 times more likely to be COVID-19 positive, p<0.001. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Katz el al., Nutrition, doi:10.1016/j.nut.2020.111106 (Peer Reviewed) |
| Increased risk for Covid-19 in patients with Vitamin D deficiency |
Retrospective database analysis showing patients with vitamin D deficiency were 4.6 times more likely to be COVID-19 positive, p<0.001. 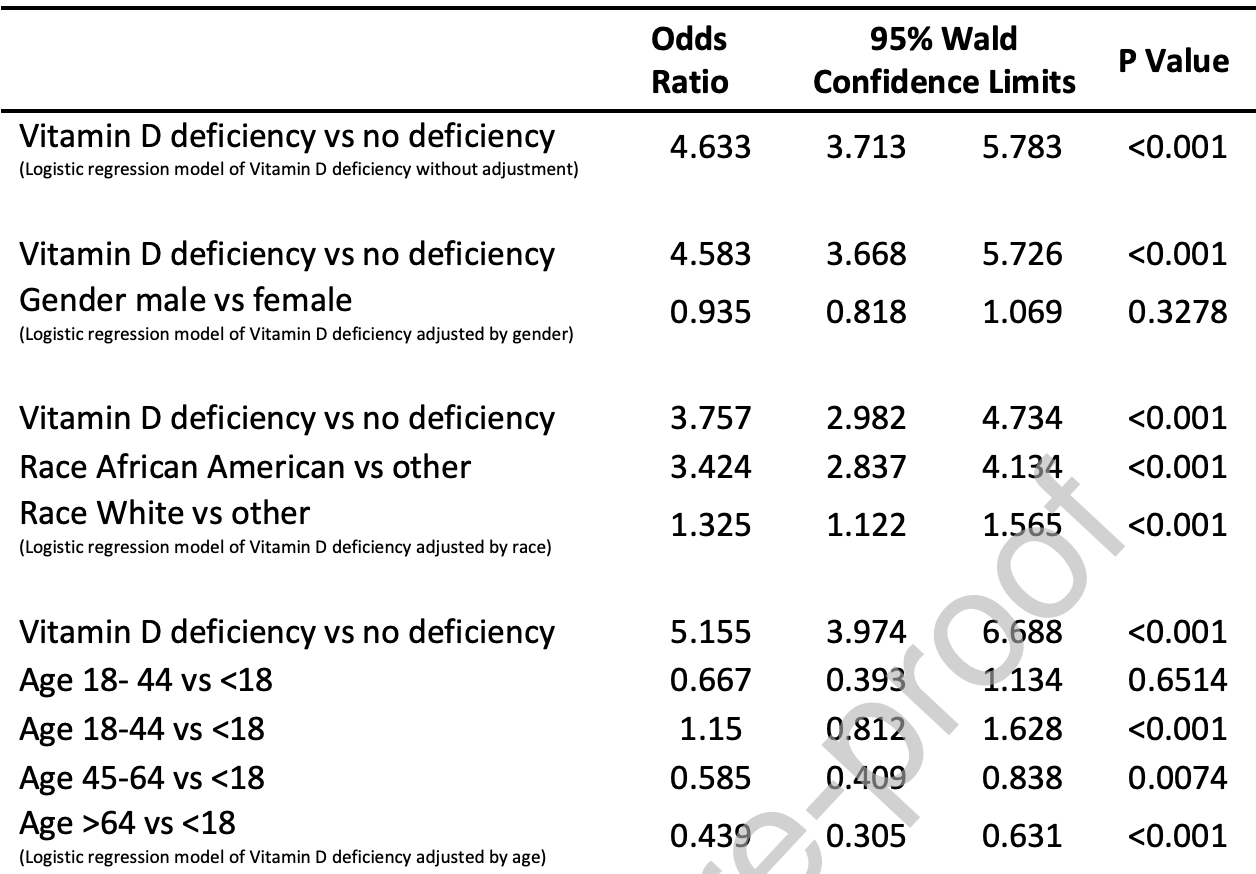 risk of case, 78.4% lower, RR 0.22, p < 0.001, adjusted. Katz et al., 12/4/2020, retrospective, population-based cohort, USA, North America, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Louca et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000250 (preprint 11/30/20) (Peer Reviewed) | cases, ↓7.5%, p=0.0007 | Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 Symptom Study app |
| Details Survey analysis of dietary supplements showing vitamin D usage associated with lower incidence of COVID-19. These results are for PCR+ cases only, they do not reflect potential benefits for reducing the severity of cases. A number of bias.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Louca et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000250 (preprint 11/30/20) (Peer Reviewed) |
| Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 Symptom Study app |
Survey analysis of dietary supplements showing vitamin D usage associated with lower incidence of COVID-19. These results are for PCR+ cases only, they do not reflect potential benefits for reducing the severity of cases. A number of biases could affect the results, for example users of the app may not be representative of the general population, and people experiencing symptoms may be more likely to install and use the app. 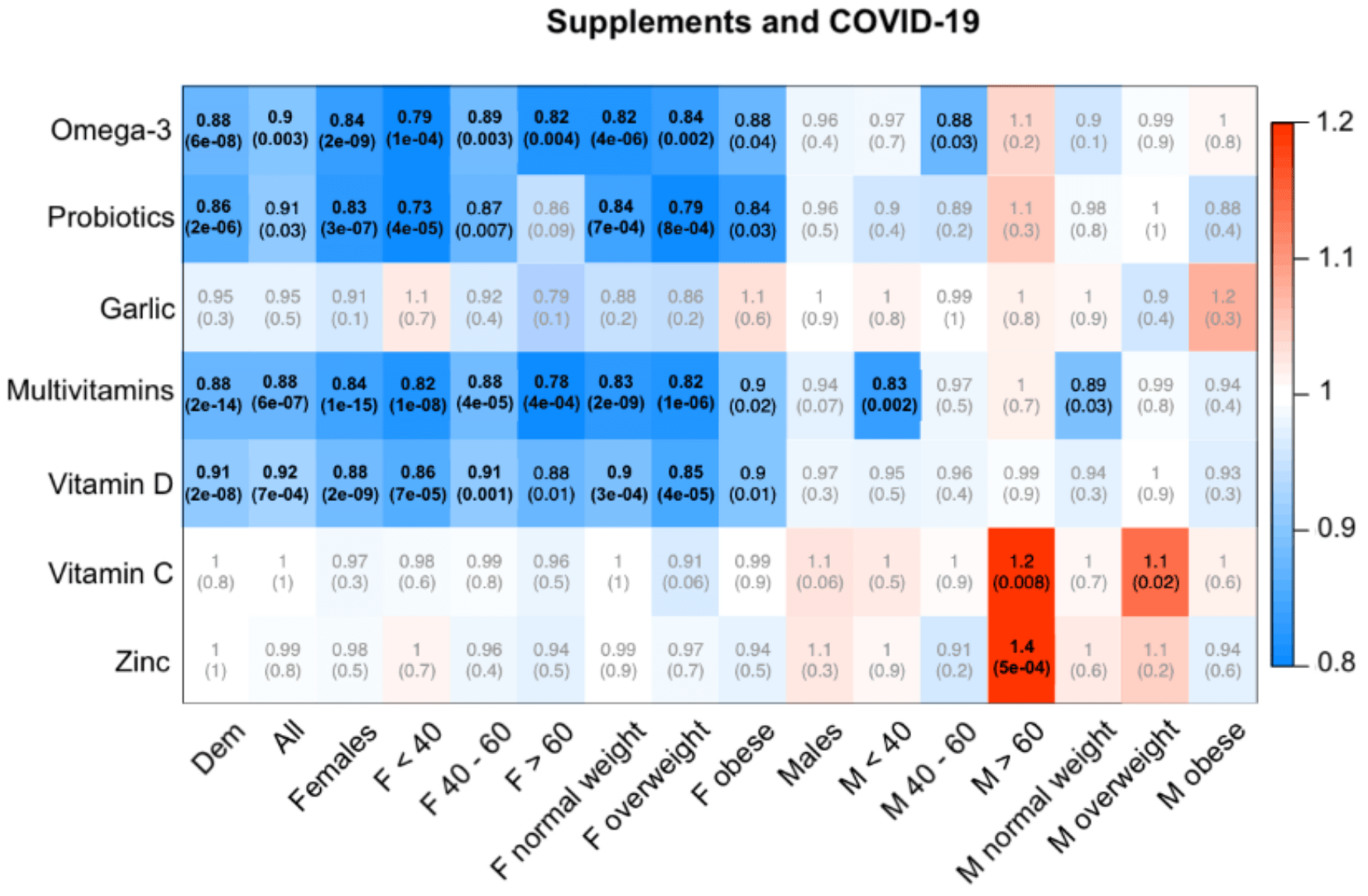 risk of case, 7.5% lower, RR 0.92, p < 0.001, OR converted to RR, United Kingdom, all adjustment model. Louca et al., 11/30/2020, retrospective, population-based cohort, United Kingdom, Europe, peer-reviewed, 26 authors, dosage not specified. |
| Submit Corrections or Comments |
| Levels | De Smet et al., American Journal of Clinical Pathology, doi:10.1093/ajcp/aqaa252 (Peer Reviewed) | death, ↓70.1%, p=0.02 | Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality |
| Details Retrospective 186 hospitalized patients in Belgium showing that 59% of patients were vitamin D deficient, and that non-vitamin D deficient patients had significantly lower mortality risk, RR 0.26, p = 0.015. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| De Smet et al., American Journal of Clinical Pathology, doi:10.1093/ajcp/aqaa252 (Peer Reviewed) |
| Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality |
Retrospective 186 hospitalized patients in Belgium showing that 59% of patients were vitamin D deficient, and that non-vitamin D deficient patients had significantly lower mortality risk, RR 0.26, p = 0.015. 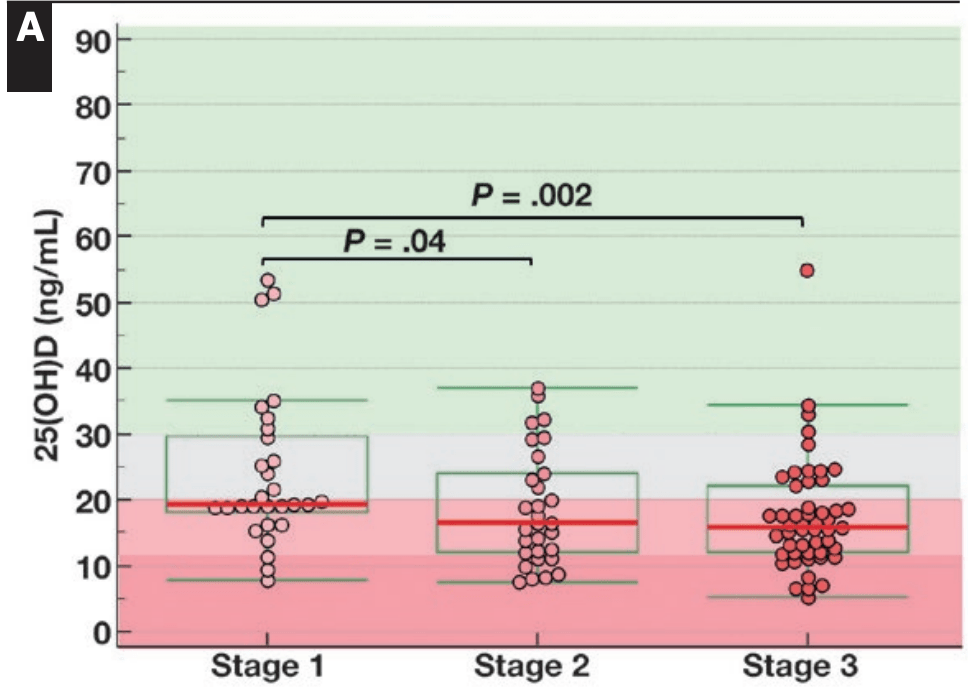 risk of death, 70.1% lower, RR 0.30, p = 0.02, high D levels 7 of 77 (9.1%), low D levels 20 of 109 (18.3%), adjusted, OR converted to RR, >20ng/mL. De Smet et al., 11/25/2020, retrospective, Belgium, Europe, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Levels | Jain et al., Nature, doi:10.1038/s41598-020-77093-z (Peer Reviewed) | death, ↓85.2%, p=0.001 | Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers |
| Details Prospective study of 91 asymptomatic and 63 ICU patients showing significantly higher vitamin D deficiency in the ICU patients (97% vs. 33%). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Jain et al., Nature, doi:10.1038/s41598-020-77093-z (Peer Reviewed) |
| Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers |
Prospective study of 91 asymptomatic and 63 ICU patients showing significantly higher vitamin D deficiency in the ICU patients (97% vs. 33%). 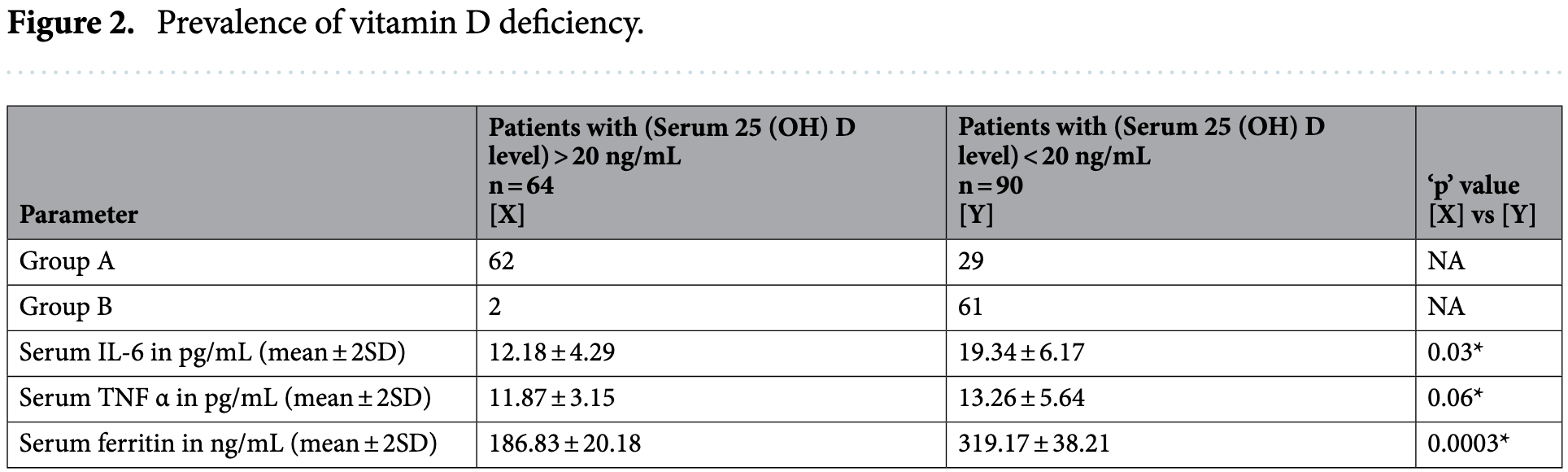 risk of death, 85.2% lower, RR 0.15, p = 0.001, high D levels 2 of 64 (3.1%), low D levels 19 of 90 (21.1%), >20ng/mL. risk of ICU admission, 95.4% lower, RR 0.05, p < 0.001, high D levels 2 of 64 (3.1%), low D levels 61 of 90 (67.8%), >20ng/mL. Jain et al., 11/19/2020, prospective, India, South Asia, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Late | Murai et al., JAMA, doi:10.1001/jama.2020.26848 (preprint 11/17) (Peer Reviewed) | death, ↑48.7%, p=0.43 | Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial |
| Details Very late stage (mean 10 days from symptom onset, 90% on oxygen at baseline) vitamin D supplementation RCT not showing significant differences. Ethnicity was poorly matched between arms, and diabetes was 41% in the treatment arm vs. 29% .. |
| Details Source PDF Late treatment study Late treatment study |
| Murai et al., JAMA, doi:10.1001/jama.2020.26848 (preprint 11/17) (Peer Reviewed) |
| Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial |
Very late stage (mean 10 days from symptom onset, 90% on oxygen at baseline) vitamin D supplementation RCT not showing significant differences.Ethnicity was poorly matched between arms, and diabetes was 41% in the treatment arm vs. 29% in the control arm. Baseline ventilation was 15% in the treatment arm vs. 12% control, this alone may account for the higher mortality. Calcifediol or calcitriol, which avoids several days delay in conversion, may be more successful, especially with this very late stage usage. 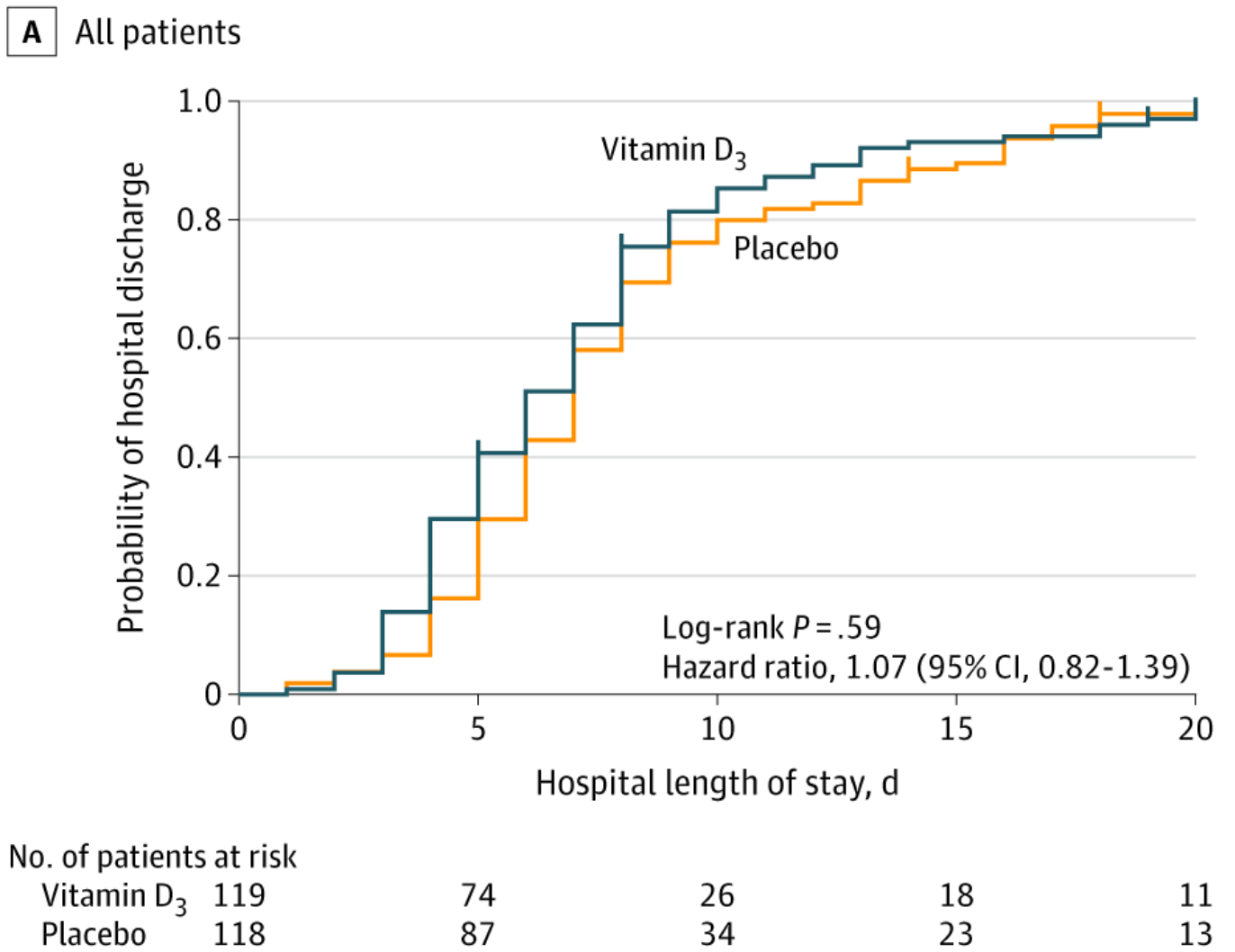 risk of death, 48.7% higher, RR 1.49, p = 0.43, treatment 9 of 119 (7.6%), control 6 of 118 (5.1%). risk of mechanical ventilation, 47.5% lower, RR 0.52, p = 0.09, treatment 9 of 119 (7.6%), control 17 of 118 (14.4%). risk of ICU admission, 24.6% lower, RR 0.75, p = 0.30, treatment 19 of 119 (16.0%), control 25 of 118 (21.2%). Excluded in after exclusion results of meta analysis: very late stage, >50% on oxygen/ventilation at baseline. Murai et al., 11/17/2020, Double Blind Randomized Controlled Trial, Brazil, South America, peer-reviewed, 17 authors, dosage 200,000IU single dose. |
| Submit Corrections or Comments |
| Levels | Luo et al., The Journal of Nutrition, doi:10.1093/jn/nxaa332 (Peer Reviewed) | progression, ↓63.0%, p=0.01 | Vitamin D Deficiency Is Inversely Associated with COVID-19 Incidence and Disease Severity in Chinese People |
| Details Retrospective 335 patients in China compared to 560 matched controls showing significanlty lower risk of severe COVID-19 with vitamin D sufficiency (>=30 nmol/L) OR 0.37, p = 0.014. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Luo et al., The Journal of Nutrition, doi:10.1093/jn/nxaa332 (Peer Reviewed) |
| Vitamin D Deficiency Is Inversely Associated with COVID-19 Incidence and Disease Severity in Chinese People |
Retrospective 335 patients in China compared to 560 matched controls showing significanlty lower risk of severe COVID-19 with vitamin D sufficiency (>=30 nmol/L) OR 0.37, p = 0.014. risk of disease progression, 63.0% lower, RR 0.37, p = 0.01, high D levels 335, low D levels 560, >30nmol/L. Luo et al., 11/13/2020, retrospective, China, Asia, peer-reviewed, median age 56.0, 5 authors. |
| Submit Corrections or Comments |
| Meta | Jungreis et al., medRxiv, doi:10.1101/2020.11.08.20222638 (Preprint) | Mathematical analysis of Córdoba calcifediol trial suggests strong role for Vitamin D in reducing ICU admissions of hospitalized COVID-19 patients |
| Details Analysis of Castillo et al. confirming efficacy of calcifediol treatment. Authors find that issues related to imperfect blinding and comorbidities can not explain the result found. See [1] for a response to issues raised on this analysis. |
| Details Source PDF Meta Meta |
| Jungreis et al., medRxiv, doi:10.1101/2020.11.08.20222638 (Preprint) |
| Mathematical analysis of Córdoba calcifediol trial suggests strong role for Vitamin D in reducing ICU admissions of hospitalized COVID-19 patients |
| Analysis of Castillo et al. confirming efficacy of calcifediol treatment. Authors find that issues related to imperfect blinding and comorbidities can not explain the result found.See [1] for a response to issues raised on this analysis. Jungreis et al., 11/12/2020, preprint, 2 authors. |
| Submit Corrections or Comments |
| Late | Rastogi et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-139065 (Peer Reviewed) | viral+, ↓52.6%, p=0.02 | Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study) |
| Details 53% reduction in PCR+ with high-dose cholecalciferol supplementation. RCT with 16 treatment patients and 24 control patients. Relative risk of PCR+ at 2 weeks with treatment, RR 0.47, p=0.18 25(OH)D levels at day 14 were 52 ng/ml vs. 15.. |
| Details Source PDF Late treatment study Late treatment study |
| Rastogi et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-139065 (Peer Reviewed) |
| Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study) |
53% reduction in PCR+ with high-dose cholecalciferol supplementation. RCT with 16 treatment patients and 24 control patients.Relative risk of PCR+ at 2 weeks with treatment, RR 0.47, p=0.1825(OH)D levels at day 14 were 52 ng/ml vs. 15 ng/ml in the intervention and control group. 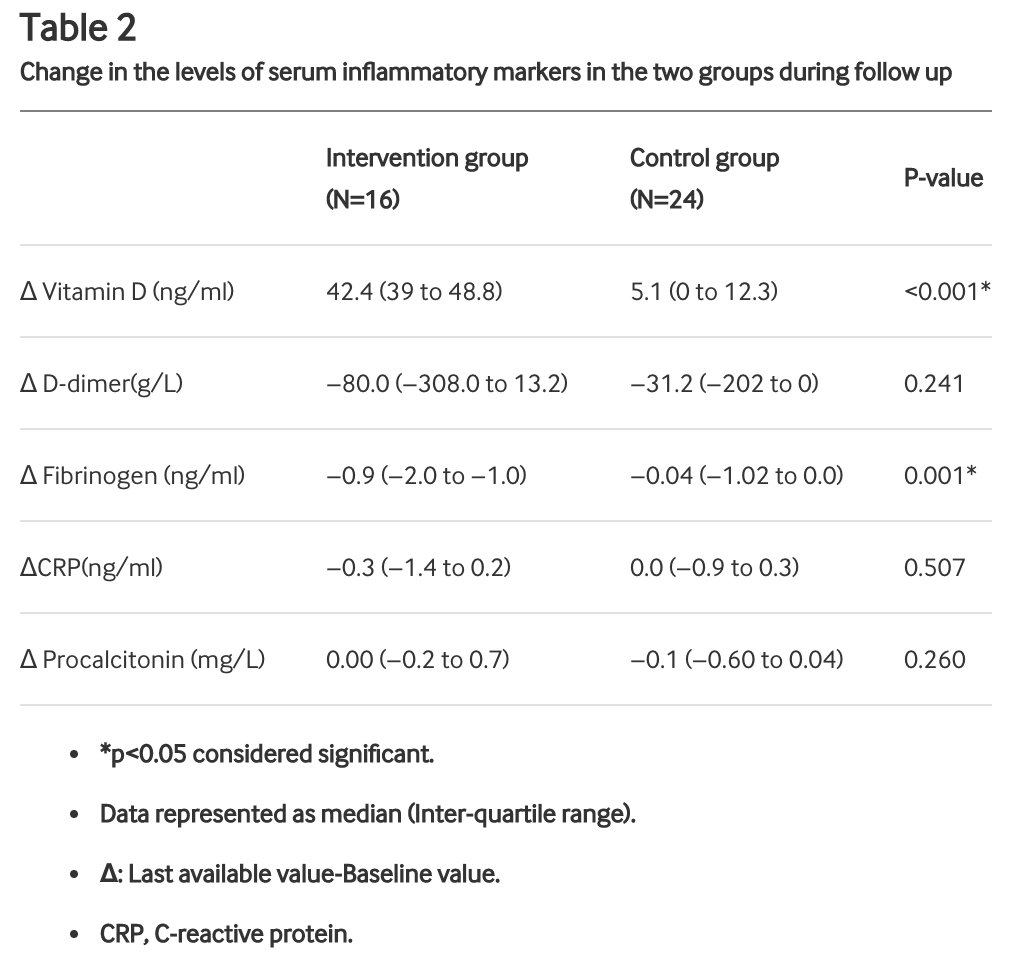 risk of no virological cure, 52.6% lower, RR 0.47, p = 0.02, treatment 6 of 16 (37.5%), control 19 of 24 (79.2%). Rastogi et al., 11/12/2020, Randomized Controlled Trial, India, South Asia, peer-reviewed, 8 authors, dosage 60,000IU days 1-7. |
| Submit Corrections or Comments |
| PrEPPEP | Cereda et al., Nutrition, doi:10.1016/j.nut.2020.111055 (Peer Reviewed) | death, ↑73.0%, p=0.14 | Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy |
| Details Retrospective 105 Parkinson's disease patients, 92 caregivers, and 127 hospital inpatients, showing higher, but not statistically significant mortality and hospitalization with treatment. Supplementation was defined as >=25,000IU/month fo.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Cereda et al., Nutrition, doi:10.1016/j.nut.2020.111055 (Peer Reviewed) |
| Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy |
Retrospective 105 Parkinson's disease patients, 92 caregivers, and 127 hospital inpatients, showing higher, but not statistically significant mortality and hospitalization with treatment. Supplementation was defined as >=25,000IU/month for at least 3 months. 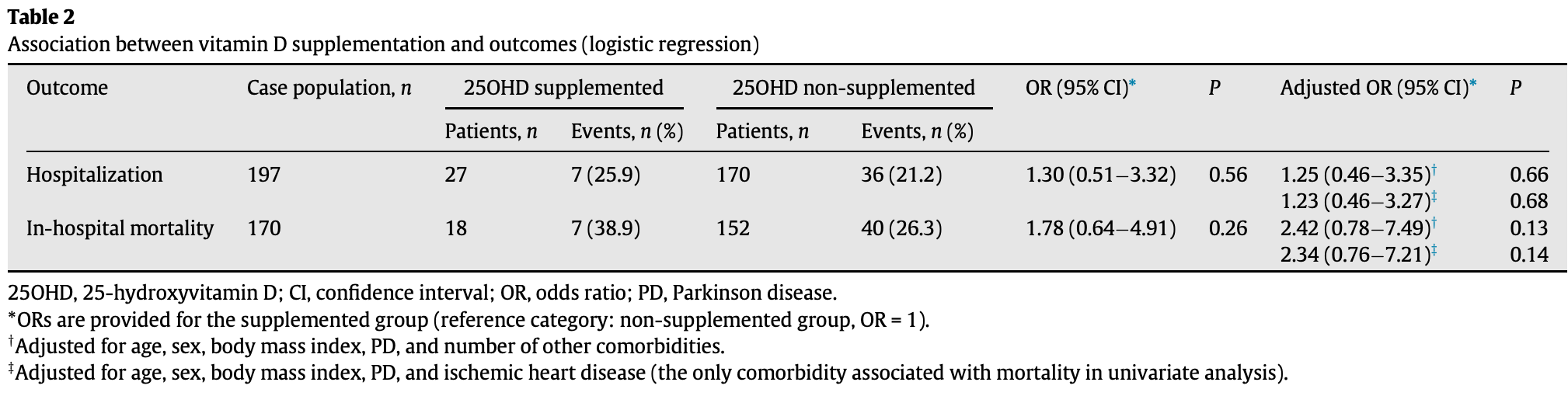 risk of death, 73.0% higher, RR 1.73, p = 0.14, treatment 7 of 18 (38.9%), control 40 of 152 (26.3%), OR converted to RR, >=25,000IU/month for at least 3 months. risk of hospitalization, 17.3% higher, RR 1.17, p = 0.68, treatment 7 of 27 (25.9%), control 36 of 170 (21.2%), OR converted to RR. Cereda et al., 11/11/2020, retrospective, Italy, Europe, peer-reviewed, 7 authors, dosage varies. |
| Submit Corrections or Comments |
| Levels | Walk et al., medRxiv, doi:10.1101/2020.11.07.20227512 (Preprint) | int./death, ↑0.4%, p=1.00 | Vitamin D - contrary to vitamin K - does not associate with clinical outcome in hospitalized COVID-19 patients |
| Details Small retrospective study of 135 patients not finding a significant difference in vitamin D status. Patients with good outcomes had a median of 45.0 nmol/L versus 37.7 nmol/L for bad outcomes, p = 0.85. Authors found that vitamin D suffi.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Walk et al., medRxiv, doi:10.1101/2020.11.07.20227512 (Preprint) |
| Vitamin D - contrary to vitamin K - does not associate with clinical outcome in hospitalized COVID-19 patients |
Small retrospective study of 135 patients not finding a significant difference in vitamin D status. Patients with good outcomes had a median of 45.0 nmol/L versus 37.7 nmol/L for bad outcomes, p = 0.85.Authors found that vitamin D sufficient persons had accelerated elastic fiber degradation, they hypothesize pro-calcification effects during COVID-19 and that vitamin K might compensate for this. 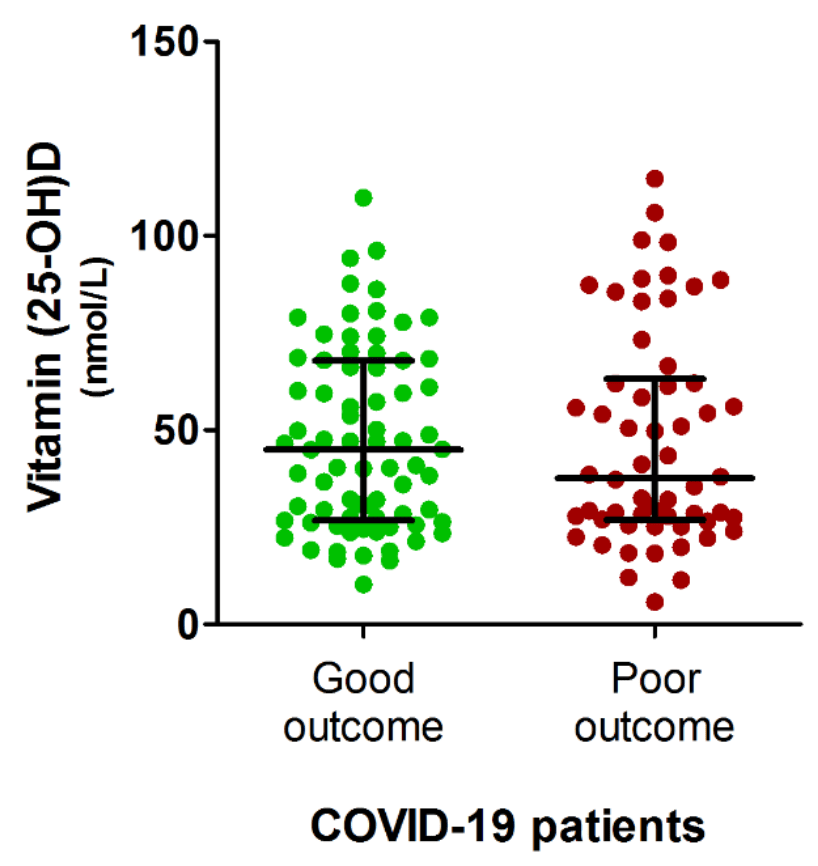 risk of intubation/death, 0.4% higher, RR 1.00, p = 1.00, high D levels 48 of 110 (43.6%), low D levels 10 of 23 (43.5%), >25nmol/L. Walk et al., 11/9/2020, retrospective, Netherlands, Europe, preprint, 5 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Annweiler et al., Nutrients, doi:10.3390/nu12113377 (Peer Reviewed) | death, ↓93.0%, p=0.02 | Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study |
| Details Retrospective study finding that regular bolus vitamin D supplementation was associated with less severe COVID-19 and better survival in frail elderly. For those receiving regular supplementation: Adjusted mortality hazard ratio with su.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Annweiler et al., Nutrients, doi:10.3390/nu12113377 (Peer Reviewed) |
| Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study |
Retrospective study finding that regular bolus vitamin D supplementation was associated with less severe COVID-19 and better survival in frail elderly.For those receiving regular supplementation:Adjusted mortality hazard ratio with supplementation HR 0.07, p = 0.017.
Risk of severe COVID-19 with supplementation OR 0.08, p = 0.033.For supplementation started after COVID-19 diagnosis:Adjusted mortality hazard ratio HR 0.37, p = 0.28.
Risk of severe COVID-19 with supplementation OR 0.46, p = 0.4. 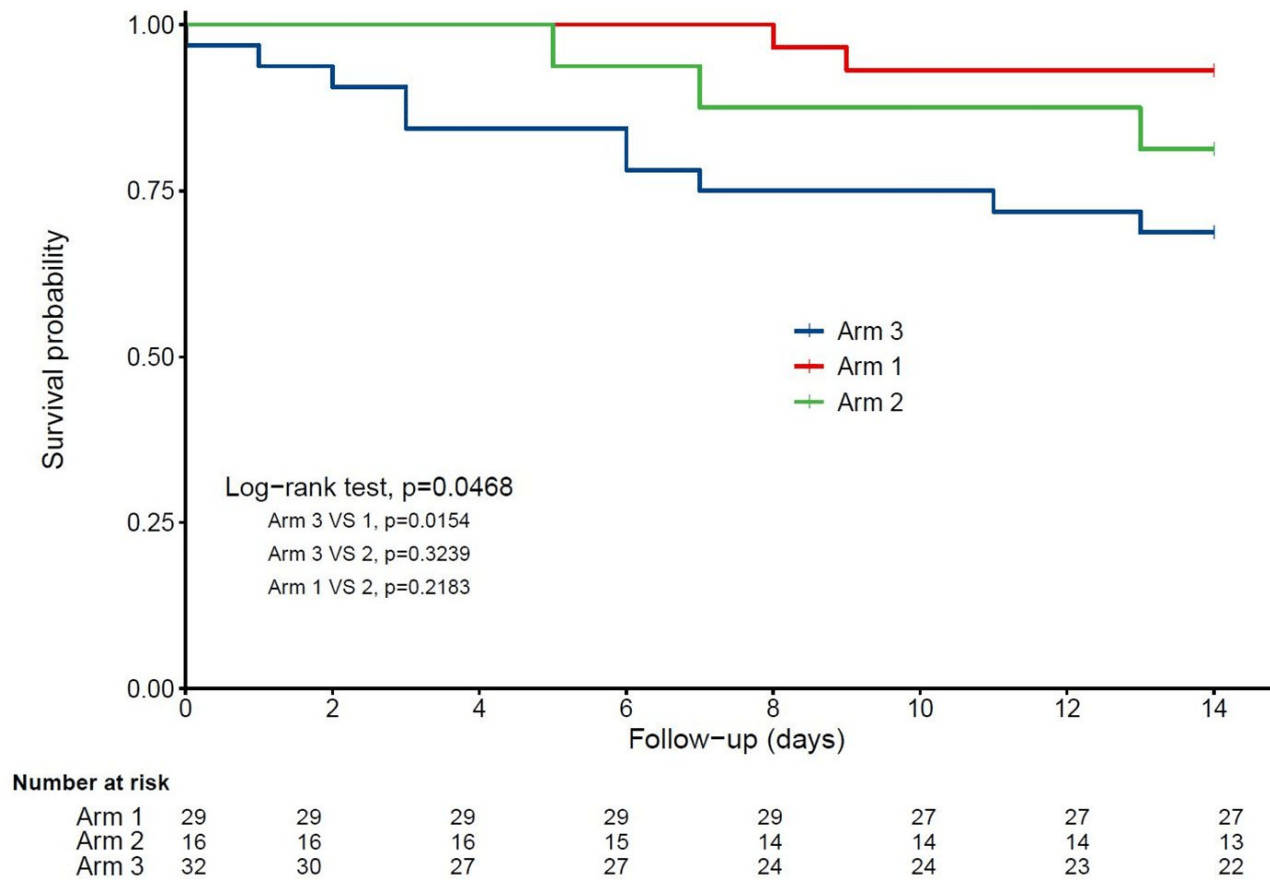 risk of death, 93.0% lower, RR 0.07, p = 0.02, treatment 2 of 29 (6.9%), control 10 of 32 (31.2%), adjusted, regular bolus supplementation. Annweiler et al., 11/2/2020, retrospective, France, Europe, peer-reviewed, 7 authors, dosage 50,000IU monthly, dose varies - 50,000 IU/month, or 80,000IU/100,000IU every 2–3 months. |
| Submit Corrections or Comments |
| Levels | Cereda et al., Clinical Nutrition (Edinburgh, Scotland), doi:10.1016/j.clnu.2020.10.055 (Peer Reviewed) | death, ↑120.0%, p=0.04 | Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital |
| Details Prospective cohort study of 129 adult hospitalized COVID-19 patients finding patients with vitamin D levels >20ng/mL had increased mortality after adjustment. This study does not account for the risk of having a serious enough case to be .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Cereda et al., Clinical Nutrition (Edinburgh, Scotland), doi:10.1016/j.clnu.2020.10.055 (Peer Reviewed) |
| Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital |
Prospective cohort study of 129 adult hospitalized COVID-19 patients finding patients with vitamin D levels >20ng/mL had increased mortality after adjustment. This study does not account for the risk of having a serious enough case to be hospitalized, and adjustments for factors correlated with vitamin D levels could obscure a potential association with vitamin D levels. 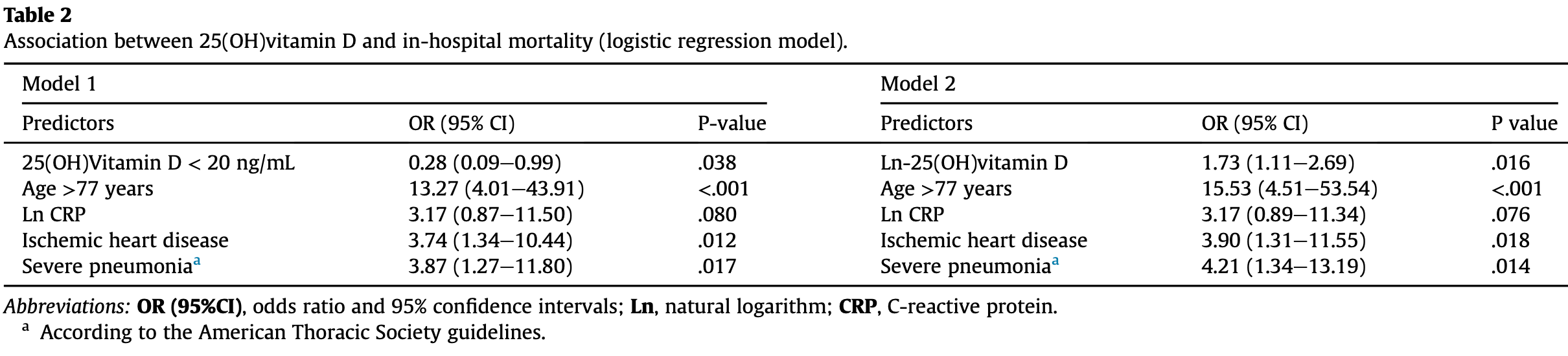 risk of death, 120.0% higher, RR 2.20, p = 0.04, high D levels 10 of 30 (33.3%), low D levels 24 of 99 (24.2%), OR converted to RR, >20ng/mL. risk of ICU admission, 86.7% lower, RR 0.13, p = 0.59, high D levels 0 of 30 (0.0%), low D levels 5 of 99 (5.1%), relative risk is not 0 because of continuity correction due to zero events. Cereda et al., 11/1/2020, prospective, Italy, Europe, peer-reviewed, 13 authors. |
| Submit Corrections or Comments |
| Late | Ohaegbulam et al., American Journal of Therapeutics, doi:10.1097/MJT.0000000000001222 (Peer Reviewed) | Vitamin D Supplementation in COVID-19 Patients: A Clinical Case Series |
| Details Small case study of 4 vitamin D deficient patients with 2 patients treated with cholecalciferol 1000 IU daily and two patients treated with ergocalciferol 50,000 IU daily for 5 days (high dose), showing that patients receiving high dose t.. |
| Details Source PDF Late treatment study Late treatment study |
| Ohaegbulam et al., American Journal of Therapeutics, doi:10.1097/MJT.0000000000001222 (Peer Reviewed) |
| Vitamin D Supplementation in COVID-19 Patients: A Clinical Case Series |
Small case study of 4 vitamin D deficient patients with 2 patients treated with cholecalciferol 1000 IU daily and two patients treated with ergocalciferol 50,000 IU daily for 5 days (high dose), showing that patients receiving high dose therapy had improved clinical recovery, with shorter lengths of stay, lower oxygen requirements, and a reduction in inflammatory marker status. 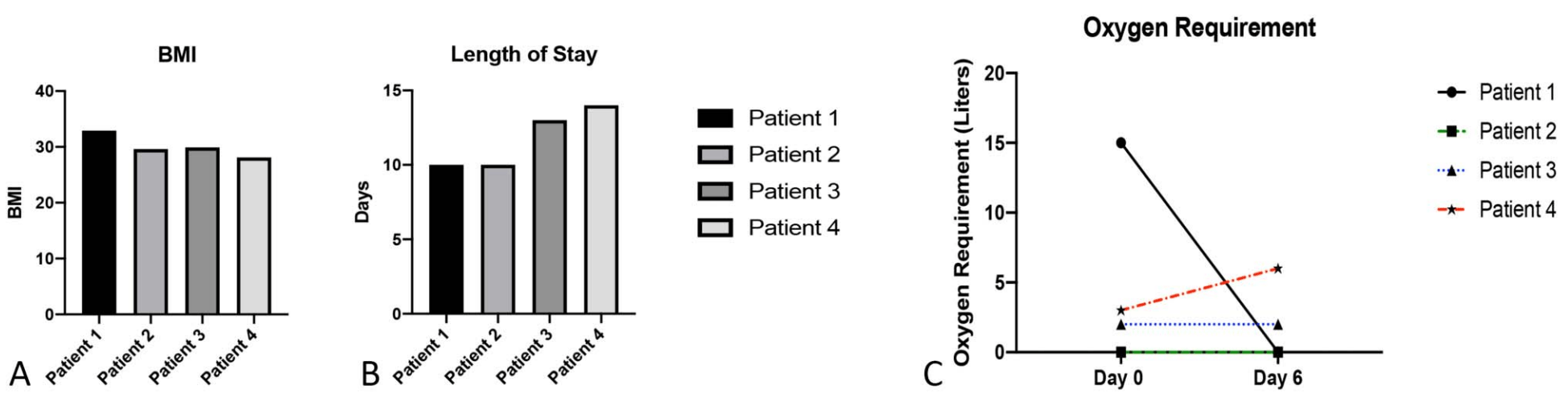 Ohaegbulam et al., 10/31/2020, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| Review | Mercola et al., Nutrients 2020, 12:11, 3361, doi:10.3390/nu12113361 (Review) (Peer Reviewed) | review | Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity |
| Details Review of vitamin D and COVID-19 concluding that the evidence seems strong enough that people and physicians can use or recommend vitamin D supplements to prevent or treat COVID-19 in light of their safety and wide therapeutic window. |
| Details Source PDF Review Review |
| Mercola et al., Nutrients 2020, 12:11, 3361, doi:10.3390/nu12113361 (Review) (Peer Reviewed) |
| Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity |
| Review of vitamin D and COVID-19 concluding that the evidence seems strong enough that people and physicians can use or recommend vitamin D supplements to prevent or treat COVID-19 in light of their safety and wide therapeutic window. Mercola et al., 10/31/2020, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Abrishami et al., European Journal of Nutrition, doi:10.1007/s00394-020-02411-0 (Peer Reviewed) | death, ↓75.9%, p=0.04 | Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study |
| Details Retrospective 73 hospitalized patients showing the probability of death in patients with vitamin D deficiency (< 25ng/mL) was 34.6% compared with 6.4% in patients with sufficient vitamin D levels. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Abrishami et al., European Journal of Nutrition, doi:10.1007/s00394-020-02411-0 (Peer Reviewed) |
| Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study |
Retrospective 73 hospitalized patients showing the probability of death in patients with vitamin D deficiency (< 25ng/mL) was 34.6% compared with 6.4% in patients with sufficient vitamin D levels. 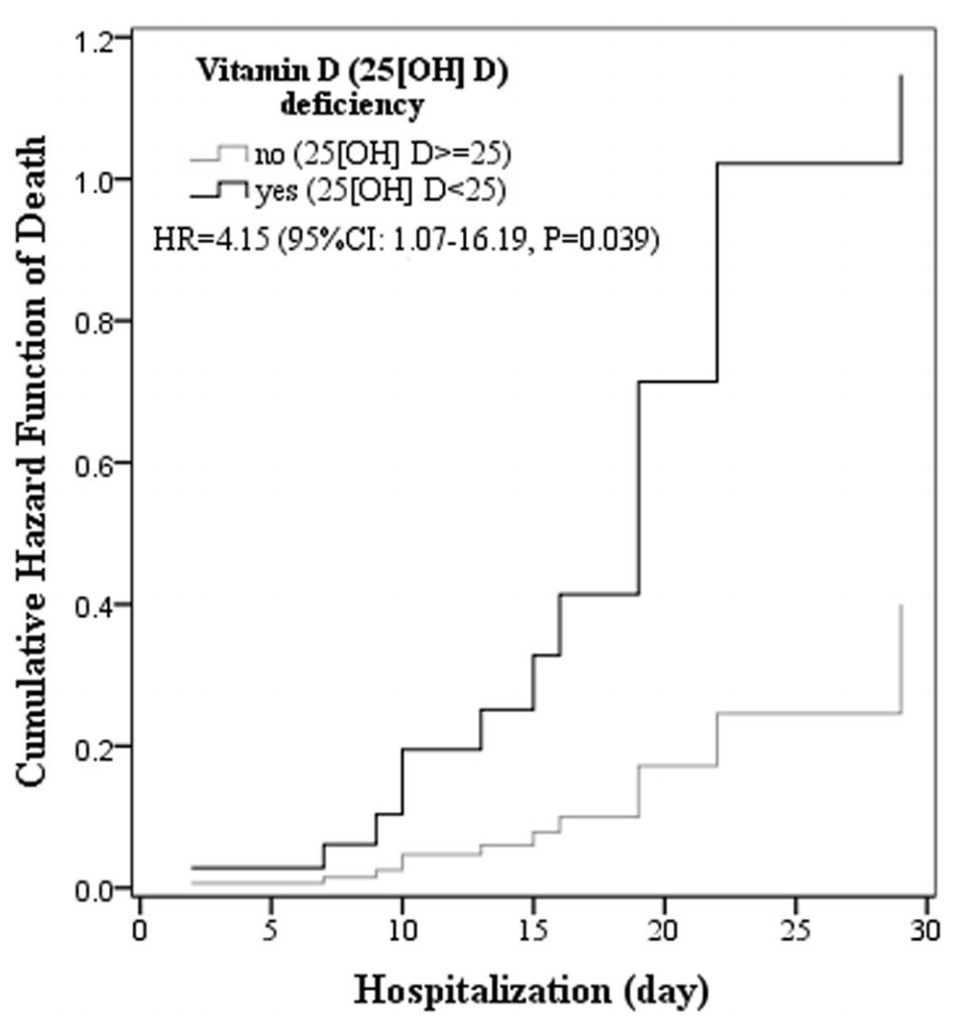 risk of death, 75.9% lower, RR 0.24, p = 0.04, high D levels (≥25ng/mL) 3 of 47 (6.4%), low D levels (<25ng/mL) 9 of 26 (34.6%), adjusted, Cox model 2. Abrishami et al., 10/30/2020, retrospective, Iran, Middle East, peer-reviewed, mean age 55.2, 7 authors. |
| Submit Corrections or Comments |
| Levels | Hernández et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgaa733 (Peer Reviewed) | death/ICU, ↓83.0%, p<0.0001 | Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection |
| Details Retrospective 216 COVID-19 patients and 197 population controls, showing vitamin D deficiency in 82.2% of COVID-19 cases and 47.2% of population-based controls (P < .0001). Authors note: "We did not find any relationship between vita.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Hernández et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgaa733 (Peer Reviewed) |
| Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection |
Retrospective 216 COVID-19 patients and 197 population controls, showing vitamin D deficiency in 82.2% of COVID-19 cases and 47.2% of population-based controls (P < .0001). Authors note: "We did not find any relationship between vitamin D concentrations or vitamin deficiency and the severity of the disease". While no association was found within hospitalized patients, there is an association with hospitalization, and hospitalization is an indication of COVID-19 severity.19 of the COVID-19 patients were taking vitamin D supplements, showing lower ventilation and ICU admission, but no significant difference in mortality. 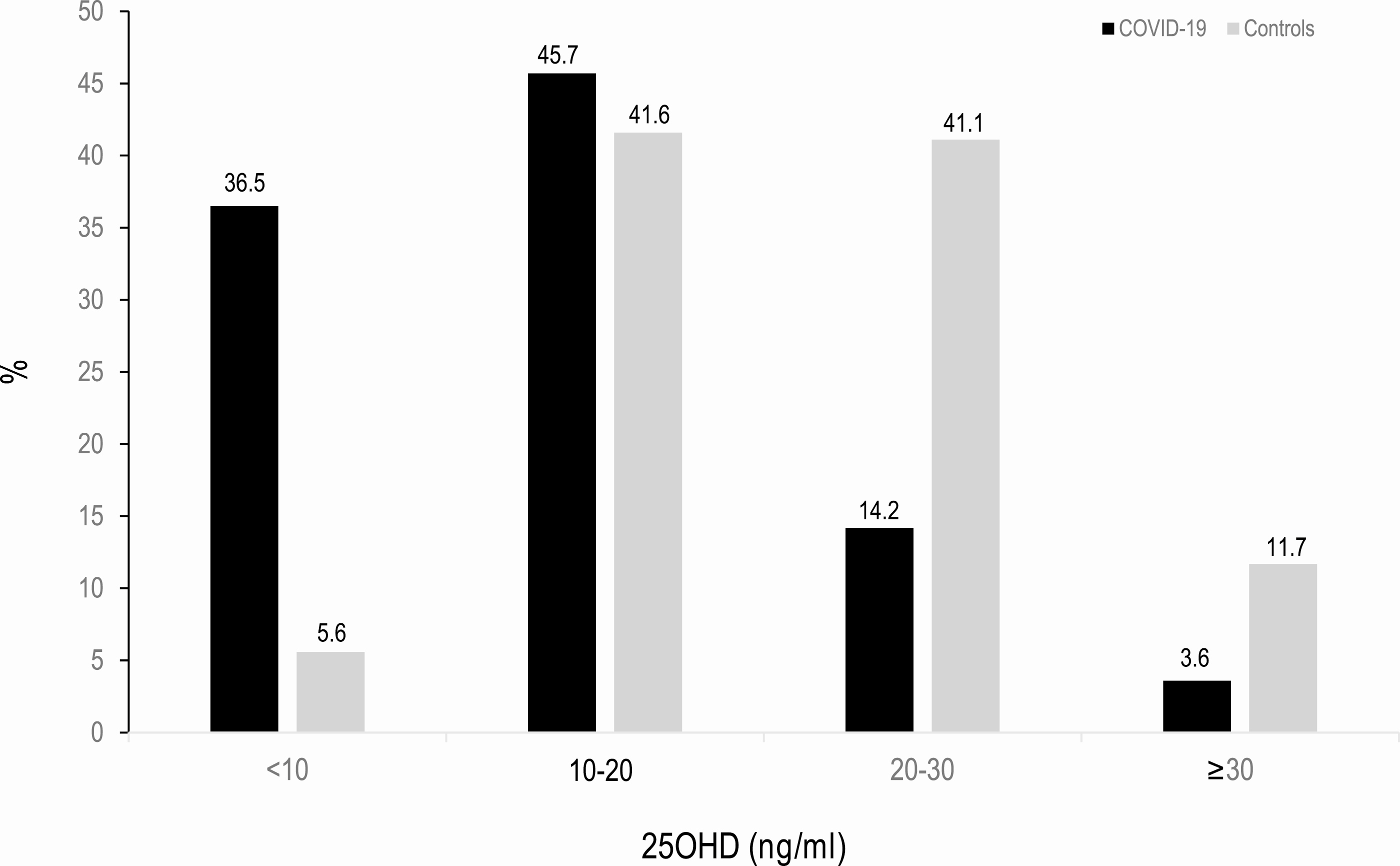 risk of combined death/ICU/ventilation, 83.0% lower, RR 0.17, p < 0.001, high D levels 35, low D levels 162, >= 20ng/mL risk of hospitalization * risk of death/ICU/ventilation | hospitalization. risk of combined death/ICU/ventilation if hospitalized, 12.0% lower, RR 0.88, p = 0.86, high D levels 35, low D levels 162, >= 20ng/mL risk of death/ICU/ventilation | hospitalization. risk of hospitalization, 80.6% lower, RR 0.19, p < 0.001, >= 20ng/mL. risk of death, 3.7% higher, RR 1.04, p = 1.00, high D levels 2 of 19 (10.5%), low D levels 20 of 197 (10.2%), supplementation. risk of mechanical ventilation, 75.9% lower, RR 0.24, p = 0.13, high D levels 1 of 19 (5.3%), low D levels 43 of 197 (21.8%), supplementation. risk of ICU admission, 79.3% lower, RR 0.21, p = 0.05, high D levels 1 of 19 (5.3%), low D levels 50 of 197 (25.4%), supplementation. hospitalization time, 33.3% lower, relative time 0.67, p = 0.11, high D levels 19, low D levels 197, supplementation. Hernández et al., 10/27/2020, retrospective, Spain, Europe, peer-reviewed, 12 authors. |
| Submit Corrections or Comments |
| Levels | Tomasa-Irriguible et al., Metabolites, doi:10.3390/metabo11090565 (preprint 10/26/2020) (Peer Reviewed) | ventilation, ↓35.0%, p=0.21 | Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave |
| Details Retrospective 120 hospitalized patients in Spain showing no significant differences for vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Tomasa-Irriguible et al., Metabolites, doi:10.3390/metabo11090565 (preprint 10/26/2020) (Peer Reviewed) |
| Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave |
Retrospective 120 hospitalized patients in Spain showing no significant differences for vitamin D deficiency. 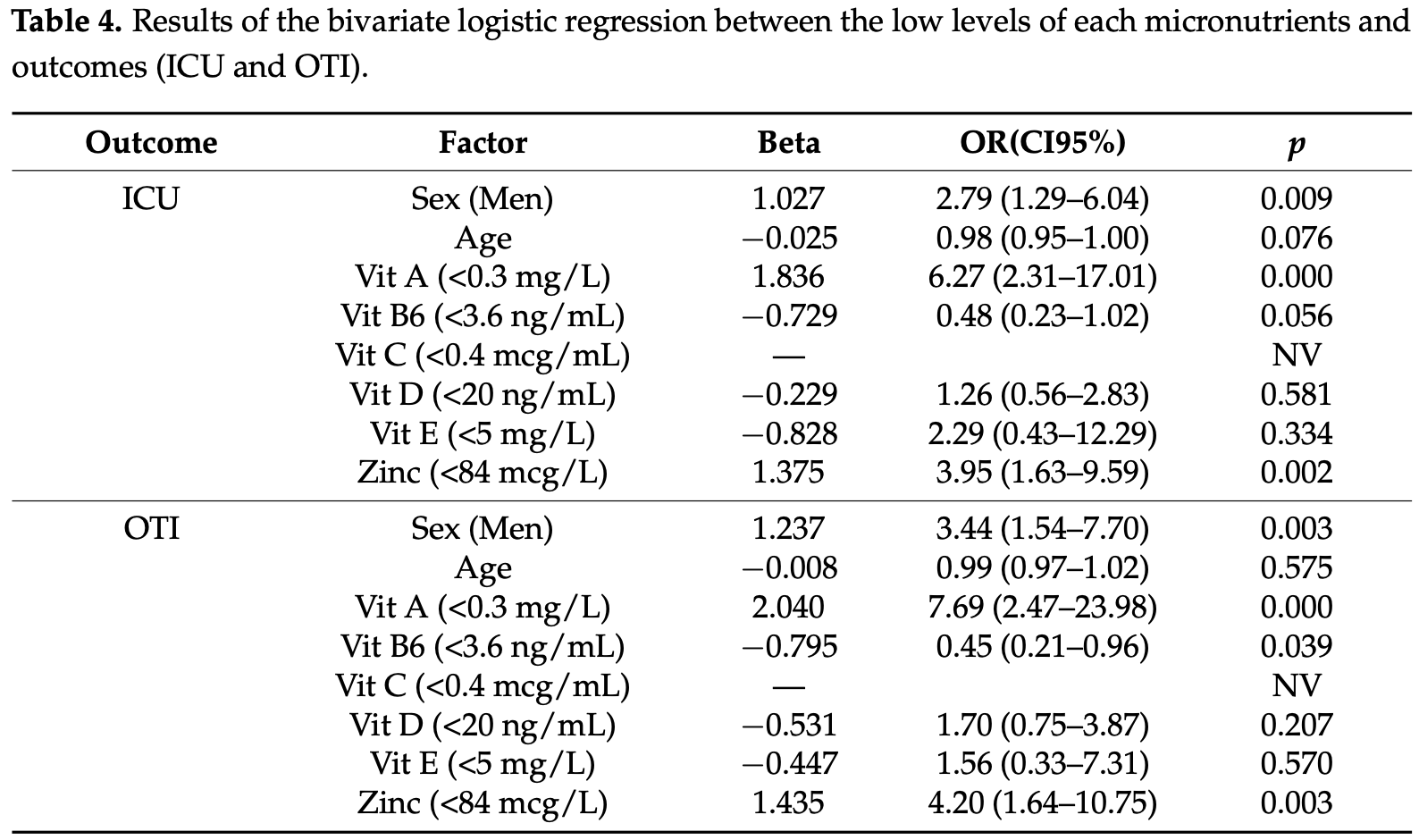 risk of mechanical ventilation, 35.0% lower, RR 0.65, p = 0.21, high D levels 15 of 27 (55.6%), low D levels 18 of 78 (23.1%), adjusted, OR converted to RR, ≥20 ng/mL, bivariate logistic regression. risk of ICU admission, 16.9% lower, RR 0.83, p = 0.58, high D levels 0 of 27 (0.0%), low D levels 17 of 78 (21.8%), adjusted, OR converted to RR, ≥20 ng/mL, bivariate logistic regression. Tomasa-Irriguible et al., 10/26/2020, retrospective, Spain, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Review | Basha et al., Clinical Epidemiology and Global Health, doi:10.1016/j.cegh.2020.10.005 (Review) (Peer Reviewed) | review | Is the shielding effect of cholecalciferol in SARS CoV-2 infection dependable? An evidence based unraveling |
| Details Review of vitamin D for COVID-19, concluding that the available evidence is very suggestive of protective and preventive effect of vitamin D. Authors note that strict lockdown (longer time indoors and home quarantine) may increase the r.. |
| Details Source PDF Review Review |
| Basha et al., Clinical Epidemiology and Global Health, doi:10.1016/j.cegh.2020.10.005 (Review) (Peer Reviewed) |
| Is the shielding effect of cholecalciferol in SARS CoV-2 infection dependable? An evidence based unraveling |
| Review of vitamin D for COVID-19, concluding that the available evidence is very suggestive of protective and preventive effect of vitamin D. Authors note that strict lockdown (longer time indoors and home quarantine) may increase the risk of developing vitamin D deficiency. They suggest it is the duty of governments to strengthen recommendations regarding nutritional supplementation (especially vitamin D and C), particularly under quarantine and lockdown times. Basha et al., 10/21/2020, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Macaya et al., Nutr. Hosp., doi:10.20960/nh.03193 (Peer Reviewed) | severe case, ↓55.0%, p=0.07 | Interaction between age and vitamin D deficiency in severe COVID-19 infection |
| Details Retrospective 80 hospitalized patients in Spain showing higher risk of severe COVID-19 with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Macaya et al., Nutr. Hosp., doi:10.20960/nh.03193 (Peer Reviewed) |
| Interaction between age and vitamin D deficiency in severe COVID-19 infection |
Retrospective 80 hospitalized patients in Spain showing higher risk of severe COVID-19 with vitamin D deficiency. 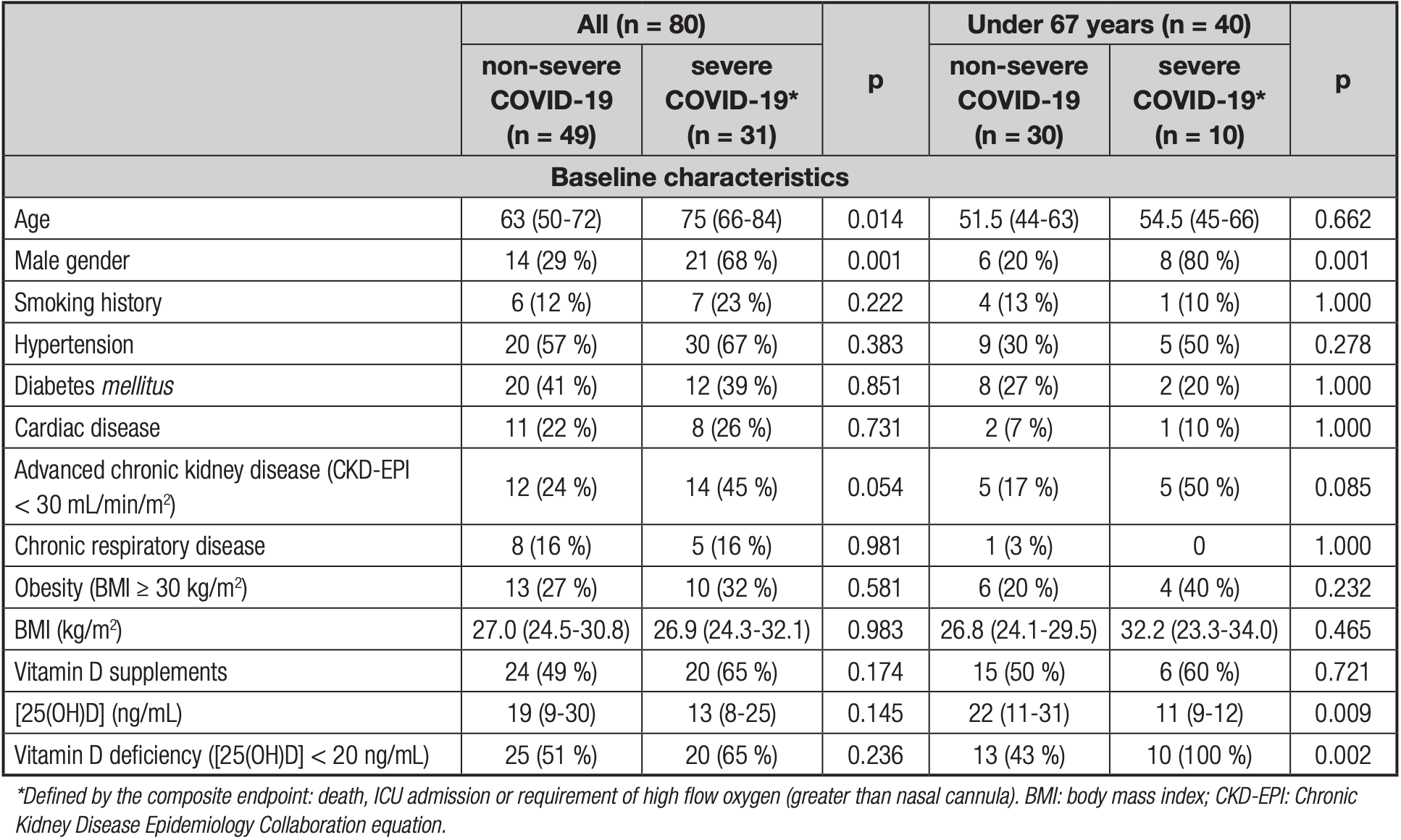 risk of severe case, 55.0% lower, RR 0.45, p = 0.07, high D levels 11 of 35 (31.4%), low D levels 20 of 45 (44.4%), OR converted to RR, >20ng/mL. Macaya et al., 10/21/2020, retrospective, Spain, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Blanch-Rubió et al., Aging, doi:10.18632/aging.104117 (Peer Reviewed) | cases, ↓8.0%, p=0.68 | Influence of anti-osteoporosis treatments on the incidence of COVID-19 in patients with non-inflammatory rheumatic conditions |
| Details Retrospective 2,102 rheumatology patients in Spain showing lower, but not statistically significant, cases with vitamin D supplementation. Details of vitamin D supplementation are not providied - other patients may have also independently.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Blanch-Rubió et al., Aging, doi:10.18632/aging.104117 (Peer Reviewed) |
| Influence of anti-osteoporosis treatments on the incidence of COVID-19 in patients with non-inflammatory rheumatic conditions |
Retrospective 2,102 rheumatology patients in Spain showing lower, but not statistically significant, cases with vitamin D supplementation. Details of vitamin D supplementation are not providied - other patients may have also independently taken vitamin D. 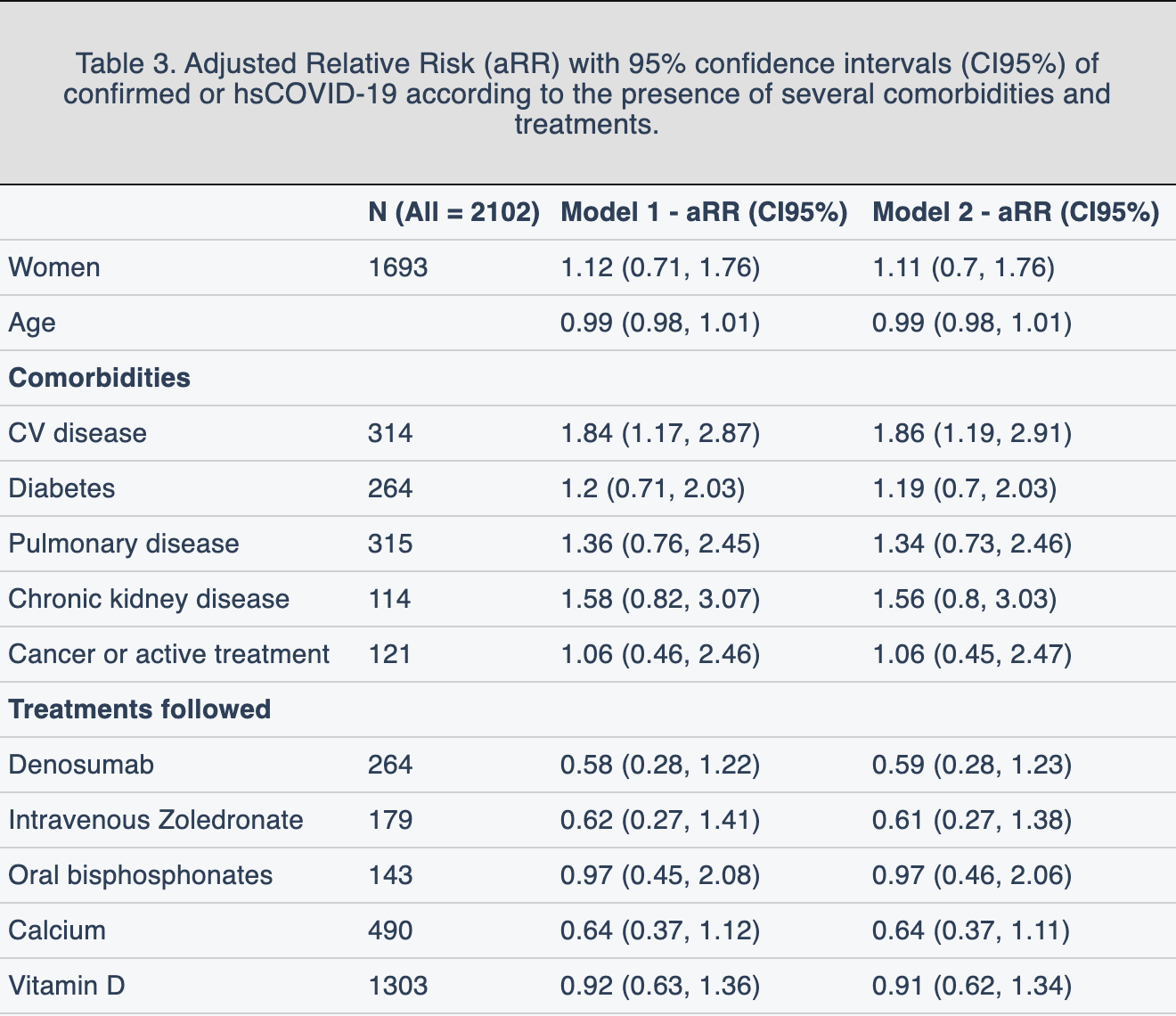 risk of case, 8.0% lower, RR 0.92, p = 0.68, treatment 62 of 1,303 (4.8%), control 47 of 799 (5.9%), adjusted. Blanch-Rubió et al., 10/20/2020, retrospective, Spain, Europe, peer-reviewed, 10 authors, dosage not specified. |
| Submit Corrections or Comments |
| Early, PrEP | Annweiler et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2020.105771 (Peer Reviewed) | death, ↓89.0%, p=0.002 | Vitamin D and survival in COVID-19 patients: A quasi-experimental study |
| Details Vitamin D3 supplementation during or just before COVID-19 was associated with 68% lower mortality and less severe COVID-19 in frail elderly. Retrospective 66 French nursing home residents, mean age 87.7, 9 control patients, and 57 that r.. |
| Details Source PDF Early, PrEP Early, PrEP |
| Annweiler et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2020.105771 (Peer Reviewed) |
| Vitamin D and survival in COVID-19 patients: A quasi-experimental study |
Vitamin D3 supplementation during or just before COVID-19 was associated with 68% lower mortality and less severe COVID-19 in frail elderly.Retrospective 66 French nursing home residents, mean age 87.7, 9 control patients, and 57 that received an oral bolus of 80,000 IU vitamin D3 either in the week following the suspicion or diagnosis of COVID-19, or during the previous month. 17.5% mortality in the treatment group and 55.6% in the control group. 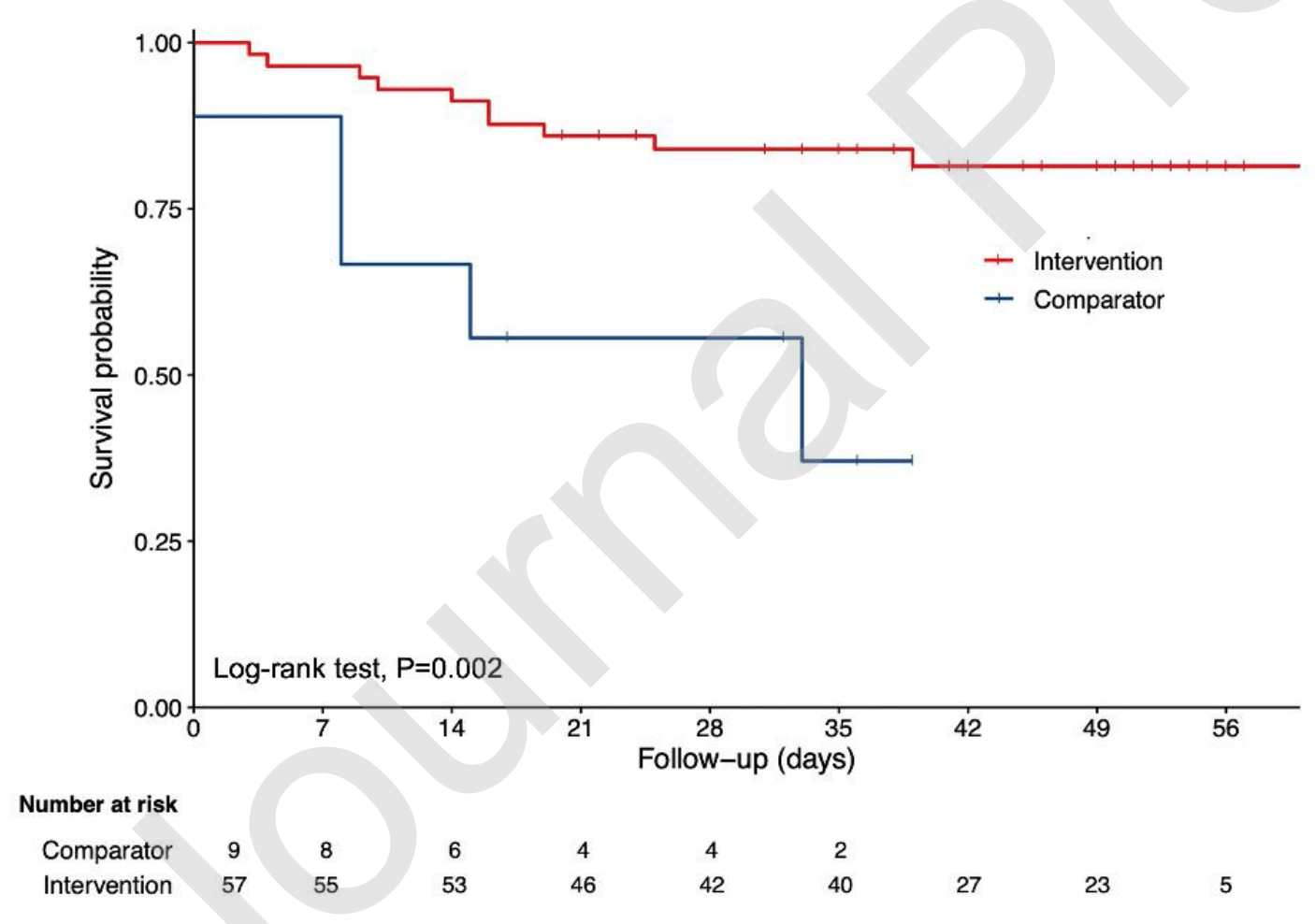 risk of death, 89.0% lower, RR 0.11, p = 0.002, treatment 10 of 57 (17.5%), control 5 of 9 (55.6%), adjusted. Annweiler et al., 10/13/2020, retrospective, France, Europe, peer-reviewed, mean age 87.7, 6 authors, dosage 80,000IU single dose, 80,000IU either in the week following the suspicion or diagnosis of COVID-19, or during the previous month. |
| Submit Corrections or Comments |
| Levels | Ye et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.182600 (Peer Reviewed) | hosp., ↓93.4%, p=0.03 | Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity? A Case-Control Study |
| Details Case control study in China comparing 62 patients with 80 healthy controls showing vitamin D deficiency is a risk factor for COVID-19, especially for severe/critical cases. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Ye et al., Journal of the American College of Nutrition, doi:10.1080/07315724.2020.182600 (Peer Reviewed) |
| Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity? A Case-Control Study |
Case control study in China comparing 62 patients with 80 healthy controls showing vitamin D deficiency is a risk factor for COVID-19, especially for severe/critical cases. 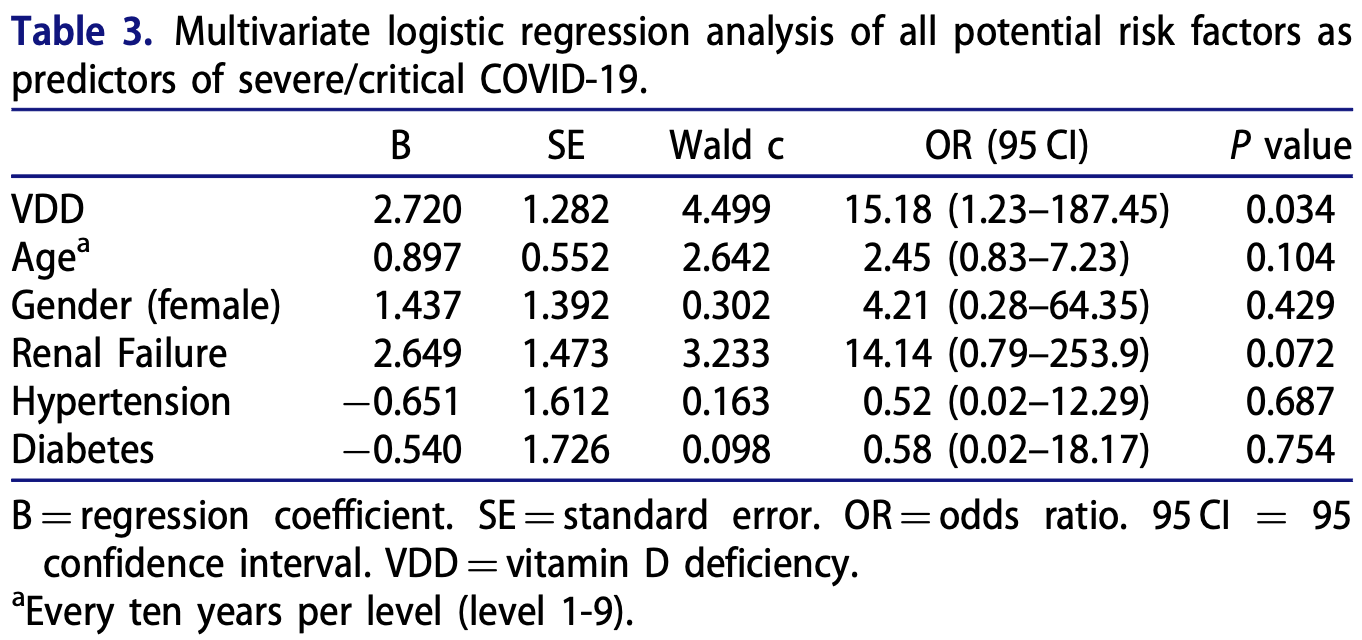 risk of severe/critical COVID-19, 93.4% lower, RR 0.07, p = 0.03, high D levels 2 of 36 (5.6%), low D levels 8 of 26 (30.8%), adjusted, >50nmol/L. Ye et al., 10/13/2020, retrospective, China, Asia, peer-reviewed, 18 authors. |
| Submit Corrections or Comments |
| Levels | Faniyi et al., medRxiv, doi:10.1101/2020.10.05.20206706 (Preprint) | seropositive, ↓28.8%, p=0.003 | Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic |
| Details Analysis of vitamin D status and anti-SARS-Cov-2 antibodies in UK healthcare workers finding that Vitamin D deficiency is a risk factor for COVID-19 seroconversion. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Faniyi et al., medRxiv, doi:10.1101/2020.10.05.20206706 (Preprint) |
| Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic |
Analysis of vitamin D status and anti-SARS-Cov-2 antibodies in UK healthcare workers finding that Vitamin D deficiency is a risk factor
for COVID-19 seroconversion. risk of seropositive, 28.8% lower, RR 0.71, p = 0.003, high D levels 170 of 331 (51.4%), low D levels 44 of 61 (72.1%), >30nmol/L. Faniyi et al., 10/6/2020, prospective, United Kingdom, Europe, preprint, 10 authors. |
| Submit Corrections or Comments |
| Levels | Yılmaz et al., Pediatric Pulmonology, doi:10.1002/ppul.25106 (Peer Reviewed) | severe case, ↓73.4%, p=1.00 | Is vitamin D deficiency a risk factor for COVID‐19 in children? |
| Details Retrospective 40 hospitalized pediatric COVID-19 patients and 45 healthy controls showing significantly lower vitamin D levels for COVID-19 patients (13.1 vs. 34.8µg/L), and that, within the hospitalized patients, there was more moderate .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Yılmaz et al., Pediatric Pulmonology, doi:10.1002/ppul.25106 (Peer Reviewed) |
| Is vitamin D deficiency a risk factor for COVID‐19 in children? |
Retrospective 40 hospitalized pediatric COVID-19 patients and 45 healthy controls showing significantly lower vitamin D levels for COVID-19 patients (13.1 vs. 34.8µg/L), and that, within the hospitalized patients, there was more moderate and severe cases for patients with low vitamin D levels (non-statistically significant due to the small numbers). 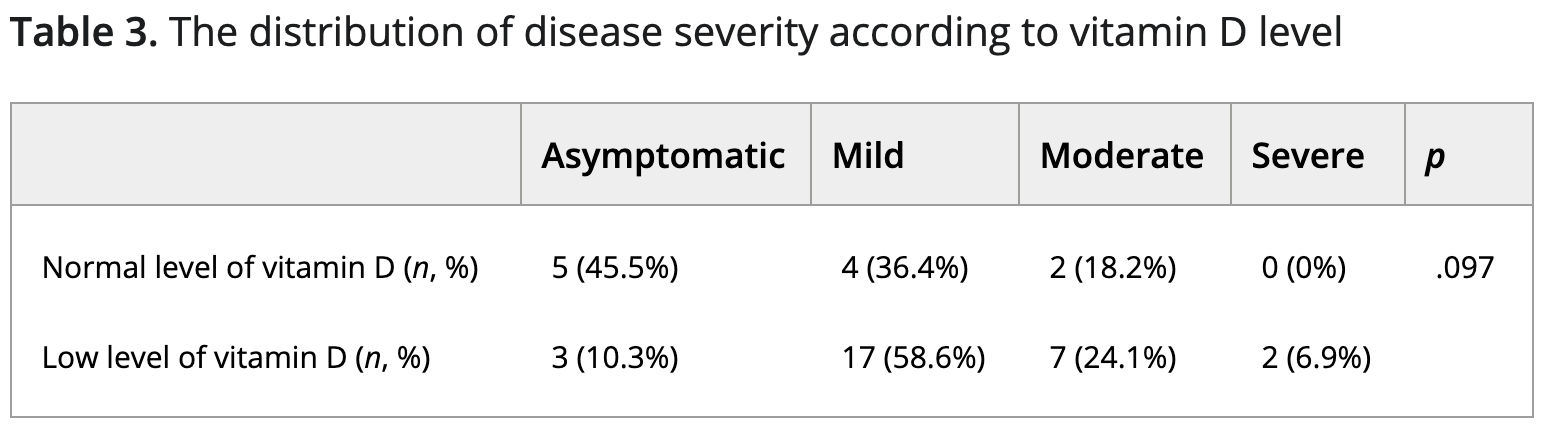 risk of severe case, 73.4% lower, RR 0.27, p = 1.00, high D levels 0 of 11 (0.0%), low D levels 2 of 29 (6.9%), relative risk is not 0 because of continuity correction due to zero events, >20ng/ml. risk of moderate or severe case, 41.4% lower, RR 0.59, p = 0.69, high D levels 2 of 11 (18.2%), low D levels 9 of 29 (31.0%), >20ng/ml. Yılmaz et al., 10/5/2020, retrospective, Turkey, Europe, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| Levels | Karahan et al., J. Nutr. Health Aging, doi:10.1007/s12603-020-1479-0 (Peer Reviewed) | death, ↓82.5%, p<0.0001 | Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey |
| Details Retrospective 149 COVID-19 patients, 69.1% with vitamin D deficiency, showing lower vitamin D levels associated with higher mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Karahan et al., J. Nutr. Health Aging, doi:10.1007/s12603-020-1479-0 (Peer Reviewed) |
| Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey |
Retrospective 149 COVID-19 patients, 69.1% with vitamin D deficiency, showing lower vitamin D levels associated with higher mortality. 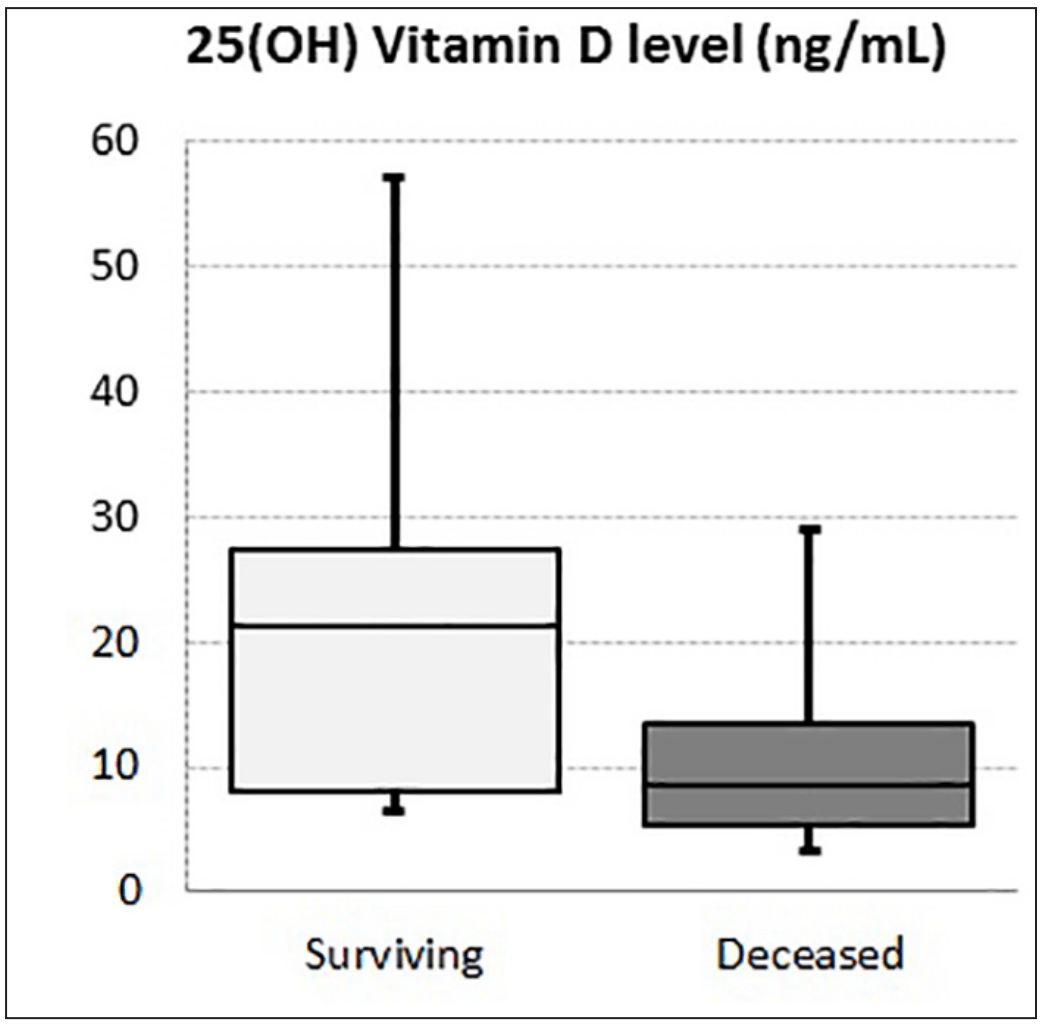 risk of death, 82.5% lower, RR 0.17, p < 0.001, high D levels 5 of 46 (10.9%), low D levels 64 of 103 (62.1%), >20nmol/L. Karahan et al., 10/5/2020, retrospective, Turkey, Europe, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| Levels | Kerget el al., Tuberk Toraks, doi:10.5578/tt.70027 (Peer Reviewed) | Evaluation of the relationship of serum vitamin D levels in COVID-19 patients with clinical course and prognosis |
| Details Prospective study of 88 hospitalized PCR+ COVID-19 patients and 20 asymptomatic PCR- medical personnel, showing lower vitamin D levels correlated with COVID-19 and with the development of ARDS and MAS. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Kerget el al., Tuberk Toraks, doi:10.5578/tt.70027 (Peer Reviewed) |
| Evaluation of the relationship of serum vitamin D levels in COVID-19 patients with clinical course and prognosis |
Prospective study of 88 hospitalized PCR+ COVID-19 patients and 20 asymptomatic PCR- medical personnel, showing lower vitamin D levels correlated with COVID-19 and with the development of ARDS and MAS. 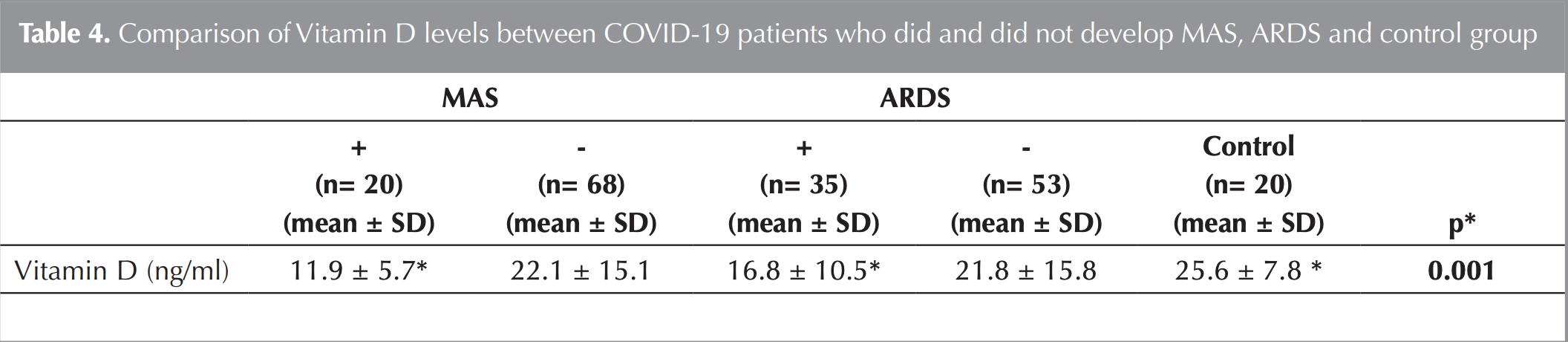 Kerget et al., 9/30/2020, prospective, Turkey, Europe, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Levels | Maghbooli et al., PLOS One, doi:10.1371/journal.pone.0239799 (Peer Reviewed) | death, ↓51.7%, p=0.08 | Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection |
| Details Retrospective 235 hospitalized patients showing a significant association between vitamin D sufficiency and reduction in clinical severity. For patients over 40, mortality was 9.7% with 25(OH)D levels >30ng/mL, versus 20% for <30ng/mL. .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Maghbooli et al., PLOS One, doi:10.1371/journal.pone.0239799 (Peer Reviewed) |
| Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection |
Retrospective 235 hospitalized patients showing a significant association between vitamin D sufficiency and reduction in clinical severity.For patients over 40, mortality was 9.7% with 25(OH)D levels >30ng/mL, versus 20% for <30ng/mL.A significant reduction in serum CRP, an inflammatory marker, along with increased lymphocytes percentage suggest that vitamin D sufficiency may help modulate the immune response possibly by reducing the risk for cytokine storm in response to this viral infection. 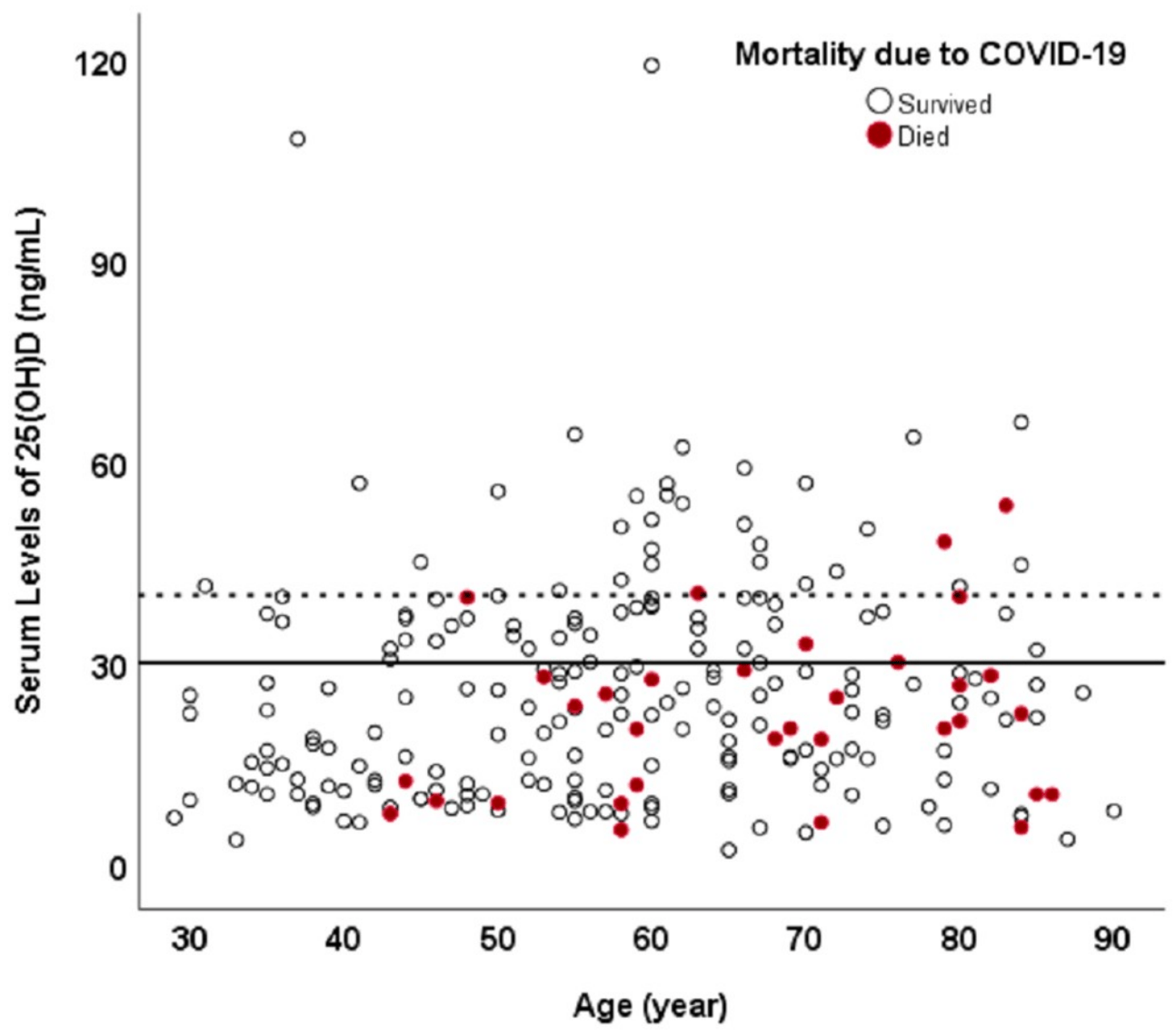 risk of death, 51.7% lower, RR 0.48, p = 0.08, high D levels 7 of 72 (9.7%), low D levels 27 of 134 (20.1%), age >40. risk of mechanical ventilation, 31.6% lower, RR 0.68, p = 0.49, high D levels 6 of 77 (7.8%), low D levels 18 of 158 (11.4%). risk of ICU admission, 32.0% lower, RR 0.68, p = 0.33, high D levels 11 of 77 (14.3%), low D levels 33 of 158 (20.9%), >30nmol/L. Maghbooli et al., 9/25/2020, retrospective, Iran, Middle East, peer-reviewed, 11 authors. |
| Submit Corrections or Comments |
| Levels | Kaufman et al., PLOS One, doi:10.1371/journal.pone.0239252 (Peer Reviewed) | cases, ↓53.0%, p<0.001 | SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels |
| Details Analysis of 191,779 patients in the US finding COVID-19 positivity strongly and inversely associated with circulating 25(OH)D levels. The relationship persists across latitudes, races/ethnicities, gender, and age ranges. COVID-19 adjuste.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Kaufman et al., PLOS One, doi:10.1371/journal.pone.0239252 (Peer Reviewed) |
| SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels |
Analysis of 191,779 patients in the US finding COVID-19 positivity strongly and inversely associated with circulating 25(OH)D levels. The relationship persists across latitudes, races/ethnicities, gender, and age ranges.COVID-19 adjusted odds ratio OR 0.984 per ng/mL increment, p<0.001). The decrease in positivity rate appeared to plateau as values approached 55 ng/mL.Patients with high D levels (>55 ng/mL) compared to patients with very low D levels (<20 ng/mL) have a much lower risk of COVID-19 cases, with unadjusted RR 0.47, p<0.001. 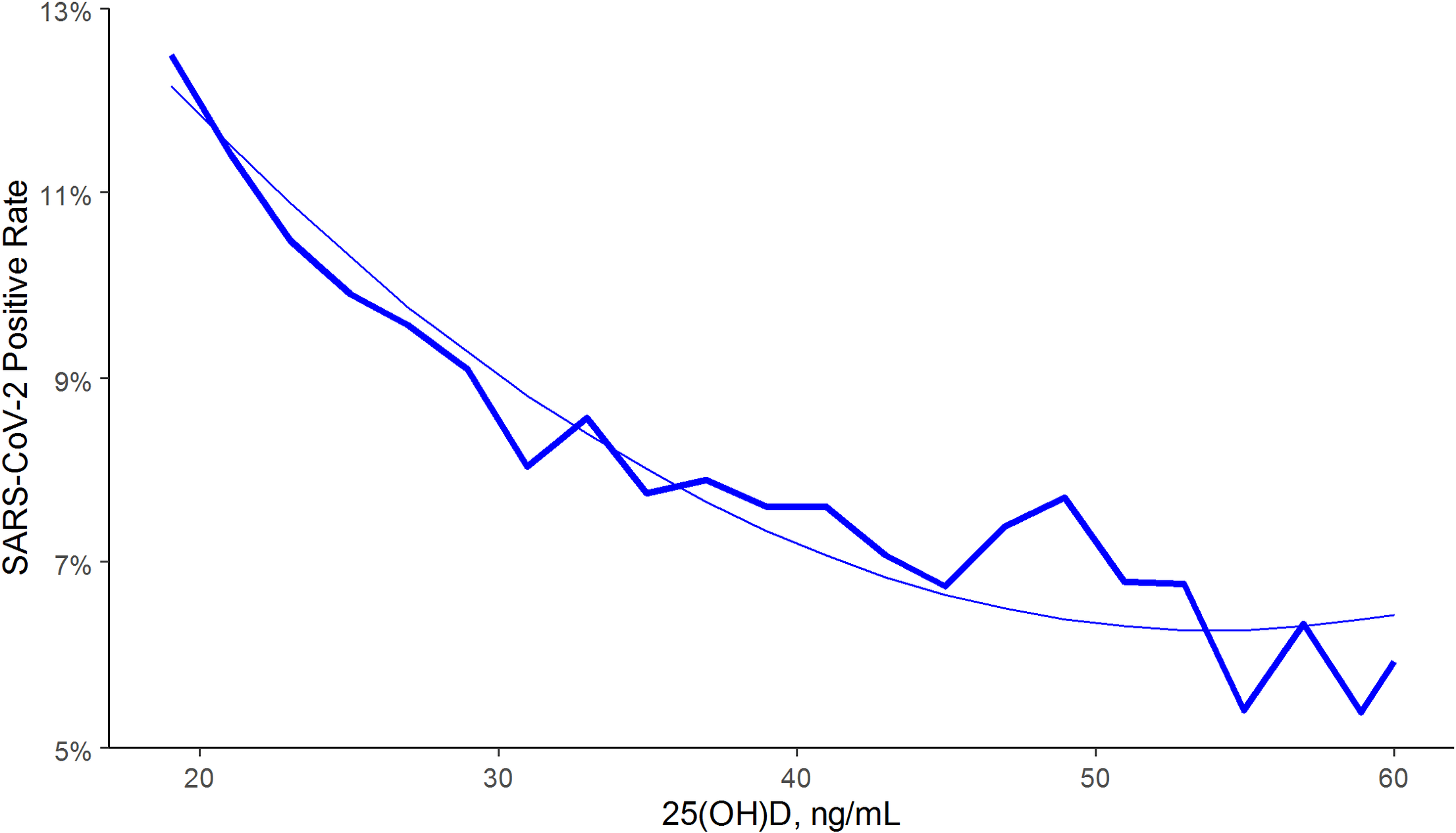 risk of case, 53.0% lower, RR 0.47, p < 0.001, high D levels 12,321, low D levels 39,190, >55 ng/mL vs. <20 ng/mL. Kaufman et al., 9/17/2020, retrospective, population-based cohort, USA, North America, peer-reviewed, median age 54.0, 5 authors. |
| Submit Corrections or Comments |
| Levels | Radujkovic et al., Nutrients 2020, 12:9, 2757, doi:10.3390/nu12092757 (Peer Reviewed) | death, ↓93.2%, p=0.001 | Vitamin D Deficiency and Outcome of COVID-19 Patients |
| Details Observational study 185 patients in Germany shows an association between vitamin D status and severity and mortality. Adjusted hazard ratio of vitamin D sufficiency for combined mechanical ventilation and death was HR 0.16, p < 0.001, and.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Radujkovic et al., Nutrients 2020, 12:9, 2757, doi:10.3390/nu12092757 (Peer Reviewed) |
| Vitamin D Deficiency and Outcome of COVID-19 Patients |
Observational study 185 patients in Germany shows an association between vitamin D status and severity and mortality. Adjusted hazard ratio of vitamin D sufficiency for combined mechanical ventilation and death was HR 0.16, p < 0.001, and for death HR 0.068, p < 0.001. 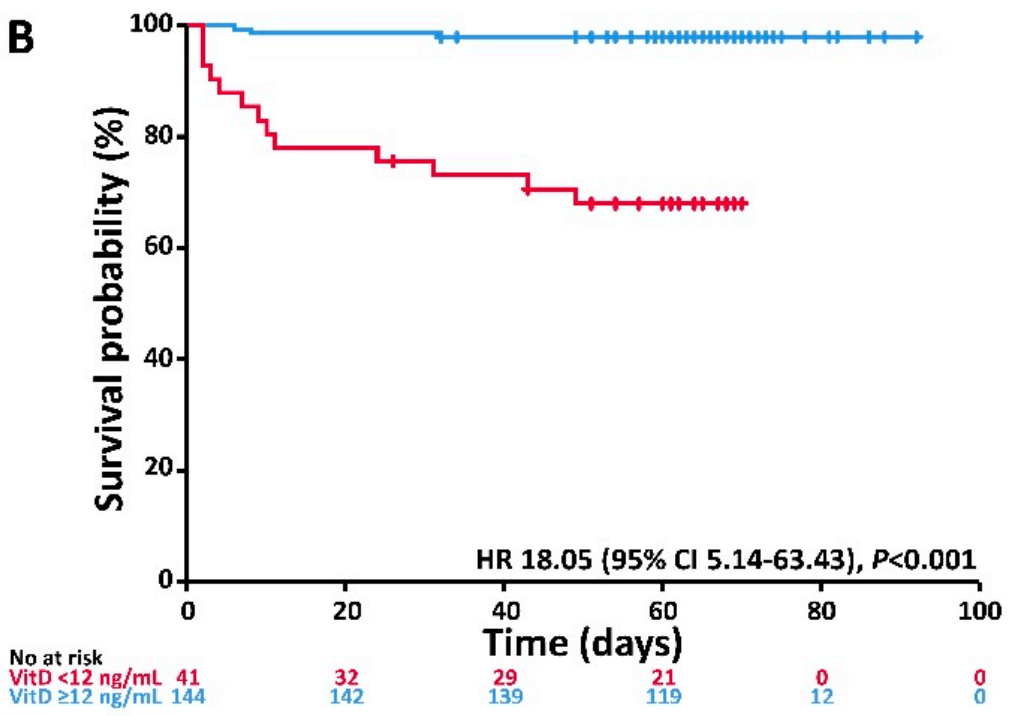 risk of death, 93.2% lower, RR 0.07, p = 0.001, high D levels 144, low D levels 12, >30nmol/L. risk of intubation/death, 84.0% lower, RR 0.16, p < 0.001, high D levels 144, low D levels 12, >30nmol/L. Radujkovic et al., 9/10/2020, prospective, Germany, Europe, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Israel et al., medRxiv, doi:https://www.medrxiv.org/content/10.1101/2020.09.04.20188268v1 (Preprint) | cases, ↓21.3%, p<0.001 | The link between vitamin D deficiency and Covid-19 in a large population |
| Details Large observational population study showing a strong association between vitamin D deficiency and COVID-19. Liquid vitamin D (more commonly used in this study) was associated with lower risk of cases, however tablets were associated wit.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Israel et al., medRxiv, doi:https://www.medrxiv.org/content/10.1101/2020.09.04.20188268v1 (Preprint) |
| The link between vitamin D deficiency and Covid-19 in a large population |
Large observational population study showing a strong association between vitamin D deficiency and COVID-19.Liquid vitamin D (more commonly used in this study) was associated with lower risk of cases, however tablets were associated with a higher risk. Authors propose the following explanation: "the virus port of entry is the oropharynx, it is where it first reaches mucosal membranes, initially replicates and causes its first detectable effects (anosmia, agusia, sore throat). High vitamin D concentration in the oropharynx might be the most important factor that prevents this initial infection and replication. Vitamin D in drop form is likely mostly absorbed by the mucous membranes of the oropharynx, and the vitamin D concentration there is likely to be elevated following drops intake." risk of case, 21.3% lower, RR 0.79, p < 0.001, high D levels 2,601 of 32,712 (8.0%), low D levels 5,011 of 39,485 (12.7%), adjusted, OR converted to RR, multivariable >75 nmol/L vs. <30 nmol/L. risk of case, 8.7% lower, RR 0.91, p = 0.004, OR converted to RR, supplementation with drops (more common in this study). risk of case, 22.1% higher, RR 1.22, p < 0.001, OR converted to RR, supplementation with tablets. Israel et al., 9/10/2020, retrospective, population-based cohort, Israel, Middle East, preprint, 8 authors. |
| Submit Corrections or Comments |
| Levels | Meltzer et al., JAMA network open, 3:9, doi:10.1001/jamanetworkopen.2020.19722 (Peer Reviewed) | cases, ↓43.5%, p=0.02 | Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results |
| Details Retrospective 489 patients showing 44% lower risk for COVID-19 with vitamin D sufficiency, relative risk RR = 0.56, p = 0.02. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Meltzer et al., JAMA network open, 3:9, doi:10.1001/jamanetworkopen.2020.19722 (Peer Reviewed) |
| Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results |
Retrospective 489 patients showing 44% lower risk for COVID-19 with vitamin D sufficiency, relative risk RR = 0.56, p = 0.02. 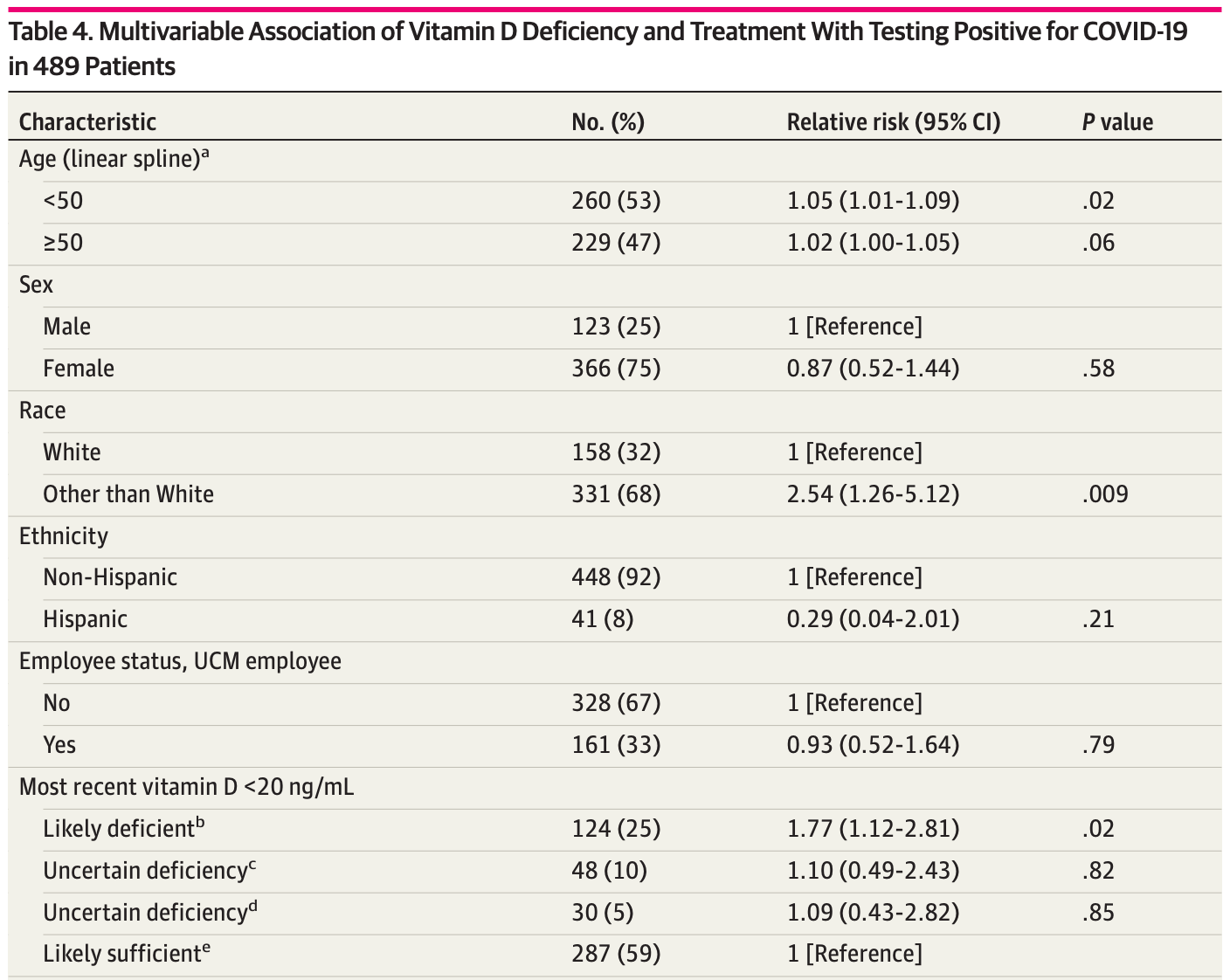 risk of case, 43.5% lower, RR 0.56, p = 0.02, high D levels 39 of 317 (12.3%), low D levels 32 of 172 (18.6%), adjusted, >20ng/mL. Meltzer et al., 9/3/2020, retrospective, USA, North America, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Late | Castillo et al., Journal of Steroid Biochemistry and Molecular Biology, 203, October 2020, doi:10.1016/j.jsbmb.2020.105751 (Peer Reviewed) | death, ↓85.4%, p=0.11 | Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study |
| Details RCT on calcifediol (25-hydroxyvitamin D) treatment for hospitalized COVID-19 patients showing significantly reduced intensive care unit admissions. All patients received standard care including HCQ+AZ. Significantly lower ICU admission .. |
| Details Source PDF Late treatment study Late treatment study |
| Castillo et al., Journal of Steroid Biochemistry and Molecular Biology, 203, October 2020, doi:10.1016/j.jsbmb.2020.105751 (Peer Reviewed) |
| Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study |
RCT on calcifediol (25-hydroxyvitamin D) treatment for hospitalized COVID-19 patients showing significantly reduced intensive care unit admissions. All patients received standard care including HCQ+AZ. Significantly lower ICU admission with the addition of calcifediol - adjusted odds ratio 0.03 [0.003-0.25]. No deaths for calcifediol (0/50), 2 deaths for SOC (2/26).For additional analysis see [1]. risk of death, 85.4% lower, RR 0.15, p = 0.11, treatment 0 of 50 (0.0%), control 2 of 26 (7.7%), relative risk is not 0 because of continuity correction due to zero events. risk of ICU admission, 94.2% lower, RR 0.06, p = 0.008, treatment 50, control 26, OR converted to RR. Castillo et al., 8/29/2020, Randomized Controlled Trial, Spain, Europe, peer-reviewed, 7 authors, dosage calcifediol 0.5mg day 1, 0.27mg day 3, 0.27mg day 7, and then weekly until discharge or ICU admission. |
| Submit Corrections or Comments |
| Levels | Mardani et al., Virus Research, doi:10.1016/j.virusres.2020.198148 (Peer Reviewed) | Association of vitamin D with the modulation of the disease severity in COVID-19 |
| Details Prospective study of 123 outpatients in Iran, showing mortality associated with significantly lower vitamin D levels. IR.SBMU.RETECH.REC.1399.131. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Mardani et al., Virus Research, doi:10.1016/j.virusres.2020.198148 (Peer Reviewed) |
| Association of vitamin D with the modulation of the disease severity in COVID-19 |
Prospective study of 123 outpatients in Iran, showing mortality associated with significantly lower vitamin D levels. IR.SBMU.RETECH.REC.1399.131. 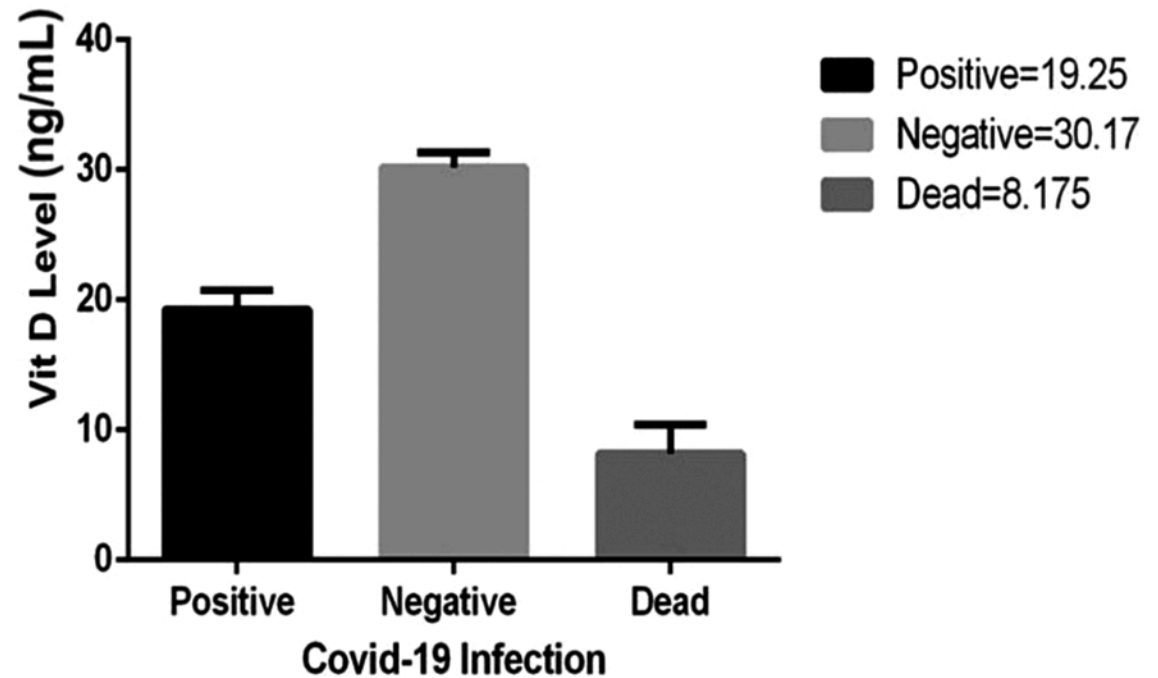 Mardani et al., 8/28/2020, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Baktash et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-138712 (Peer Reviewed) | death, ↓28.6%, p=0.50 | Vitamin D status and outcomes for hospitalised older patients with COVID-19 |
| Details Prospective study of 105 hospitalized patients, showing lower vitamin D levels in the COVID-19 positive group (27.0 nmol/L vs 52.0 nmol/L, p=0.0008), and non-statistically significant higher mortality with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Baktash et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-138712 (Peer Reviewed) |
| Vitamin D status and outcomes for hospitalised older patients with COVID-19 |
Prospective study of 105 hospitalized patients, showing lower vitamin D levels in the COVID-19 positive group (27.0 nmol/L vs 52.0 nmol/L, p=0.0008), and non-statistically significant higher mortality with vitamin D deficiency. 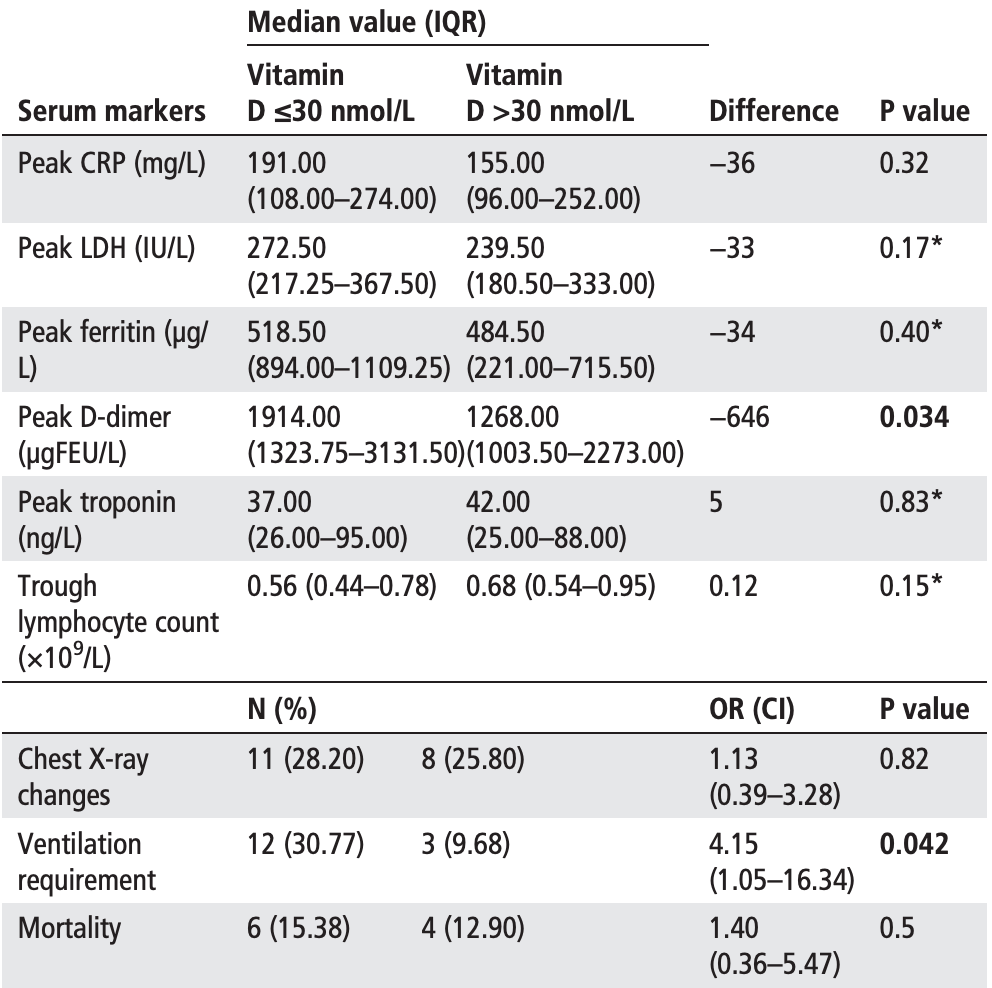 risk of death, 28.6% lower, RR 0.71, p = 0.50, high D levels 4 of 31 (12.9%), low D levels 6 of 39 (15.4%), adjusted, >30nmol/L. Baktash et al., 8/27/2020, prospective, United Kingdom, Europe, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Review | Xu et al., Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5 (Review) (Peer Reviewed) | review | The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19 |
| Details Review of vitamin D for the prevention and treatment of COVID-19, focusing on preventing SARS-CoV-2 infection, acting as an immunosuppressant inhibiting cytokine release syndrome, and preventing loss of neural sensation by stimulating exp.. |
| Details Source PDF Review Review |
| Xu et al., Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5 (Review) (Peer Reviewed) |
| The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19 |
Review of vitamin D for the prevention and treatment of COVID-19, focusing on preventing SARS-CoV-2 infection, acting as an immunosuppressant inhibiting cytokine release syndrome, and preventing loss of neural sensation by stimulating expression of neurotrophins like Nerve Growth Factor (NGF). 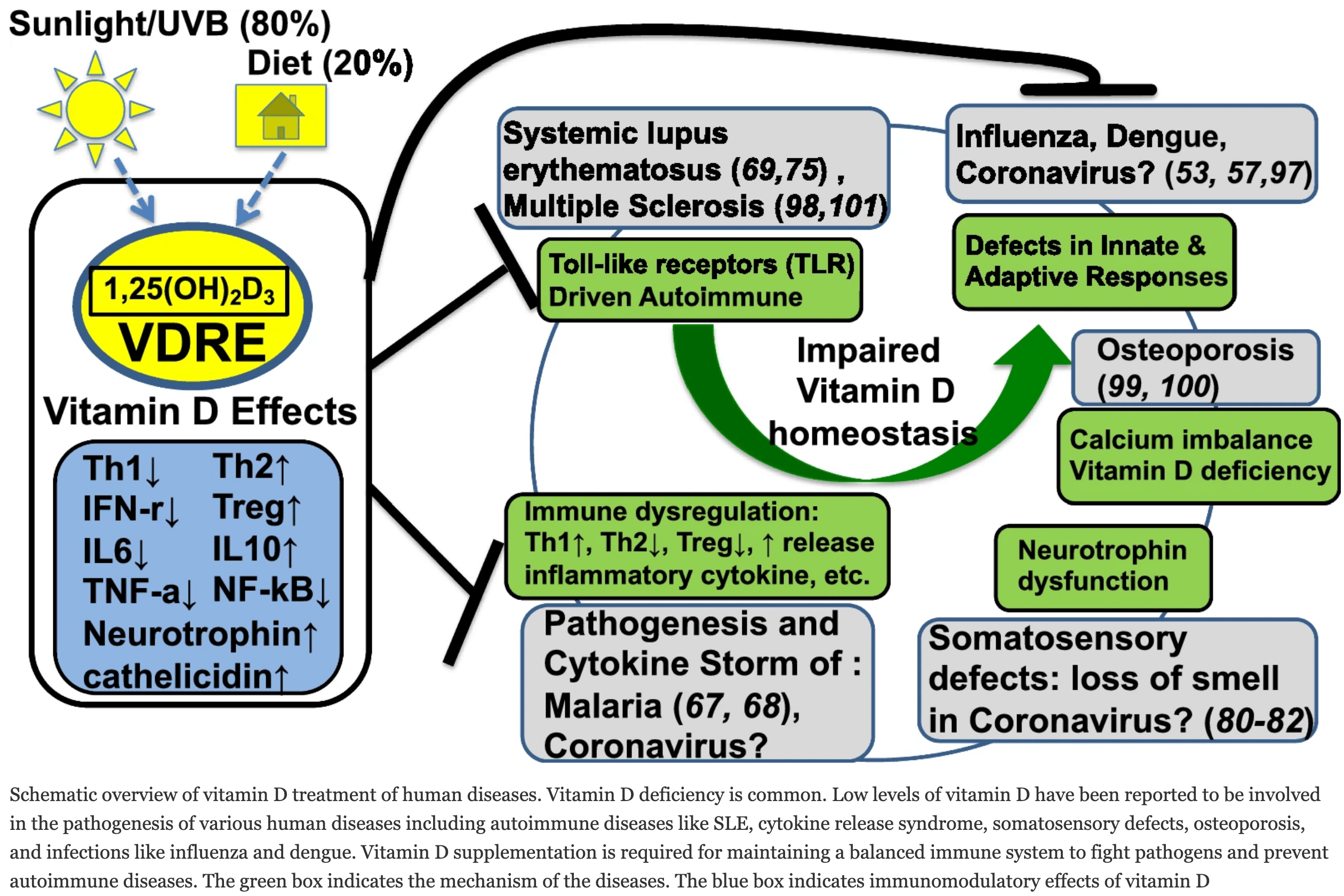 Xu et al., 8/26/2020, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Early | Afshar et al., Journal of Contemporary Medical Sciences, 10.22317/jcms.v6i4.822 (Peer Reviewed) | Suggested role of Vitamin D supplementation in COVID-19 severity |
| Details Brief report noting that there was a dramatic and complete resolution of ICU admissions after adding routine vitamin D supplementation to standard of care. |
| Details Source PDF Early treatment study Early treatment study |
| Afshar et al., Journal of Contemporary Medical Sciences, 10.22317/jcms.v6i4.822 (Peer Reviewed) |
| Suggested role of Vitamin D supplementation in COVID-19 severity |
| Brief report noting that there was a dramatic and complete resolution of ICU admissions after adding routine vitamin D supplementation to standard of care. Afshar et al., 8/26/2020, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Hastie et al., Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14:4, 561–565, doi:10.1016/j.dsx.2020.04.050 (Peer Reviewed) | death, ↓17.4%, p=0.31 | Vitamin D concentrations and COVID-19 infection in UK Biobank |
| Details Database analysis of 341,484 patients in the UK with 656 hospitalized confirmed COVID-19 patients and 203 deaths, not showing a statistically significant difference after adjustment. Since adjustment factors may be correlated with vitamin.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Hastie et al., Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14:4, 561–565, doi:10.1016/j.dsx.2020.04.050 (Peer Reviewed) |
| Vitamin D concentrations and COVID-19 infection in UK Biobank |
Database analysis of 341,484 patients in the UK with 656 hospitalized confirmed COVID-19 patients and 203 deaths, not showing a statistically significant difference after adjustment. Since adjustment factors may be correlated with vitamin D deficiency, the extent of any causal contribution of both vitamin D and the adjustment factors is unclear.There was an ~10 year time period between baseline 25(OH)D measurement and COVID-19 infection, with 84% concordance for a subsample with measurements ~4.3 years later. Vitamin D levels may change significantly across seasons and years. People that discovered they had low vitamin D levels may have been encouraged to take steps to correct the deficiency.Davies et al. raise a number of concerns with this study [1], reporting that it lacked power, suffered low precision and high bias, used flawed models, and contained many serious statistical errors. 1. Mislabelled data artificially inflated the control set, creating an illusion of high power & precision in an underpowered data set study, 2. Logistic regression violated multiple prerequisite conditions, creating biased results and a further reduction of power (overfit, over-adjusted, poor variable types, and poor handling), and 3. Unreliable data in the logistic regressions caused regression dilution bias, bias amplification, and further loss of power and precision.See also [2]. risk of death, 17.4% lower, RR 0.83, p = 0.31, adjusted, multivariable Cox. risk of hospitalization, 9.1% lower, RR 0.91, p = 0.40, adjusted, multivariable Cox. Hastie et al., 8/26/2020, retrospective, population-based cohort, database analysis, United Kingdom, Europe, peer-reviewed, 14 authors. |
| Submit Corrections or Comments |
| Early | Espitia-Hernandez et al., Biomedical Research, 31:5 (Peer Reviewed) | recov. time, ↓70.0%, p<0.0001 | Effects of Ivermectin-azithromycin-cholecalciferol combined therapy on COVID-19 infected patients: A proof of concept study |
| Details Small study with 28 patients treated with ivermectin + AZ + cholecalciferol and 7 control patients. All treated patients were PCR- at day 10 while all control patients remained PCR+. The mean duration of symptoms was 3 days in the treatm.. |
| Details Source PDF Early treatment study Early treatment study |
| Espitia-Hernandez et al., Biomedical Research, 31:5 (Peer Reviewed) |
| Effects of Ivermectin-azithromycin-cholecalciferol combined therapy on COVID-19 infected patients: A proof of concept study |
Small study with 28 patients treated with ivermectin + AZ + cholecalciferol and 7 control patients.All treated patients were PCR- at day 10 while all control patients remained PCR+. The mean duration of symptoms was 3 days in the treatment group and 10 days in the control group. recovery time, 70.0% lower, relative time 0.30, p < 0.001, treatment 28, control 7. risk of viral+ at day 10, 97.2% lower, RR 0.03, p < 0.001, treatment 0 of 28 (0.0%), control 7 of 7 (100.0%), relative risk is not 0 because of continuity correction due to zero events. Espitia-Hernandez et al., 8/15/2020, retrospective, Mexico, North America, peer-reviewed, 5 authors, dosage 8,000IU daily, 4000IU twice daily for 30 days, this trial uses multiple treatments in the treatment arm (combined with ivermectin and azithromycin) - results of individual treatments may vary. |
| Submit Corrections or Comments |
| Levels | Im et al., Int. J. Infect. Dis., doi:10.1016/j.ijid.2020.08.018 (Peer Reviewed) | cases, ↓73.1%, p=0.0003 | Nutritional status of patients with COVID-19 |
| Details Nutrient study of 50 hospitalized COVID-19 patients in South Korea showing that 76% of patients were vitamin D deficient. Comparison with 150 matched controls showed a higher probability of cases with vitamin D deficiency. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Im et al., Int. J. Infect. Dis., doi:10.1016/j.ijid.2020.08.018 (Peer Reviewed) |
| Nutritional status of patients with COVID-19 |
Nutrient study of 50 hospitalized COVID-19 patients in South Korea showing that 76% of patients were vitamin D deficient. Comparison with 150 matched controls showed a higher probability of cases with vitamin D deficiency. 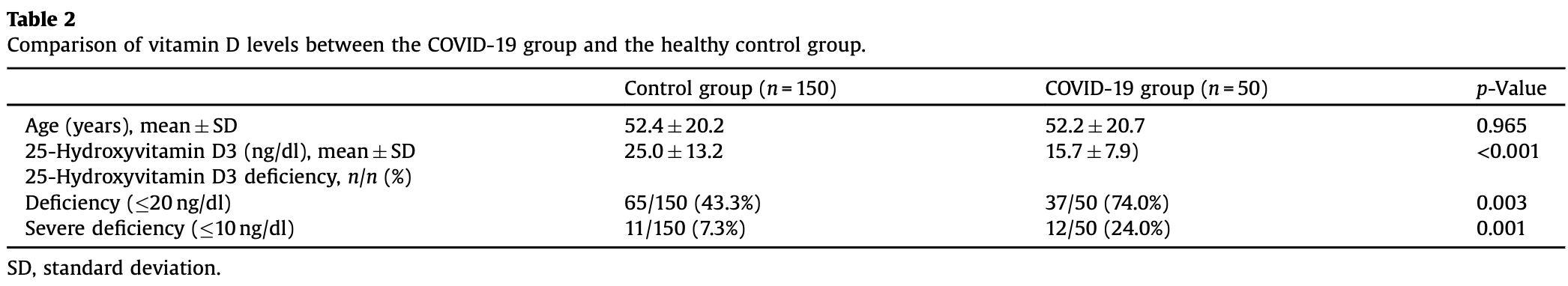 risk of case, 73.1% lower, RR 0.27, p < 0.001, high D levels 13 of 50 (26.0%) cases, 85 of 150 (56.7%) controls, case control OR. Im et al., 8/11/2020, retrospective, South Korea, Asia, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Levels | Carpagnano et al., J. Endocrinol. Invest., 2020, Aug 9, 1-7, doi:10.1007/s40618-020-01370-x (Peer Reviewed) | death, ↓70.6%, p=0.05 | Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19 |
| Details Retrospective study 42 patients with acute respiratory failure, 81% with low vitamin D levels. After 10 days, patients with severe vitamin D deficiency had a 50% probability of dying, while those with vitamin D ≥ 10 ng/mL had a 5% mortal.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Carpagnano et al., J. Endocrinol. Invest., 2020, Aug 9, 1-7, doi:10.1007/s40618-020-01370-x (Peer Reviewed) |
| Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19 |
Retrospective study 42 patients with acute respiratory failure, 81% with low vitamin D levels.After 10 days, patients with severe vitamin D deficiency had a 50% probability of dying, while those with vitamin D ≥ 10 ng/mL had a 5% mortality risk, RR 0.1, p = 0.019. 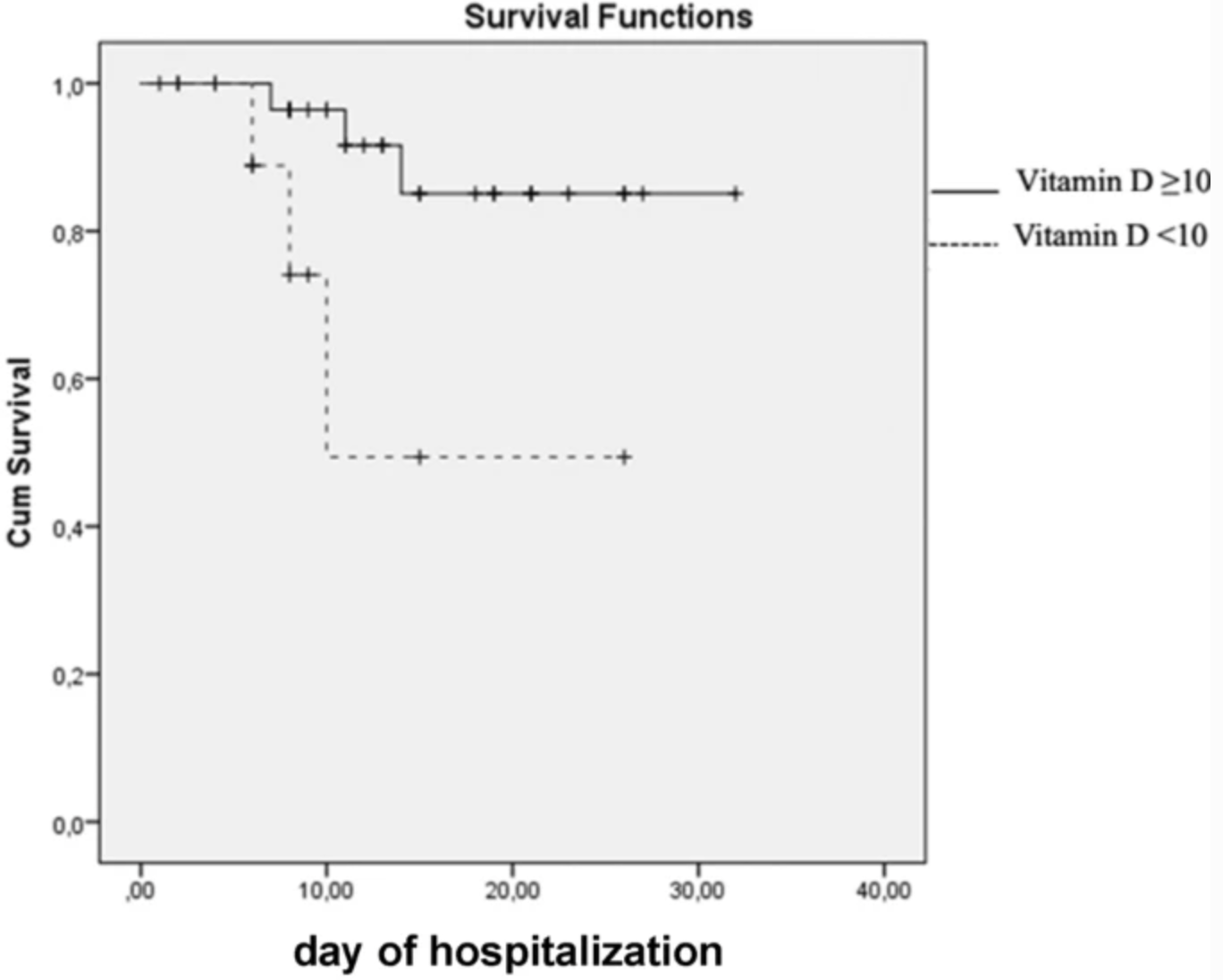 risk of death at day 26, 70.6% lower, RR 0.29, p = 0.05, high D levels 5 of 34 (14.7%), low D levels 4 of 8 (50.0%), >30 ng/mL. risk of death at day 10, 90.0% lower, RR 0.10, p = 0.02, high D levels 2 of 34 (5.9%), low D levels 4 of 8 (50.0%), adjusted, >30 ng/mL. Carpagnano et al., 8/9/2020, retrospective, Italy, Europe, peer-reviewed, 10 authors. |
| Submit Corrections or Comments |
| Levels | Merzon et al., The FEBS Journal, doi:doi.org/10.1111/febs.15495 (Peer Reviewed) | hosp., ↓46.4%, p=0.06 | Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: an Israeli population‐based study |
| Details Analysis of 7,807 patients finding that low vitamin D levels are correlated with increased risk of cases and hospitalization. Adjusted odds ratio OR for sufficient vitamin D level for cases 0.69, p < 0.001, and for hospitalization 0.51, p.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Merzon et al., The FEBS Journal, doi:doi.org/10.1111/febs.15495 (Peer Reviewed) |
| Low plasma 25(OH) vitamin D level is associated with increased risk of COVID‐19 infection: an Israeli population‐based study |
Analysis of 7,807 patients finding that low vitamin D levels are correlated with increased risk of cases and hospitalization. Adjusted odds ratio OR for sufficient vitamin D level for cases 0.69, p < 0.001, and for hospitalization 0.51, p = 0.061. risk of hospitalization, 46.4% lower, RR 0.54, p = 0.06, high D levels 79, low D levels 703, OR converted to RR, >30ng/mL. risk of case, 28.4% lower, RR 0.72, p < 0.001, high D levels 1,139, low D levels 6,668, OR converted to RR, >30ng/mL. Merzon et al., 7/23/2020, retrospective, Israel, Middle East, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| Levels | Lansiaux et al., Spat. Spatiotemporal Epidemiol, doi:10.1016/j.sste.2020.100362 (Peer Reviewed) | Covid-19 and vit-d: Disease mortality negatively correlates with sunlight exposure |
| Details Analysis of COVID-19 mortality rate and sunlight exposure finding a correlation that suggests a protective effect of sunlight exposure. In continental metropolitan France, average annual sunlight hours were found to be significantly cor.. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Lansiaux et al., Spat. Spatiotemporal Epidemiol, doi:10.1016/j.sste.2020.100362 (Peer Reviewed) |
| Covid-19 and vit-d: Disease mortality negatively correlates with sunlight exposure |
| Analysis of COVID-19 mortality rate and sunlight exposure finding a correlation that suggests a protective effect of sunlight exposure.In continental metropolitan France, average annual sunlight hours were found to be significantly correlated to the COVID-19 mortality rate, with a Pearson coefficient of -0.636. Lansiaux et al., 7/23/2020, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Late | Krishnan et al., J Clin Anesth., doi:10.1016/j.jclinane.2020.110005 (Peer Reviewed) | death, ↓19.0%, p=0.42 | Clinical comorbidities, characteristics, and outcomes of mechanically ventilated patients in the State of Michigan with SARS-CoV-2 pneumonia |
| Details Retrospective 152 mechanically ventilated patients in the USA showing unadjusted lower mortality with vitamin C, vitamin D, HCQ, and zinc treatment, statistically significant only for vitamin C. |
| Details Source PDF Late treatment study Late treatment study |
| Krishnan et al., J Clin Anesth., doi:10.1016/j.jclinane.2020.110005 (Peer Reviewed) |
| Clinical comorbidities, characteristics, and outcomes of mechanically ventilated patients in the State of Michigan with SARS-CoV-2 pneumonia |
Retrospective 152 mechanically ventilated patients in the USA showing unadjusted lower mortality with vitamin C, vitamin D, HCQ, and zinc treatment, statistically significant only for vitamin C. risk of death, 19.0% lower, RR 0.81, p = 0.42, treatment 8 of 16 (50.0%), control 84 of 136 (61.8%). Excluded in after exclusion results of meta analysis: unadjusted results with no group details. Krishnan et al., 7/20/2020, retrospective, USA, North America, peer-reviewed, 13 authors, dosage not specified. |
| Submit Corrections or Comments |
| PrEPPEP | Jolliffe et al., medRxiv, doi:10.1101/2020.07.14.20152728 (Preprint) (meta analysis) | meta-analysis | Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of aggregate data from randomised controlled trials |
| Details Meta analysis of 40 RCTs showing that vitamin D supplementation is safe and reduced risk of acute respiratory infections, odds ratio OR 0.89 [0.81-0.98]. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Jolliffe et al., medRxiv, doi:10.1101/2020.07.14.20152728 (Preprint) (meta analysis) |
| Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of aggregate data from randomised controlled trials |
Meta analysis of 40 RCTs showing that vitamin D supplementation is safe and reduced risk of acute respiratory infections, odds ratio OR 0.89 [0.81-0.98]. 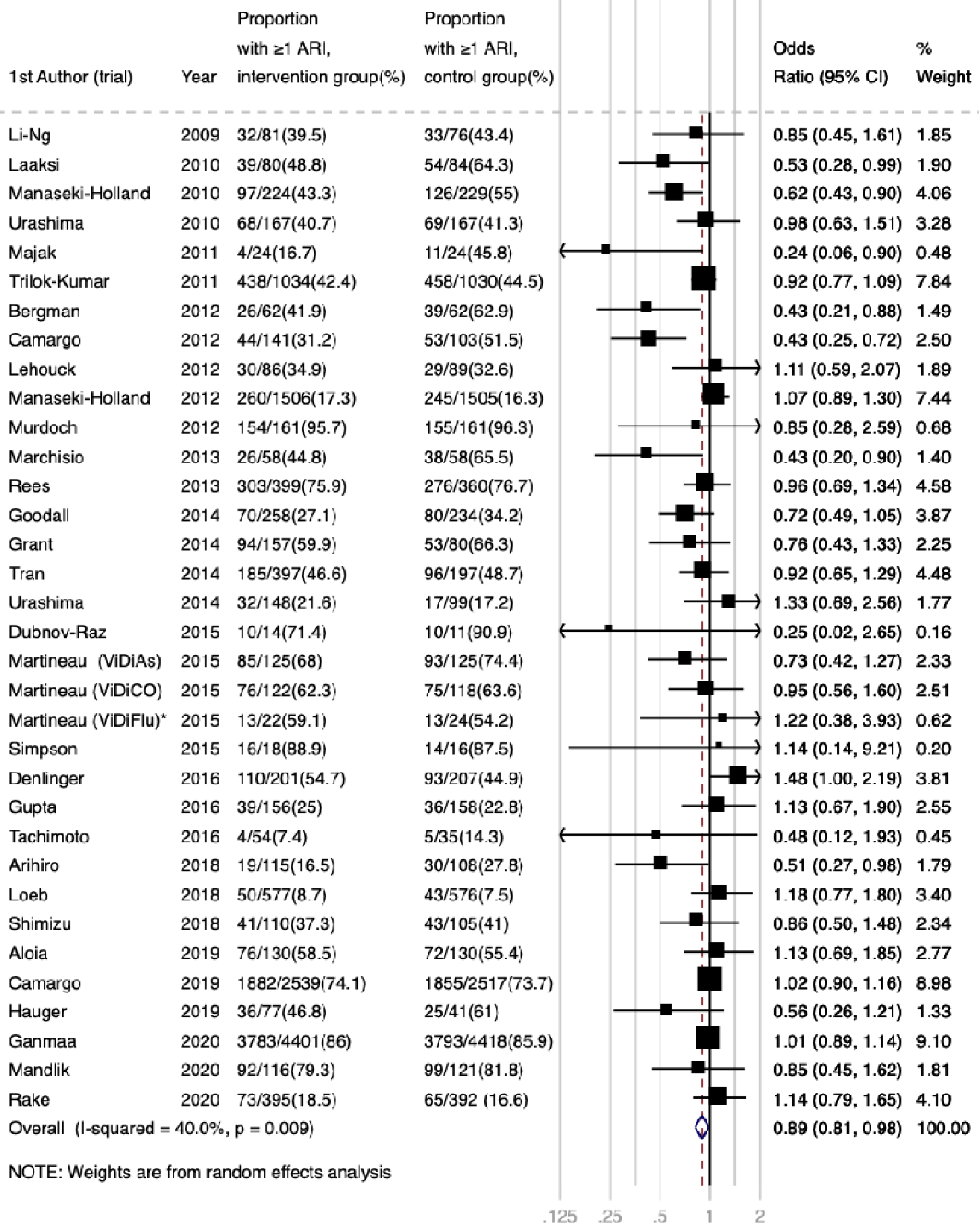 Jolliffe et al., 7/17/2020, preprint, 41 authors. |
| Submit Corrections or Comments |
| Levels | Hamza et al., Pakistan Journal of Medical & Health Sciences (Peer Reviewed) | Role of Vitamin D in Pathogenesis and Severity of Coronavirus Disease 2019 (COVID-19) Infection |
| Details Prospective study of 168 patients in Pakistan reporting an association between vitamin D deficiency and symptomatic cases. Details of the association are not provided. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Hamza et al., Pakistan Journal of Medical & Health Sciences (Peer Reviewed) |
| Role of Vitamin D in Pathogenesis and Severity of Coronavirus Disease 2019 (COVID-19) Infection |
Prospective study of 168 patients in Pakistan reporting an association between vitamin D deficiency and symptomatic cases. Details of the association are not provided. 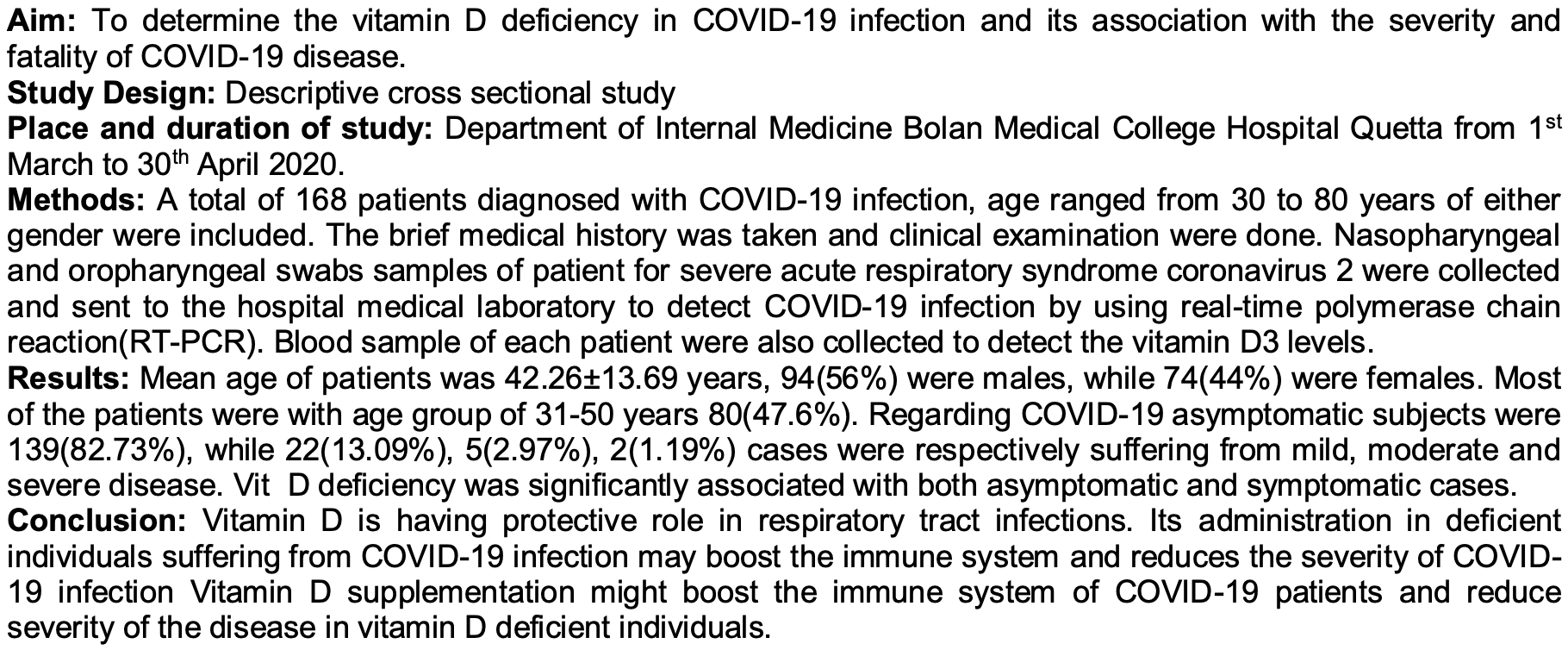 Hamza et al., 6/30/2020, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | Faul et al., Irish Medical Journal, 113:5, 84 (Peer Reviewed) | ventilation, ↓69.0%, p=0.03 | Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection |
| Details Analysis of 33 hospitalized COVID-19 patients with respiratory failure requiring FiO2 greater than 0.4. Intubation hazard ratio for vitamin D sufficiency HR 0.31, p = 0.03. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Faul et al., Irish Medical Journal, 113:5, 84 (Peer Reviewed) |
| Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection |
Analysis of 33 hospitalized COVID-19 patients with respiratory failure requiring FiO2 greater than 0.4.Intubation hazard ratio for vitamin D sufficiency HR 0.31, p = 0.03. risk of mechanical ventilation, 69.0% lower, RR 0.31, p = 0.03, high D levels 4 of 21 (19.0%), low D levels 8 of 12 (66.7%), adjusted, >30nmol/L. Faul et al., 6/30/2020, retrospective, Ireland, Europe, peer-reviewed, 9 authors. |
| Submit Corrections or Comments |
| Levels | Panagiotou et al., medRxiv, doi:10.1101/2020.06.21.20136903 (Preprint) | ICU, ↓52.0%, p=0.02 | Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice |
| Details Retrospective analysis 134 hospitalized patients. 19% of ICU patients had 25(OH)D levels > 50 nmol/L vs. 39.1% of non-ICU patients, p=0.02 |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Panagiotou et al., medRxiv, doi:10.1101/2020.06.21.20136903 (Preprint) |
| Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice |
Retrospective analysis 134 hospitalized patients. 19% of ICU patients had 25(OH)D levels > 50 nmol/L vs. 39.1% of non-ICU patients, p=0.02 risk of ICU admission, 52.0% lower, RR 0.48, p = 0.02, high D levels 8 of 44 (18.2%), low D levels 34 of 90 (37.8%), >50nmol/L. Panagiotou et al., 6/30/2020, retrospective, United Kingdom, Europe, preprint, 12 authors. |
| Submit Corrections or Comments |
| Levels | Mendy et al., medRxiv, doi:10.1101/2020.06.25.20137323 (Preprint) | death, ↓7.0%, p=0.89 | Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients |
| Details Retrospective 689 patients showing vitamin D deficiency associated with hospitalization and disease severity. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Mendy et al., medRxiv, doi:10.1101/2020.06.25.20137323 (Preprint) |
| Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients |
Retrospective 689 patients showing vitamin D deficiency associated with hospitalization and disease severity. 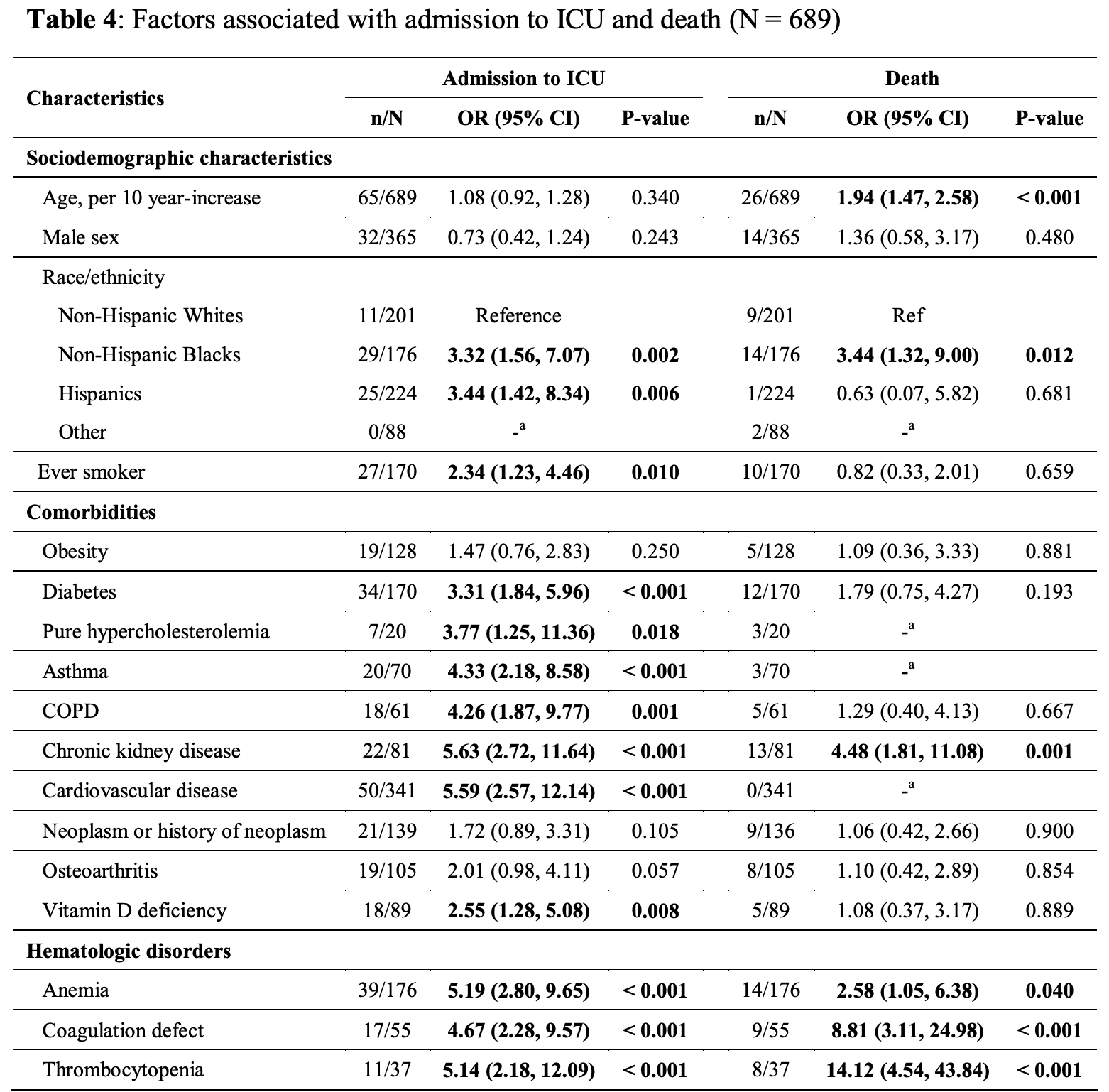 risk of death, 7.0% lower, RR 0.93, p = 0.89, high D levels 21 of 600 (3.5%), low D levels 5 of 89 (5.6%), OR converted to RR. risk of death/ICU, 16.7% lower, RR 0.83, p < 0.001, high D levels 68 of 600 (11.3%), low D levels 23 of 89 (25.8%), OR converted to RR. risk of ICU admission, 55.3% lower, RR 0.45, p = 0.008, high D levels 47 of 600 (7.8%), low D levels 18 of 89 (20.2%), OR converted to RR. risk of hospitalization, 15.1% lower, RR 0.85, p < 0.001, high D levels 171 of 600 (28.5%), low D levels 45 of 89 (50.6%), OR converted to RR. Mendy et al., 6/27/2020, retrospective, USA, North America, preprint, 4 authors. |
| Submit Corrections or Comments |
| Levels | Whittemore et al., American Journal of Infection Control, doi:10.1016/j.ajic.2020.06.193 (Peer Reviewed) | COVID-19 fatalities, latitude, sunlight, and vitamin D |
| Details Analysis of 88 countries, showing a significant correlation between death rates and latitude, suggesting that sunlight exposure and vitamin D levels influence mortality. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Whittemore et al., American Journal of Infection Control, doi:10.1016/j.ajic.2020.06.193 (Peer Reviewed) |
| COVID-19 fatalities, latitude, sunlight, and vitamin D |
Analysis of 88 countries, showing a significant correlation between death rates and latitude, suggesting that sunlight exposure and vitamin D levels influence mortality. 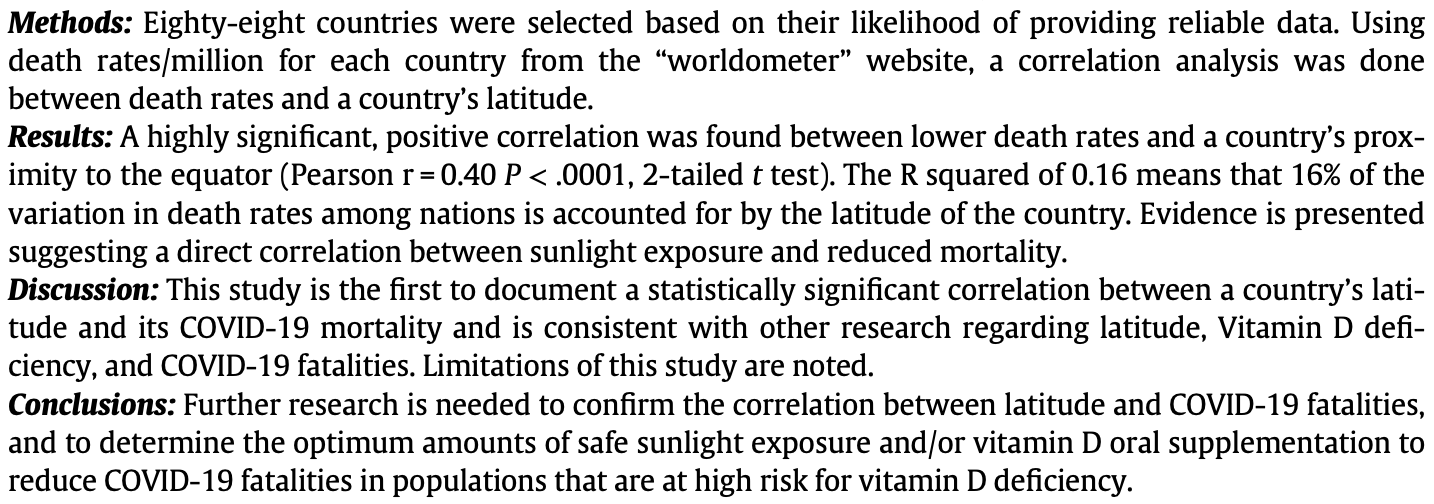 Whittemore et al., 6/26/2020, peer-reviewed, 1 author. |
| Submit Corrections or Comments |
| Review | Andrade et al., SciELO preprints, doi:10.1590/SciELOPreprints.839 (Review) (Peer Reviewed) | review | Vitamin A and D deficiencies in the prognosis of respiratory tract infections: A systematic review with perspectives for COVID-19 and a critical analysis on supplementation |
| Details Systematic review showing deficiencies of vitamins A and D negatively affecting the prognosis of respiratory tract infections. |
| Details Source PDF Review Review |
| Andrade et al., SciELO preprints, doi:10.1590/SciELOPreprints.839 (Review) (Peer Reviewed) |
| Vitamin A and D deficiencies in the prognosis of respiratory tract infections: A systematic review with perspectives for COVID-19 and a critical analysis on supplementation |
Systematic review showing deficiencies of vitamins A and D negatively affecting the prognosis of respiratory tract infections. 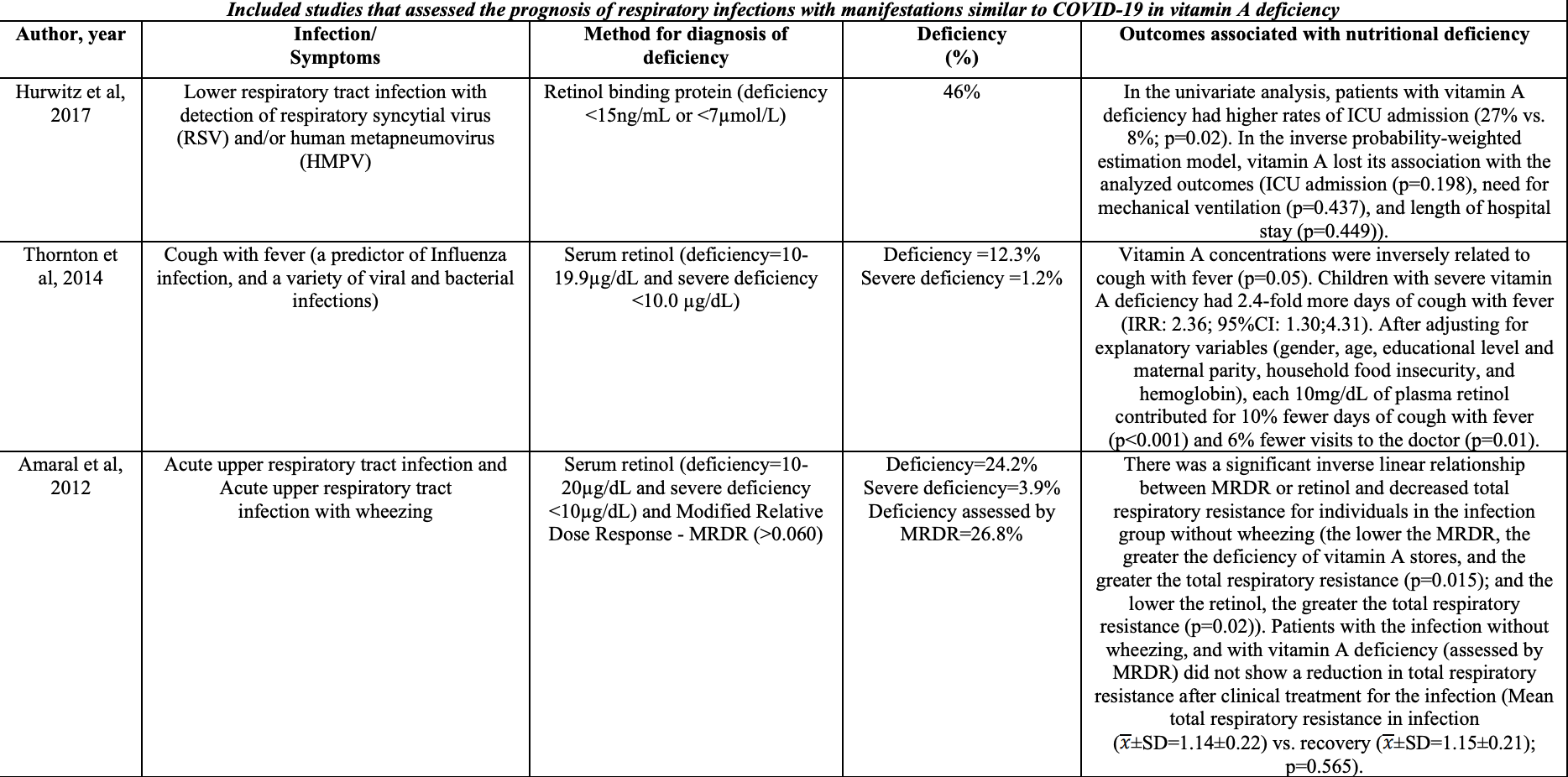 Andrade et al., 6/24/2020, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| In Vitro | Mok et al., bioRxiv, doi:10.1101/2020.06.21.162396 (Preprint) (In Vitro) | in vitro | Calcitriol, the active form of vitamin D, is a promising candidate for COVID-19 prophylaxis |
| Details In Vitro study showing that the active form of Vitamin D, calcitriol, exhibits significant potent activity against SARS-CoV-2. |
| Details Source PDF In Vitro In Vitro |
| Mok et al., bioRxiv, doi:10.1101/2020.06.21.162396 (Preprint) (In Vitro) |
| Calcitriol, the active form of vitamin D, is a promising candidate for COVID-19 prophylaxis |
In Vitro study showing that the active form of Vitamin D, calcitriol, exhibits significant potent activity against SARS-CoV-2. 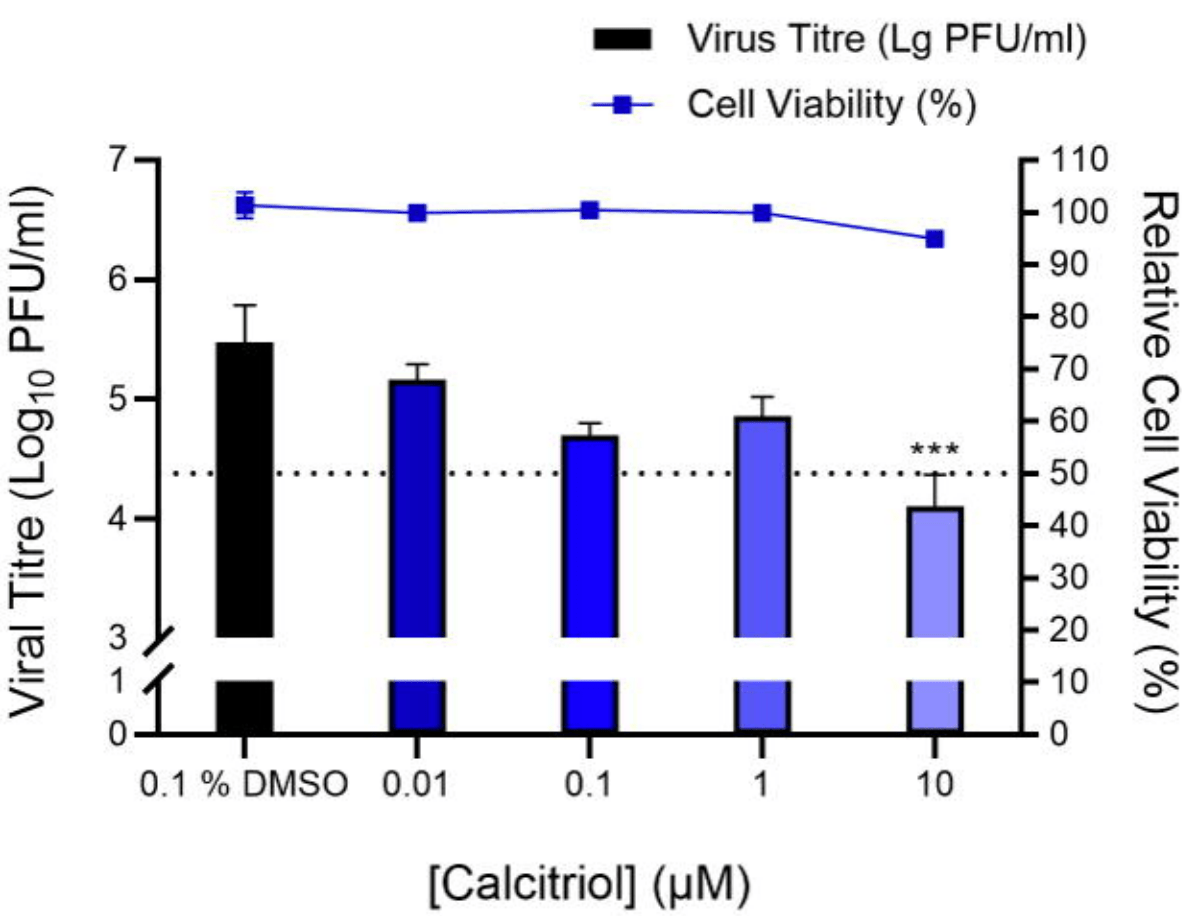 Mok et al., 6/22/2020, preprint, 20 authors. In Vitro studies are an important part of preclinical research, however results may be very different in vivo. |
| Submit Corrections or Comments |
| Levels | Raisi-Estabragh et al., J. Public Health, doi:10.1093/pubmed/fdaa095 (Peer Reviewed) | Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank |
| Details UK Biobank retrospective not finding a significant association between vitamin D levels and the risk of PCR+ after adjustment. Since adjustment factors may be correlated with vitamin D deficiency, the extent of any causal contribution of .. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Raisi-Estabragh et al., J. Public Health, doi:10.1093/pubmed/fdaa095 (Peer Reviewed) |
| Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank |
| UK Biobank retrospective not finding a significant association between vitamin D levels and the risk of PCR+ after adjustment. Since adjustment factors may be correlated with vitamin D deficiency, the extent of any causal contribution of both vitamin D and the adjustment factors is unclear.There was an ~10 year time period between baseline 25(OH)D measurement and COVID-19 infection. Vitamin D levels may change significantly across seasons and years. People that discovered they had low vitamin D levels may have been encouraged to take steps to correct the deficiency. Raisi-Estabragh et al., 6/19/2020, peer-reviewed, 9 authors. |
| Submit Corrections or Comments |
| Levels | Rhodes et al., BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000110 (Peer Reviewed) | COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D |
| Details Analysis of COVID-19 mortality and latitude as of May 18, 2020, showing that latitude was significantly associated with mortality (p=0.031), with an estimated 4.4% [0.4%-8.5%] increase in mortality for each 1° further north. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Rhodes et al., BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000110 (Peer Reviewed) |
| COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D |
Analysis of COVID-19 mortality and latitude as of May 18, 2020, showing that latitude was significantly associated with mortality (p=0.031), with an estimated 4.4% [0.4%-8.5%] increase in mortality for each 1° further north. 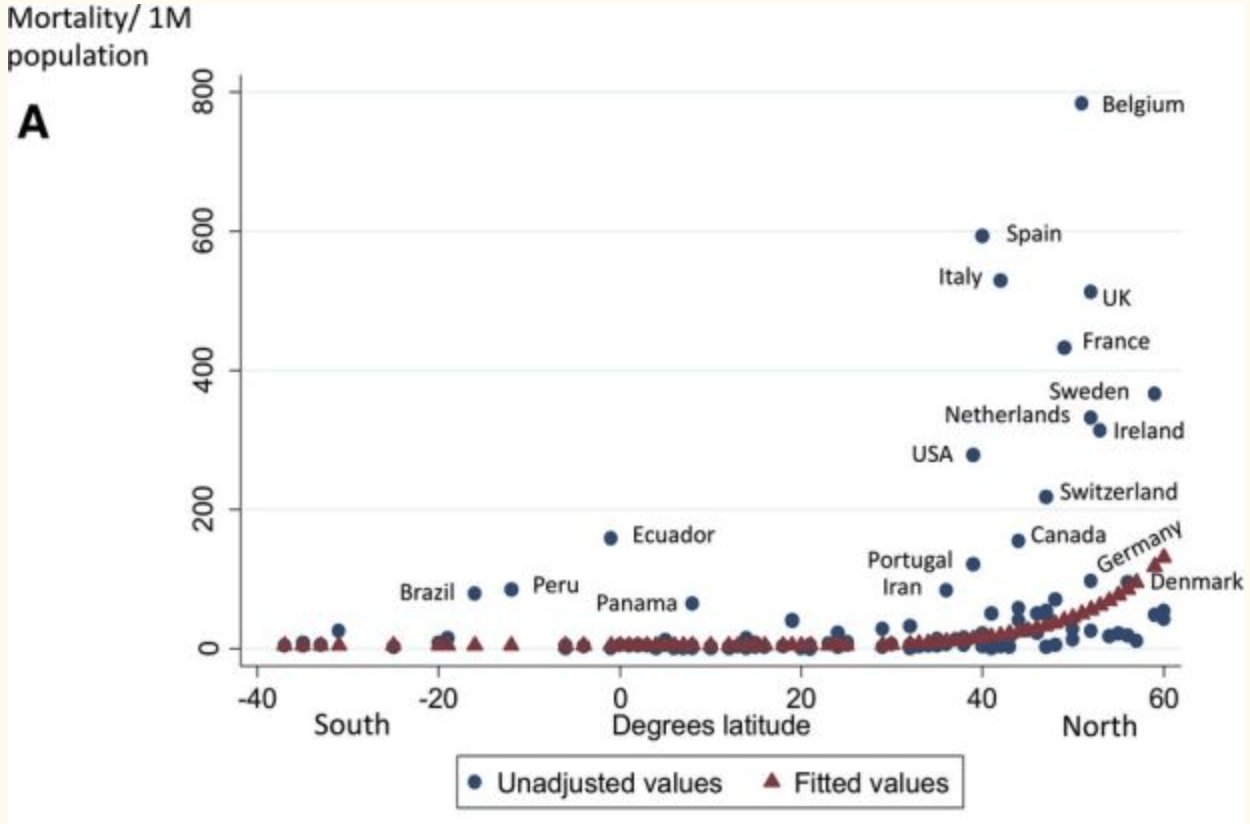 Rhodes et al., 6/14/2020, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Davies et al., medRxiv, doi:10.1101/2020.05.01.20087965 (Preprint) | Evidence Supports a Causal Role for Vitamin D Status in Global COVID-19 Outcomes |
| Details Causal inference analysis of COVID-19 severity and latitude concluding that vitamin D status plays a key role in COVID-19 outcome. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Davies et al., medRxiv, doi:10.1101/2020.05.01.20087965 (Preprint) |
| Evidence Supports a Causal Role for Vitamin D Status in Global COVID-19 Outcomes |
Causal inference analysis of COVID-19 severity and latitude concluding that vitamin D status plays a key role in COVID-19 outcome. 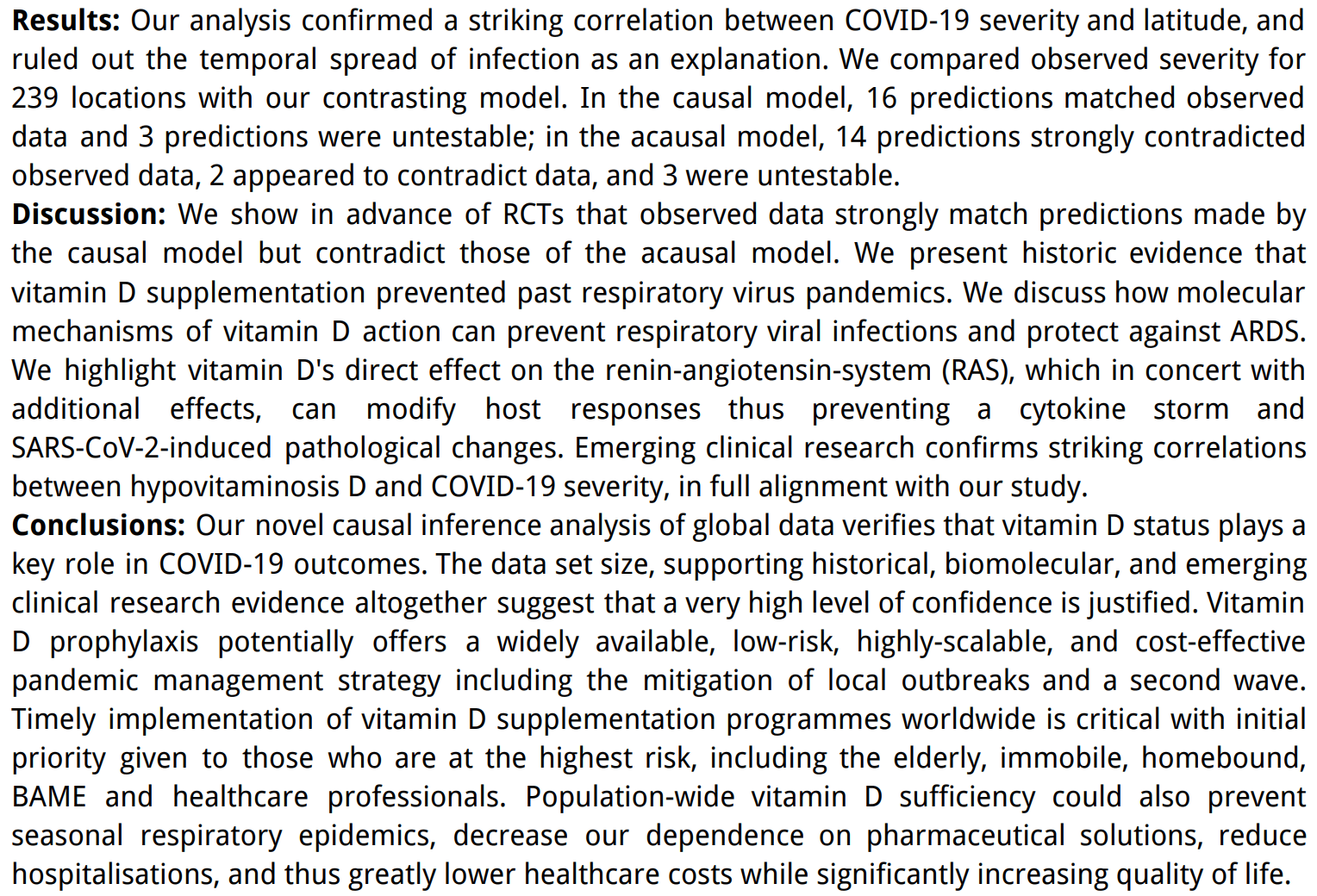 Davies et al., 6/13/2020, preprint, 3 authors. |
| Submit Corrections or Comments |
| Late | Tan et al., Nutrition, doi:10.1016/j.nut.2020.111017 (preprint 6/10/20) (Peer Reviewed) | oxygen, ↓80.5%, p=0.04 | Cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients |
| Details Observational study of 43 patients >= 50 years old, with 17 patients receiving vitamin D, magnesium, and vitamin B12 (DMB); and 26 control patients, showing a significantly lower need for oxygen therapy and ICU admission with treatment. D.. |
| Details Source PDF Late treatment study Late treatment study |
| Tan et al., Nutrition, doi:10.1016/j.nut.2020.111017 (preprint 6/10/20) (Peer Reviewed) |
| Cohort study to evaluate the effect of combination Vitamin D, Magnesium and Vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients |
Observational study of 43 patients >= 50 years old, with 17 patients receiving vitamin D, magnesium, and vitamin B12 (DMB); and 26 control patients, showing a significantly lower need for oxygen therapy and ICU admission with treatment. DMB OR 0.20 [0.04–0.93] for oxygen therapy and/or intensive care support with multivariate analysis. 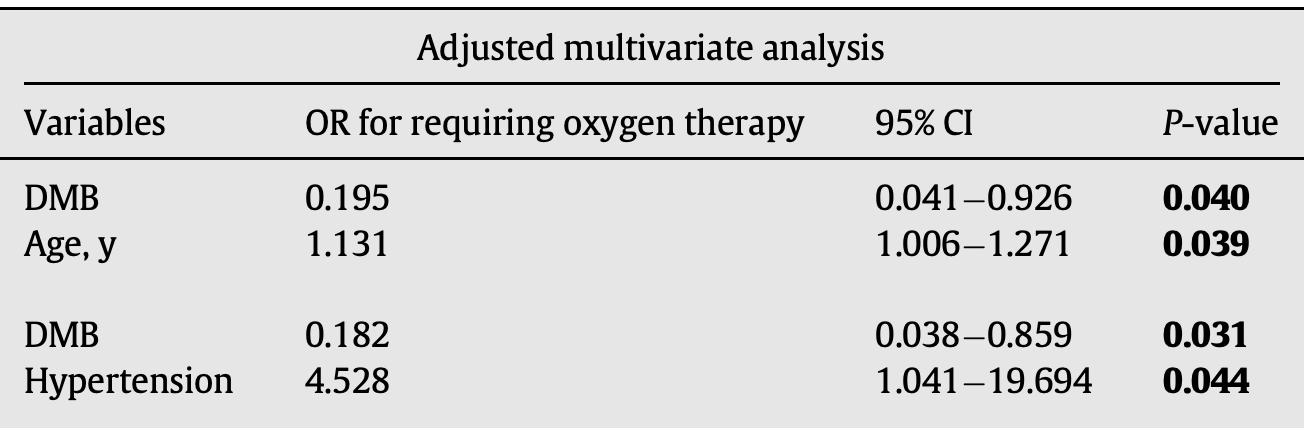 risk of oxygen therapy, 80.5% lower, RR 0.20, p = 0.04, treatment 3 of 17 (17.6%), control 16 of 26 (61.5%), adjusted, multivariate. risk of ICU admission, 80.9% lower, RR 0.19, p = 0.07, treatment 1 of 17 (5.9%), control 8 of 26 (30.8%), no adjusted result available. Tan et al., 6/10/2020, retrospective, Singapore, Asia, peer-reviewed, 14 authors, dosage 1,000IU daily. |
| Submit Corrections or Comments |
| PrEPPEP | Skutsch et al., medRxiv, doi:10.1101/2020.05.25.20112805 (Preprint) | The association of UV with rates of COVID-19 transmission and deaths in Mexico: the possible mediating role of vitamin D |
| Details Analysis of UV, temperature, humidity and COVID-19 in 45 Mexican cities, showing that UV was negatively correlated with rates of transmission (statistically significant) and mortality (not statistically significant). |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Skutsch et al., medRxiv, doi:10.1101/2020.05.25.20112805 (Preprint) |
| The association of UV with rates of COVID-19 transmission and deaths in Mexico: the possible mediating role of vitamin D |
Analysis of UV, temperature, humidity and COVID-19 in 45 Mexican cities, showing that UV was negatively correlated with rates of transmission (statistically significant) and mortality (not statistically significant). 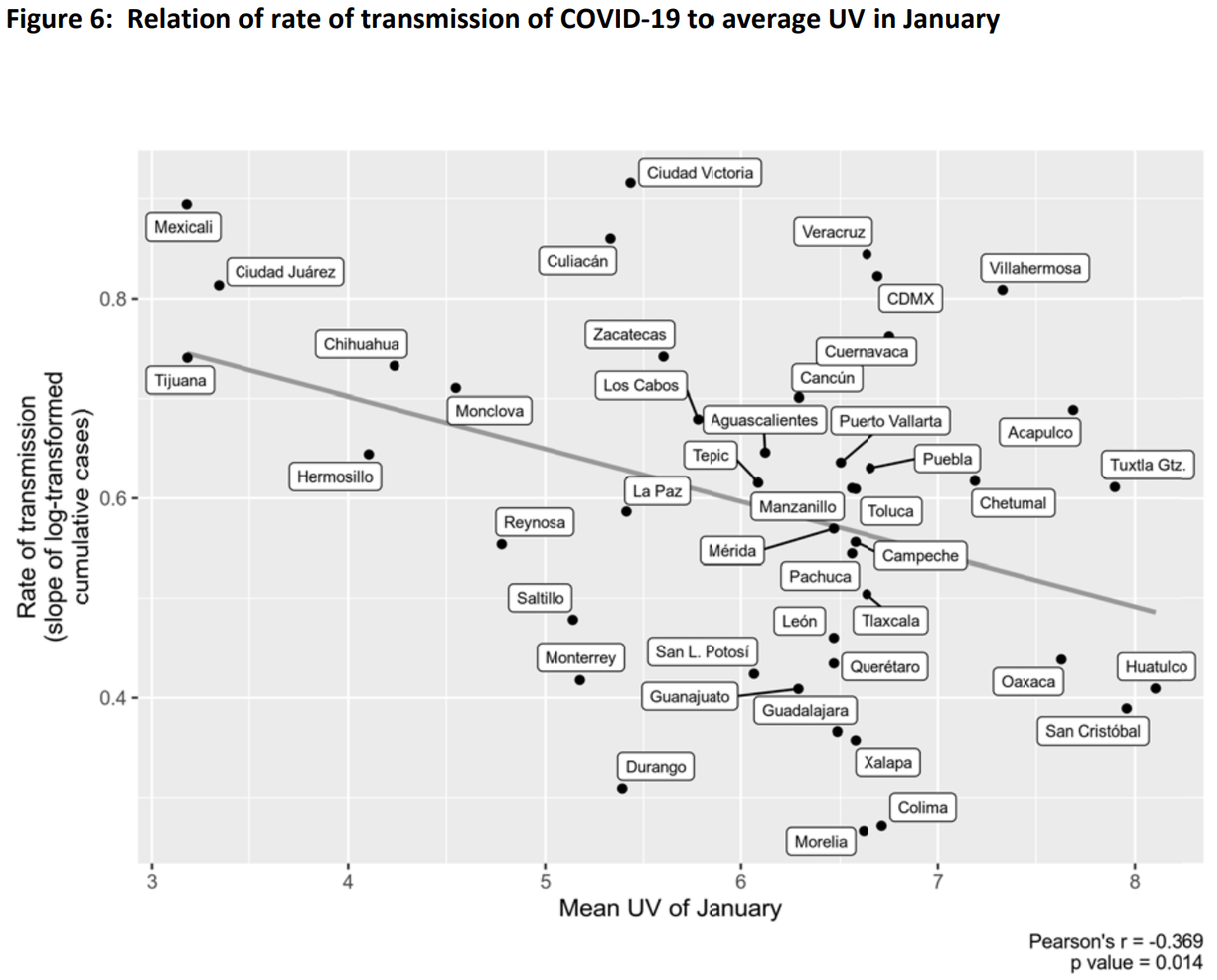 Skutsch et al., 5/27/2020, preprint, 7 authors. |
| Submit Corrections or Comments |
| Levels | Chodick et al., Journal of Travel Medicine, doi:10.1093/jtm/taaa069 (Peer Reviewed) | Angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers are not associated with increased risk of SARS-CoV-2 infection |
| Details Retrospective 14,520 patients in Israel, 1,317 testing positive, showing no significant difference in vitamin D levels (23.6ng/mL and 24.1ng/mL for positive and negative cases respectively). |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Chodick et al., Journal of Travel Medicine, doi:10.1093/jtm/taaa069 (Peer Reviewed) |
| Angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers are not associated with increased risk of SARS-CoV-2 infection |
Retrospective 14,520 patients in Israel, 1,317 testing positive, showing no significant difference in vitamin D levels (23.6ng/mL and 24.1ng/mL for positive and negative cases respectively). 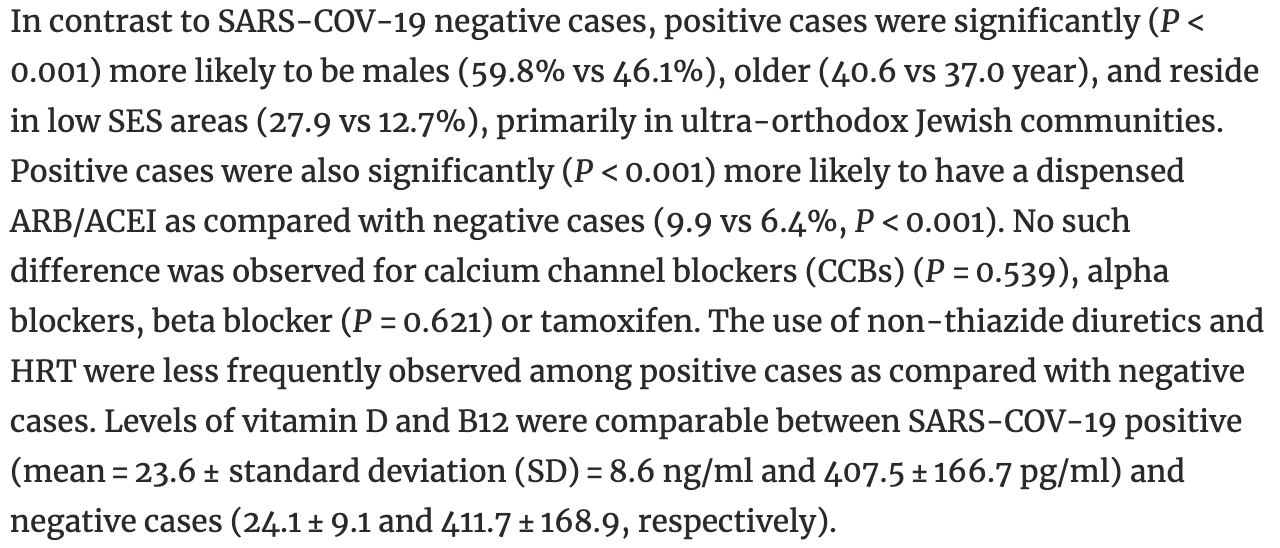 Chodick et al., 5/14/2020, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Levels | D'Avolio et al., Nutrients, 12:5, 1–7, doi:10.3390/nu12051359 (Peer Reviewed) | 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2 |
| Details Retrospective 107 patients in Switzerland showing lower vitamin D levels (11.1 ng/mL) in PCR positive patients compared with negative patients (24.6 ng/mL), p = 0.004. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| D'Avolio et al., Nutrients, 12:5, 1–7, doi:10.3390/nu12051359 (Peer Reviewed) |
| 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2 |
Retrospective 107 patients in Switzerland showing lower vitamin D levels (11.1 ng/mL) in PCR positive patients compared with negative patients (24.6 ng/mL), p = 0.004. 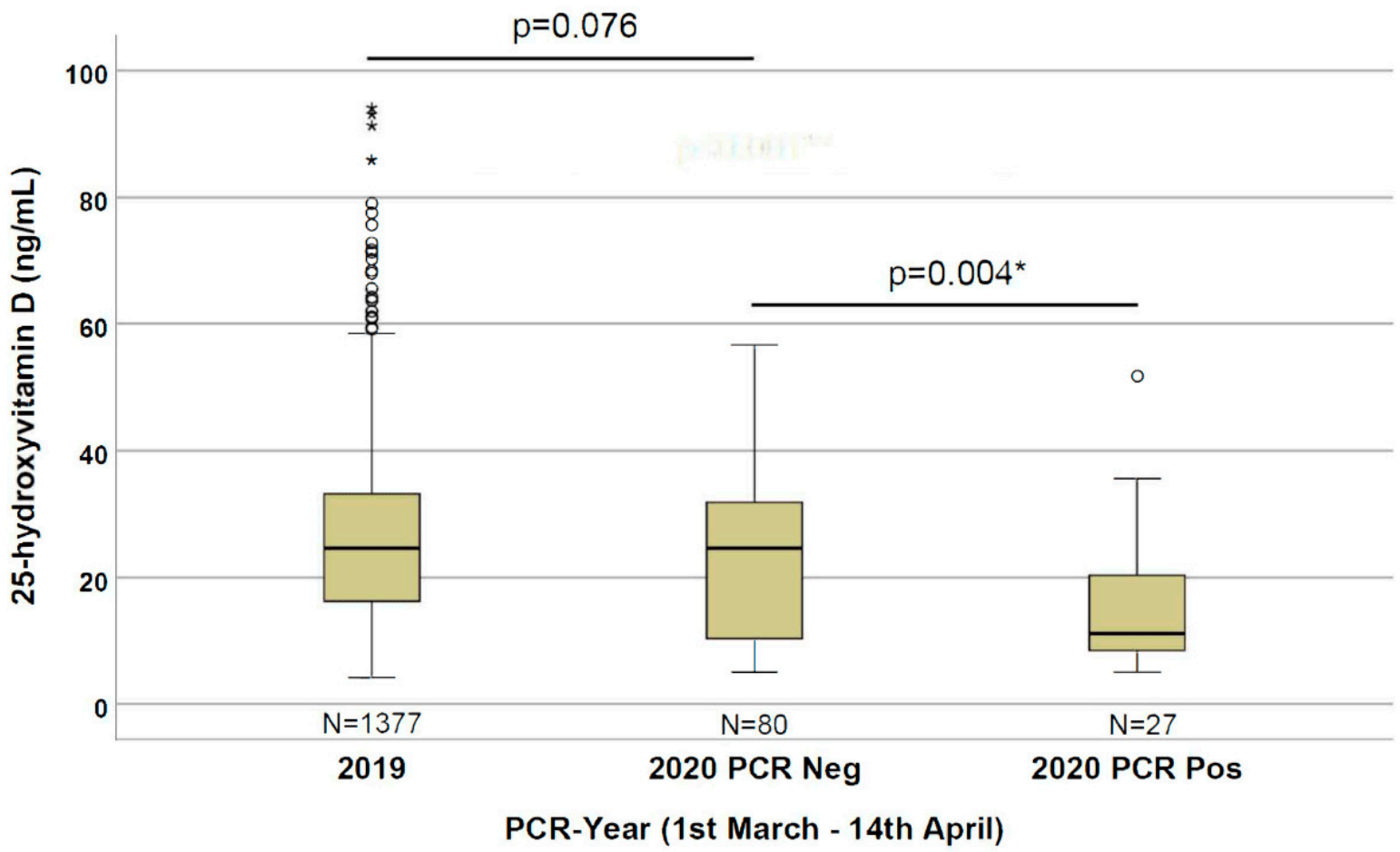 D'Avolio et al., 5/9/2020, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |
| Levels | Marik et al., Med Drug Discov., doi:10.1016/j.medidd.2020.100041 (Preprint) | Does vitamin D status impact mortality from SARS-CoV-2 infection? |
| Details Analysis of case fatality rates showing that the CFR was significantly greater for Northern states (>40° latitude) compared to Southern States (6.0% vs. 3.5%, p < 0 .001), although there were some exceptions with individual states. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Marik et al., Med Drug Discov., doi:10.1016/j.medidd.2020.100041 (Preprint) |
| Does vitamin D status impact mortality from SARS-CoV-2 infection? |
| Analysis of case fatality rates showing that the CFR was significantly greater for Northern states (>40° latitude) compared to Southern States (6.0% vs. 3.5%, p < 0 .001), although there were some exceptions with individual states. Marik et al., 4/28/2020, preprint, 3 authors. |
| Submit Corrections or Comments |
| Levels | Lau et al., medRxiv, doi:10.1101/2020.04.24.20075838 (Preprint) | ICU, ↓45.0%, p=0.29 | Vitamin D Insufficiency is Prevalent in Severe COVID-19 |
| Details Analysis of 20 hospitalized COVID-19 patients, 13 requiring ICU admission. 84.6% of the ICU patients had low vitamin D levels versus 57.1% of the non-ICU patients. |
| Details Source PDF Levels Analysis of outcomes based on serum levels |
| Lau et al., medRxiv, doi:10.1101/2020.04.24.20075838 (Preprint) |
| Vitamin D Insufficiency is Prevalent in Severe COVID-19 |
Analysis of 20 hospitalized COVID-19 patients, 13 requiring ICU admission. 84.6% of the ICU patients had low vitamin D levels versus 57.1% of the non-ICU patients. risk of ICU admission, 45.0% lower, RR 0.55, p = 0.29, high D levels 2 of 5 (40.0%), low D levels 11 of 15 (73.3%), >30ng/mL. Lau et al., 4/28/2020, retrospective, USA, North America, preprint, 7 authors. |
| Submit Corrections or Comments |
| Review | Grant et al., Nutrients, 12:4, 988, doi:10.3390/nu12040988 (Review) (Peer Reviewed) | review | Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths |
| Details Review of the evidence that vitamin D supplementation could reduce COVID-19 risk. |
| Details Source PDF Review Review |
| Grant et al., Nutrients, 12:4, 988, doi:10.3390/nu12040988 (Review) (Peer Reviewed) |
| Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths |
| Review of the evidence that vitamin D supplementation could reduce COVID-19 risk. Grant et al., 4/2/2020, peer-reviewed, 7 authors. |
| Submit Corrections or Comments |
| Review | McCullough et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.12.010 (Review) (Peer Reviewed) | review | Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience |
| Details Report on the long-term use of vitamin D in hospitalized patients with daily dosing from 5,000 to 50,000IU over 7 years. There were no cases of hypercalcemia or any adverse events related to vitamin D supplementation. Authors conclude tha.. |
| Details Source PDF Review Review |
| McCullough et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.12.010 (Review) (Peer Reviewed) |
| Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience |
| Report on the long-term use of vitamin D in hospitalized patients with daily dosing from 5,000 to 50,000IU over 7 years. There were no cases of hypercalcemia or any adverse events related to vitamin D supplementation. Authors conclude that long-term supplementation with vitamin D3 in doses ranging from 5,000 to 50,000 IUs/day appears to be safe. McCullough et al., 1/1/2019, peer-reviewed, 3 authors. |
| Submit Corrections or Comments |
| N/A | Martineau et al., BMJ 2017, 356, doi:10.1136/bmj.i6583 (Peer Reviewed) (meta analysis) | cases, ↓7.3%, p=0.003 | Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data |
| Details Meta analysis of 25 RCTs showing vitamin D supplementation was safe and it protected against acute respiratory tract infection overall. Patients who were very vitamin D deficient and those not receiving bolus doses experienced the most be.. |
| Details Source PDF N/A N/A |
| Martineau et al., BMJ 2017, 356, doi:10.1136/bmj.i6583 (Peer Reviewed) (meta analysis) |
| Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data |
Meta analysis of 25 RCTs showing vitamin D supplementation was safe and it protected against acute respiratory tract infection overall. Patients who were very vitamin D deficient and those not receiving bolus doses experienced the most benefit.Vitamin D supplementation reduced the risk of acute respiratory tract infection among all participants (adjusted odds ratio aOR 0.88 [0.81-0.96], p=0.003.In subgroup analysis, protective effects were seen in those receiving daily or weekly vitamin D without additional bolus doses (aOR 0.81 [0.72-0.91]) but not in those receiving one or more bolus doses (aOR 0.97 [0.86-1.10]). Among those receiving daily or weekly vitamin D, protective effects were stronger in those with baseline 25-hydroxyvitamin D levels <25 nmol/L (aOR 0.30 [0.17-0.53]) than in those with baseline 25-hydroxyvitamin D levels ≥25 nmol/L (aOR 0.75 [0.60-0.95]). risk of case, 7.3% lower, RR 0.93, p = 0.003, OR converted to RR. Martineau et al., 1/1/2017, peer-reviewed, 25 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Quraishi et al., JAMA Surgery, doi:10.1001/jamasurg.2013.3176 (Peer Reviewed) | Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery |
| Details Retrospective 770 gastric bypass surgery patients showing a strong relationship between pre-operative vitamin D levels and the risk of hospital acquired infections. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Quraishi et al., JAMA Surgery, doi:10.1001/jamasurg.2013.3176 (Peer Reviewed) |
| Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery |
Retrospective 770 gastric bypass surgery patients showing a strong relationship between pre-operative vitamin D levels and the risk of hospital acquired infections. 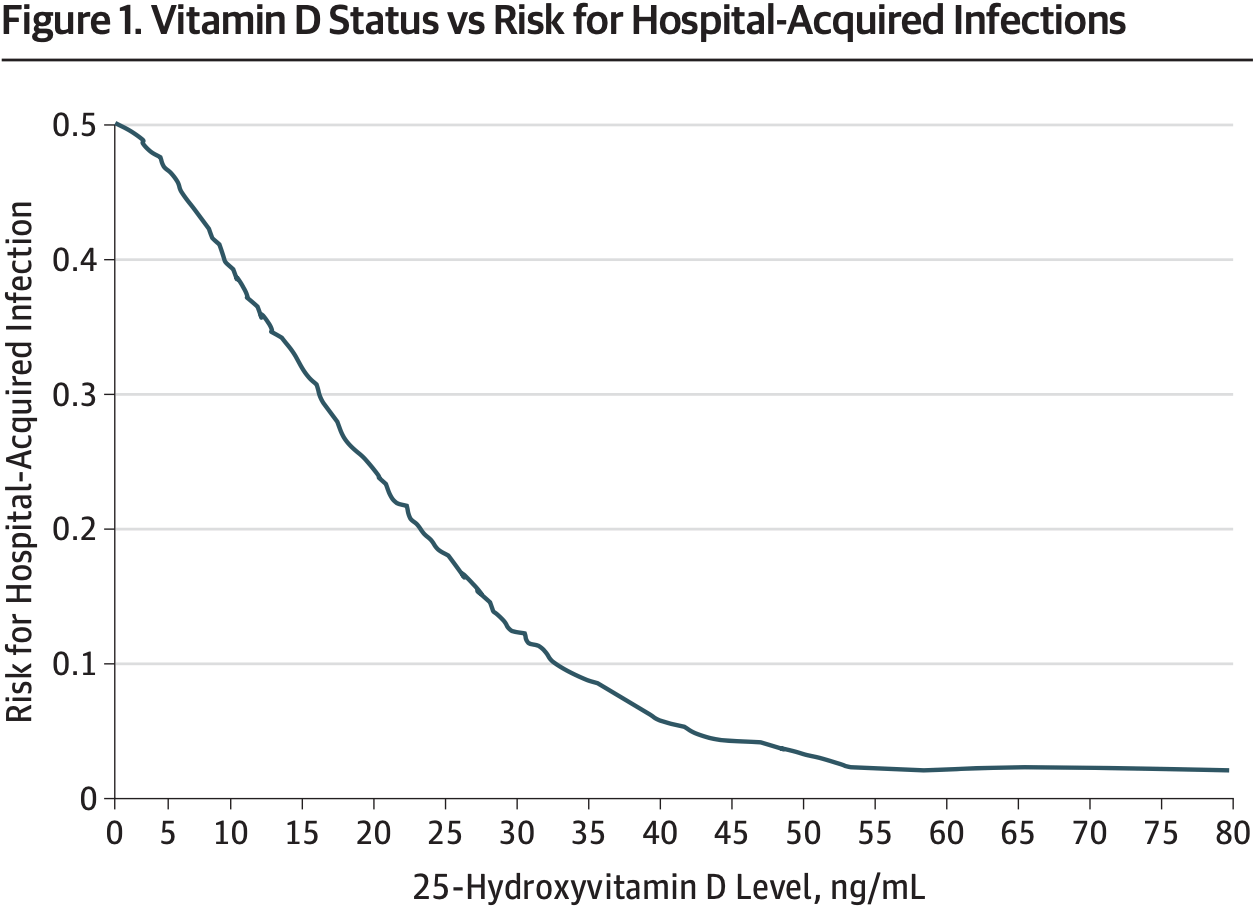 Quraishi et al., 1/1/2013, peer-reviewed, 5 authors. |
| Submit Corrections or Comments |
| N/A | Bergman et al., PLoS ONE, 2013, 8:6, doi:10.1371/journal.pone.0065835 (Peer Reviewed) (meta analysis) | meta-analysis | Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| Details Meta analysis of 11 placebo-controlled studies of 5660 patients. Vitamin D showed a protective effect against RTI (OR 0.64 [0.49-0.84]). The protective effect was larger in studies using once-daily dosing compared to bolus doses (OR = 0... |
| Details Source PDF N/A N/A |
| Bergman et al., PLoS ONE, 2013, 8:6, doi:10.1371/journal.pone.0065835 (Peer Reviewed) (meta analysis) |
| Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| Meta analysis of 11 placebo-controlled studies of 5660 patients. Vitamin D showed a protective effect against RTI (OR 0.64 [0.49-0.84]).The protective effect was larger in studies using once-daily dosing compared to bolus doses (OR = 0.51 vs OR = 0.86, p = 0.01). There was some evidence that results may have been influenced by publication bias. Bergman et al., 1/1/2013, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| Review | Palacios et al., J Steroid Biochem Mol Biol., 2014, 144PA, 138–145, doi:10.1016/j.jsbmb.2013.11.003 (Review) (Peer Reviewed) | review | Is vitamin D deficiency a major global public health problem? |
| Details Review showing vitamin D deficiency is common worldwide in all age groups. |
| Details Source PDF Review Review |
| Palacios et al., J Steroid Biochem Mol Biol., 2014, 144PA, 138–145, doi:10.1016/j.jsbmb.2013.11.003 (Review) (Peer Reviewed) |
| Is vitamin D deficiency a major global public health problem? |
Review showing vitamin D deficiency is common worldwide in all age groups. 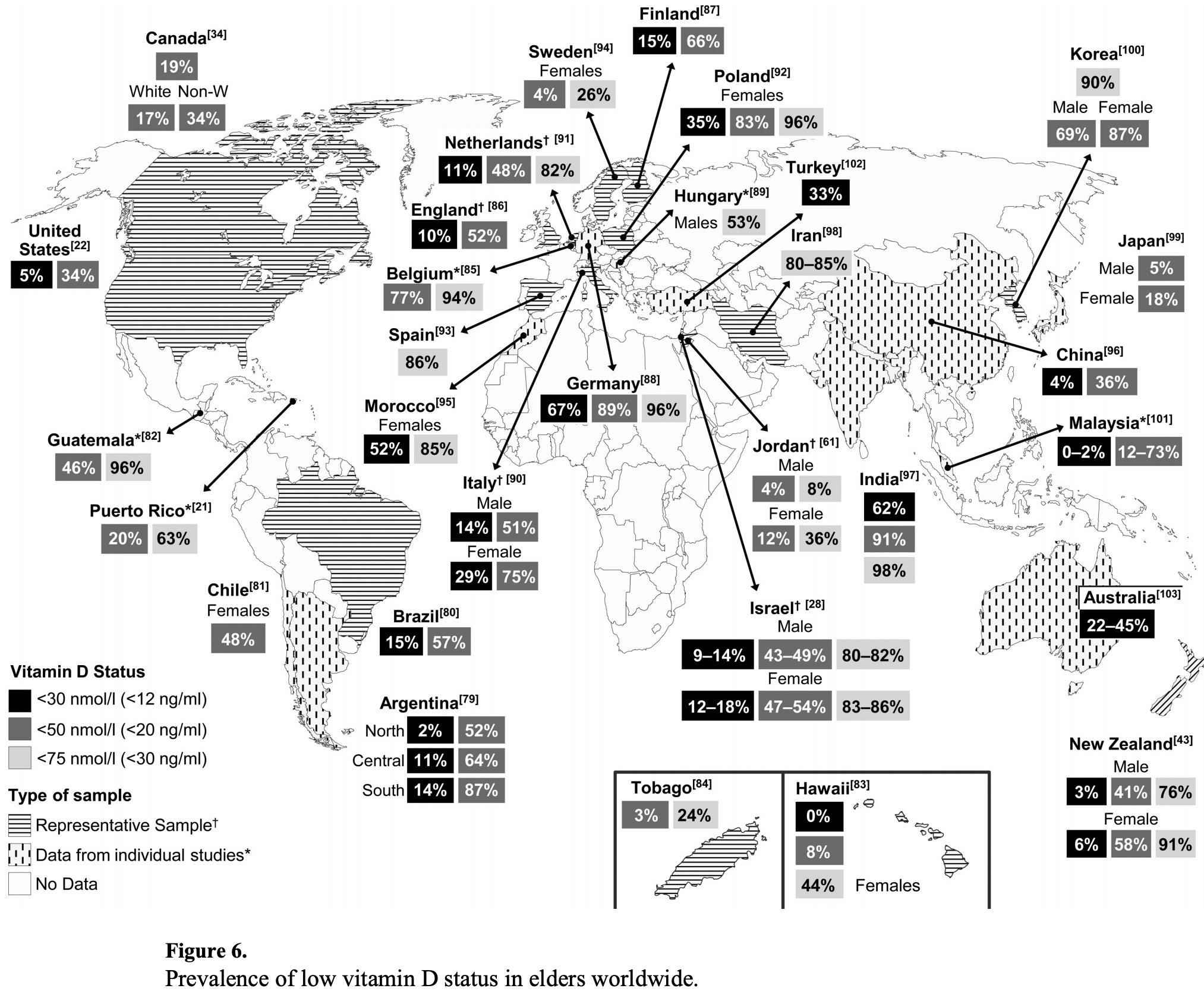 Palacios et al., 1/1/2012, peer-reviewed, 2 authors. |
| Submit Corrections or Comments |
| Related | Mitchell et al., Endocr. Pract., 2012, 18:6, 914–923, doi:10.4158/EP12072.OR (Peer Reviewed) (Related) | Prevalence and predictors of vitamin D deficiency in healthy adults |
| Details Study of 634 healthy volunteers showing 64% had 25(OH)D ≤ 30 ng/mL. Gender, ethnicity, and multivitamin use were significantly associated with 25(OH)D levels. |
| Details Source PDF Related Related |
| Mitchell et al., Endocr. Pract., 2012, 18:6, 914–923, doi:10.4158/EP12072.OR (Peer Reviewed) (Related) |
| Prevalence and predictors of vitamin D deficiency in healthy adults |
Study of 634 healthy volunteers showing 64% had 25(OH)D ≤ 30 ng/mL. Gender, ethnicity, and multivitamin use were significantly associated with 25(OH)D levels. 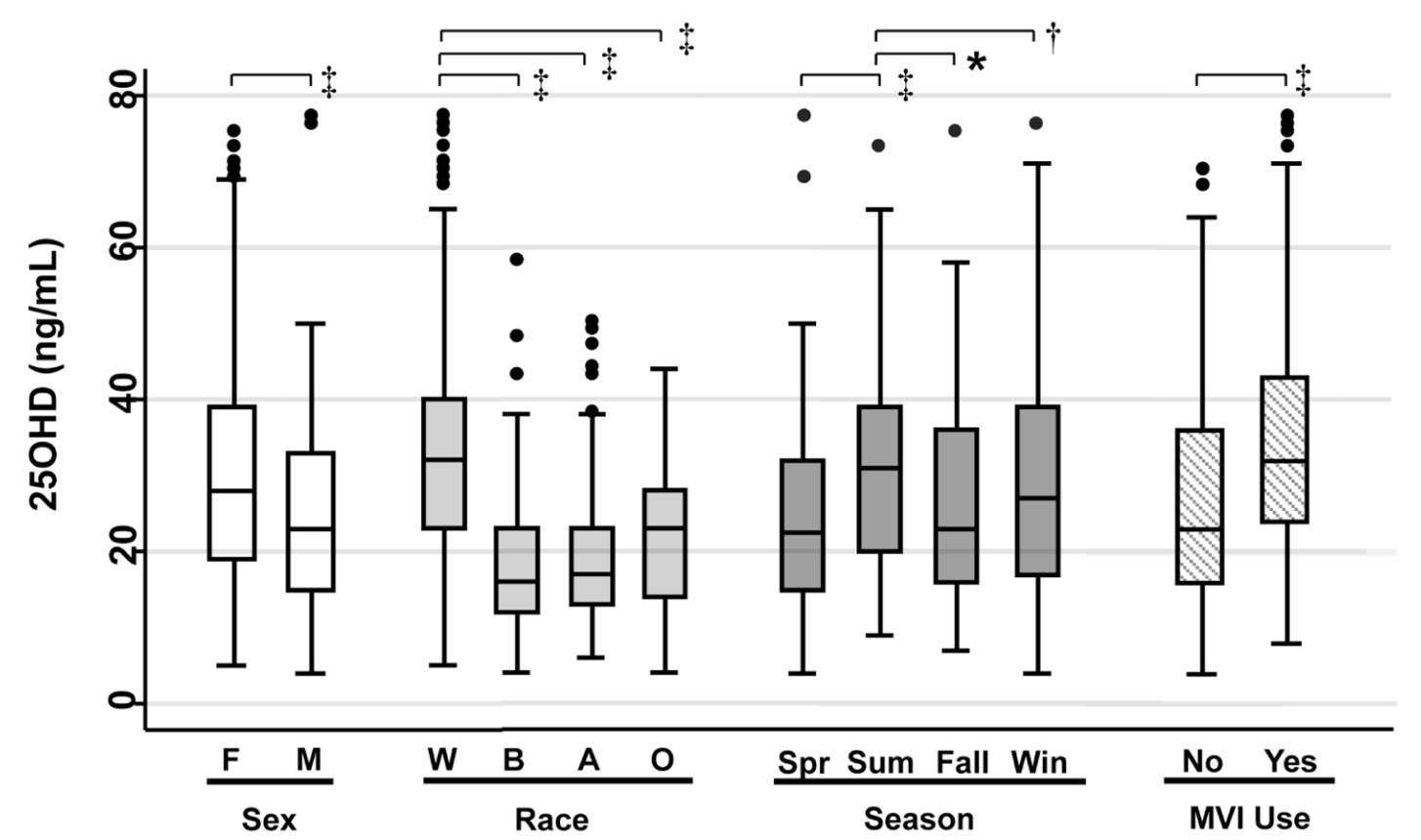 Mitchell et al., 1/1/2012, peer-reviewed, 4 authors. |
| Submit Corrections or Comments |
| PrEPPEP | Urashima et al., Am. J. Clin. Nutr. 2010, 91:5, 1255-60, doi:10.3945/ajcn.2009.29094 (Peer Reviewed) | Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren |
| Details RCT for vitamin D supplementation and seasonal influenza A in schoolchildren, showing 10.8% incidence in children in the vitamin D3 group compared with 18.6% in the placebo group, relative risk RR 0.58 [0.34-0.99], p = 0.04. The reductio.. |
| Details Source PDF Prophylaxis study Prophylaxis study |
| Urashima et al., Am. J. Clin. Nutr. 2010, 91:5, 1255-60, doi:10.3945/ajcn.2009.29094 (Peer Reviewed) |
| Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren |
RCT for vitamin D supplementation and seasonal influenza A in schoolchildren, showing 10.8% incidence in children in the vitamin D3 group compared with 18.6% in the placebo group, relative risk RR 0.58 [0.34-0.99], p = 0.04.The reduction was more prominent in children who had not been taking other vitamin D supplements. RR 0.36 [0.17-0.79], p 0.006, and who started nursery school after age 3y, RR 0.36 [0.17-0.78], p = 0.005.Reduced incidence of influenza B was not seen, RR 1.39 [0.90-2.15], p = 0.13. 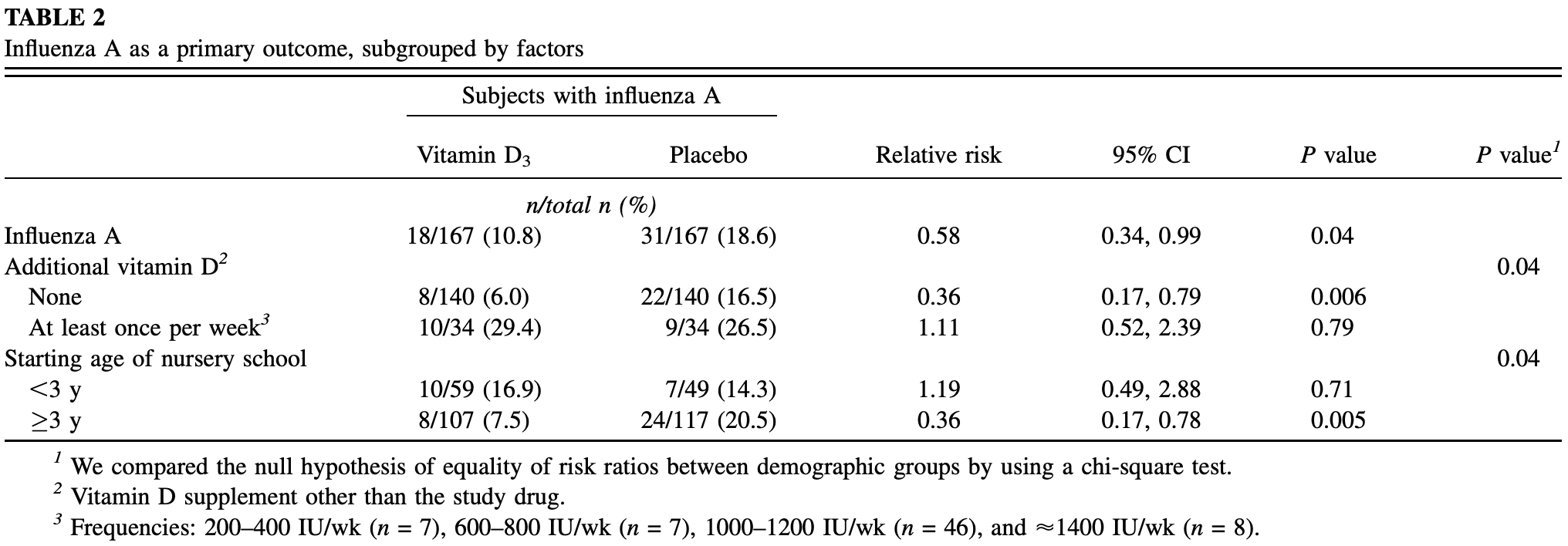 Urashima et al., 1/1/2010, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| N/A | Carlberg et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.01.002 (Peer Reviewed) | In vivo response of the human epigenome to vitamin D: A Proof-of-principle study |
| Details Epigenome-wide chromatin accessibility study before and after vitamin D supplementation (calcitriol), showing significant changes at hundreds of sites within the epigenome of human leukocytes (part of the immune system). |
| Details Source PDF N/A N/A |
| Carlberg et al., The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.01.002 (Peer Reviewed) |
| In vivo response of the human epigenome to vitamin D: A Proof-of-principle study |
Epigenome-wide chromatin accessibility study before and after vitamin D supplementation (calcitriol), showing significant changes at hundreds of sites within the epigenome of human leukocytes (part of the immune system). 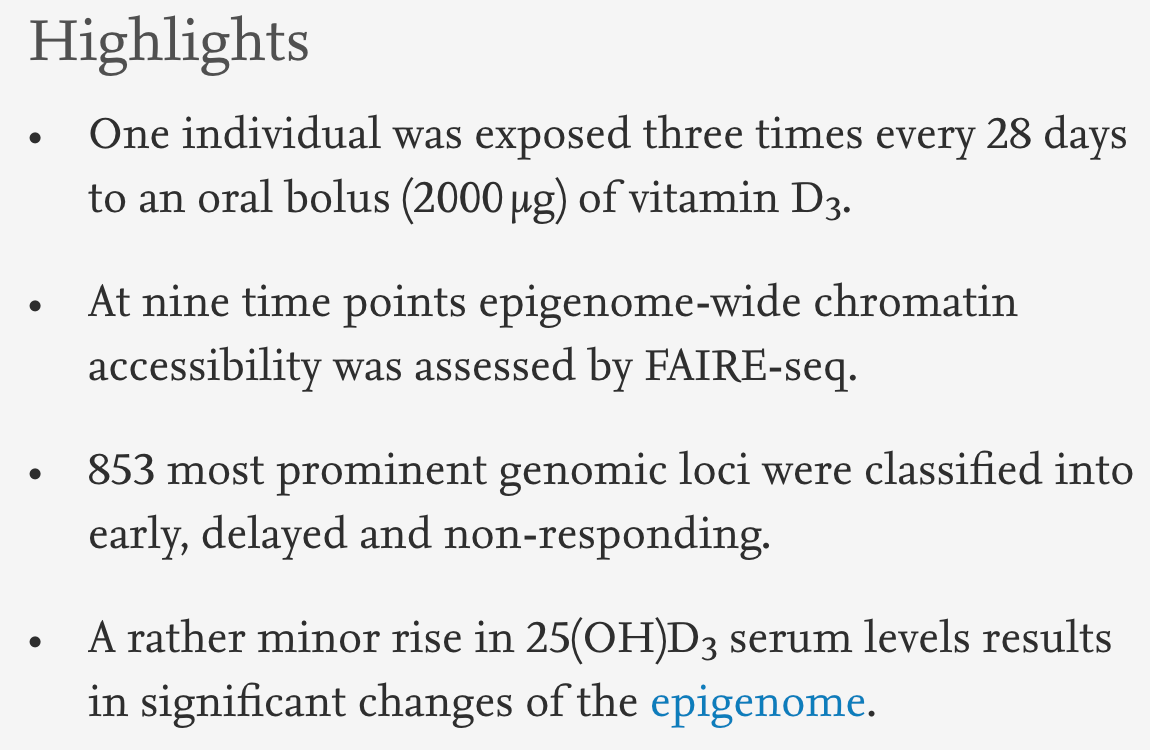 Carlberg et al., 1/1/2008, peer-reviewed, 6 authors. |
| Submit Corrections or Comments |
| Review | Cannell et al., Epidemiol Infect., 2006, 134:6. 1129-40, doi:10.1017/S0950268806007175 (Review) (Peer Reviewed) | review | Epidemic influenza and vitamin D |
| Details Review article on the mechanisms of action and seasonality of vitamin D levels, concluding that varying vitamin D levels may be the reason for the seasonality of epidemic influenza. |
| Details Source PDF Review Review |
| Cannell et al., Epidemiol Infect., 2006, 134:6. 1129-40, doi:10.1017/S0950268806007175 (Review) (Peer Reviewed) |
| Epidemic influenza and vitamin D |
Review article on the mechanisms of action and seasonality of vitamin D levels, concluding that varying vitamin D levels may be the reason for the seasonality of epidemic influenza. 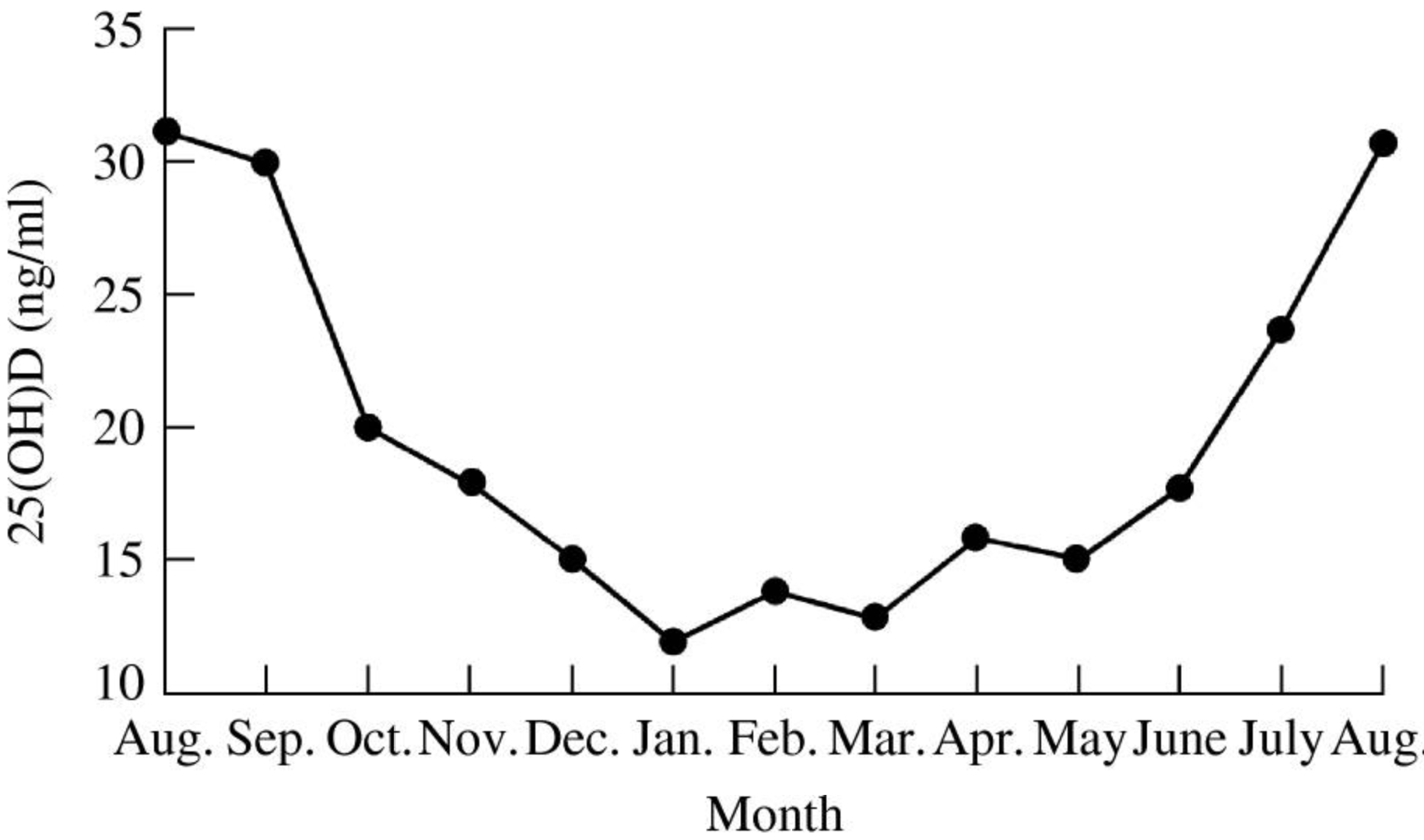 Cannell et al., 1/1/2006, peer-reviewed, 8 authors. |
| Submit Corrections or Comments |

































































































































































































0 komentar:
Posting Komentar